Published online Nov 10, 2018. doi: 10.5306/wjco.v9.i7.162
Peer-review started: July 6, 2018
First decision: August 21, 2018
Revised: August 12, 2018
Accepted: October 23, 2018
Article in press: October 23, 2018
Published online: November 10, 2018
A 42-years-old lady, presented with a large retroperitoneal mass which was preoperatively diagnosed as a retroperitoneal liposarcoma following an image guided core biopsy. She underwent a margin-negative resection of the retroperitoneal mass (multi visceral resection - enbloc excision of the retroperitoneal mass with a left nephrectomy and a segmental descending colectomy). The final histopathological examination of the resected specimen confirmed an exophytic renal angiomyolipoma (AML) which was extending into the retroperitoneum. AML is a rare benign tumor arising most commonly from the kidney. It can sometimes present as a diagnostic challenge as it mimics a retroperitoneal liposarcoma or a fat-containing renal cell carcinomas closely. We present this case to share our experience of managing a case of giant exophytic AML which resembled retroperitoneal liposarcoma closely and resulted into an aggressive surgery.
Core tip: A giant exophytic renal angiomyolipoma (AML) can pose a serious diagnostic challenge and may be confused with a retroperitoneal sarcoma. A discordance of the radiological and core biopsy findings in a suspected case of an exophytic renal AML must lead to re-evaluation of the case and repeat biopsies may further clarify the diagnosis.
- Citation: Sharma G, Jain A, Sharma P, Sharma S, Rathi V, Garg PK. Giant exophytic renal angiomyolipoma masquerading as a retroperitoneal liposarcoma: A case report and review of literature. World J Clin Oncol 2018; 9(7): 162-166
- URL: https://www.wjgnet.com/2218-4333/full/v9/i7/162.htm
- DOI: https://dx.doi.org/10.5306/wjco.v9.i7.162
Angiomyolipoma (AML) is a benign tumor primarily containing fat, atypical blood vessels and smooth muscles in varying proportions[1]. The common site of AML is kidney and it presents primarily as an intra-renal mass. Occasionally, a renal AML may outgrow exophytically in the retroperitoneum and closely mimics a liposarcoma due to the high fat content on a radiological imaging. The diagnostic dilemma is further compounded as the core-cut biopsy may also be erroneously reported as liposarcoma[2].This may result in an aggressive surgery, and at times multi-visceral resections, to achieve a margin-negative resection. A post-resection histopathological diagnosis of AML may come as a surprise for both the surgeons and the patients, and may even lead to litigations. We are reporting a case of a giant exophytic AML which was misdiagnosed preoperatively as a retroperitoneal liposarcoma following an image guided core biopsy examination.
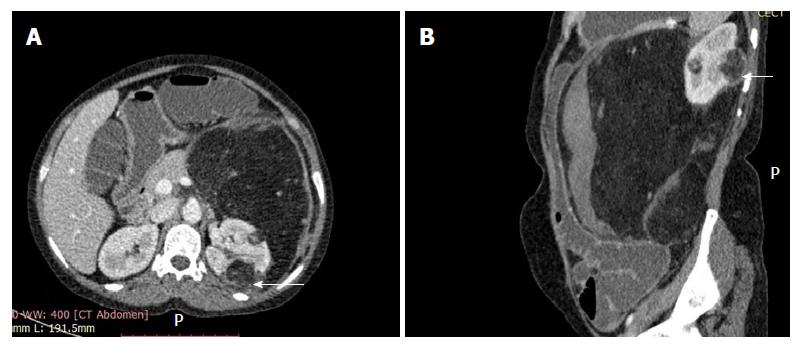
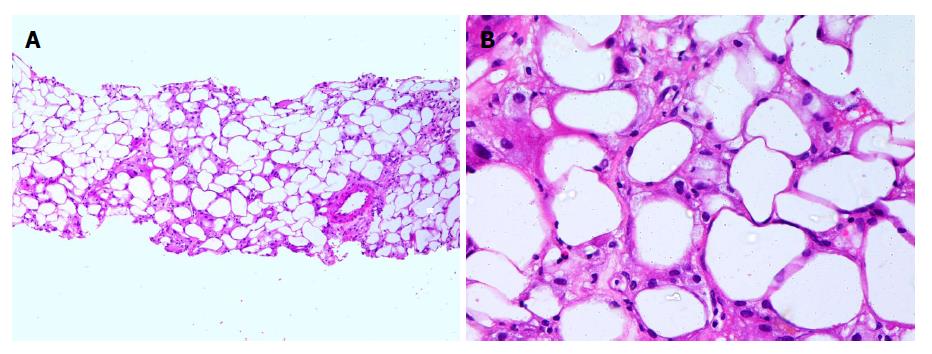
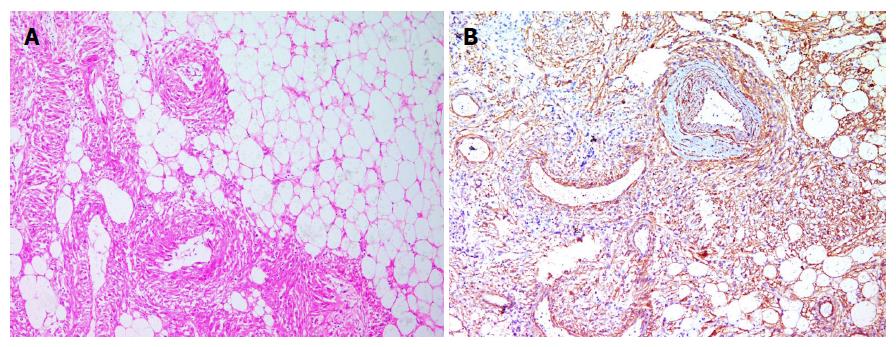
A 42-years-old lady presented to us with complaints of abdominal pain and fullness over the left side of the abdomen for two months duration. The pain was mild, dull aching, localized and continuous with a gradual increase in intensity over a period of time. She denied having hematuria, flank pain, dysuria, anorexia, rectal bleeding, malena or vaginal bleeding. She also denied any previous history of fever or blood transfusion. She reported to had undergone bilateral salpingo-oophorectomy around 3 years back for a left adnexal mass; no medical documents were available for this surgery. She developed amenorrhea following bilateral salpingo-oopherectomy, and she was not taking hormone replacement therapy. She also did not report any other significant past medical or family history. She had three children; all were borne as normal vaginal delivery and were hale and hearty. Her general physical examination was unremarkable. Her body mass index was 27.5. Her abdominal examination revealed a firm, non-tender, immobile, bimanually palpable intra-abdominal lump of size 25 × 20 cm involving left hypochondrium, left lumbar, umbilical, and left iliac fossa. Rest of her physical examination was unremarkable. Her blood investigations showed a hemoglobin of 6.6 g/dL and a total leucocyte count of 12000/μL. Her platelet count, liver function tests and renal function tests were within normal limits. Her contrast-enhanced computed tomography (CT) of the abdomen suggested two fairly well defined, predominantly fat density rounded lesions in the left kidney. The peripheral capsule of the smaller lesion was ill defined and was continuous with a large perirenal mass showing prominent vessels (Figure 1). There was also a peripheral hematoma in the perirenal lipomatous mass. An ultrasonography guided core biopsy of the retroperitoneal mass suggested liposarcoma in view of the variable sized adipocytes with atypia (Figure 2). Surgical exploration revealed a large retroperitoneal mass involving the left kidney and a segment of descending colon. The patient underwent a margin-negative resection of the retroperitoneal mass (multi visceral resection - enbloc excision of the retroperitoneal mass with a left nephrectomy and a segmental descending colectomy). Figure 3 displays the resected specimen. Her postoperative period was uneventful. Final histopathological examination of the resected specimen confirmed an exophytic renal AML which was extending into the retroperitoneum (Figure 4). A retrospective evaluation of the patient did not reveal any clinical stigmata of neurofibromatosis.
AML is a rare benign tumor which has a tri-phasic morphology - blood vessels, smooth muscles, and fat cells. Based on the fat content, AML is typically divided into classical or fat-rich type, and fat-poor AML. Both of these types are benign tumors with no metastatic potential. A third rare type is an epithelioid AML which is rare but has a malignant potential. Though fat-poor AML poses a diagnostic challenge due to the presence of scattered fat cells in the smooth muscles, classical renal AML can be easily diagnosed based on the contrast enhancement CT features: (A) the demonstration of the fat cells as the presence of regions of interest containing attenuations less than < 10-20 HU; and (B) the location of the fat cells within the lesion and not in another structure near it[3]. However, one must not forget that there are other kinds of lesions which may contain fat and mimic AML.
When this fat-rich renal AML grows exophytically and extends into the retroperitoneum, it becomes difficult to differentiate it from a retroperitoneal sarcoma, especially a liposarcoma. As the management strategies are entirely different from these two entities - wide margin-negative resection for liposarcoma vs conservative approach for AML, it is of utmost importance to differentiate them radiologically. In a retrospective study of CT images of 15 large exophytic renal AMLs and 12 well-differentiated perirenal liposarcomas, Israel et al[4] suggested that a defect in the renal parenchyma combined with the presence of the enlarged vessels may help differentiate an exophytic AML from a retroperitoneal sarcoma. In a study of 11 patients with the perirenal liposarcoma and 9 patients with the giant exophytic AMLs, Ellingson et al[5] also concluded that the presence of tumoral vessel extending into the renal cortex or a renal parenchyma defect at the site of the tumor contact points strongly towards the diagnosis of AML while intra-tumoral calcification favors the presence of liposarcoma. However, Wang et al[6] suggested that the intra-tumoral calcification can be seen in both AML and liposarcoma. They highlighted that the characteristics of a perinephric AML are intratumoral linear vascularity, aneurysmal dilatation, bridging vessel sign, hematoma, beak sign, and discrete intra-renal fatty tumors while the CT characteristics of a perinephric liposarcoma are a non-fatty soft tissue mass. Other close differentials of an exophytic AML include lipoma, leiomyoma with fatty change or a fat containing renal cell carcinoma.
A small biopsy of the lesion to confirm the diagnosis may also yield erroneous results due to the non-representative sample in view of the heterogenous nature of the AML[5]. A positive immune-reactivity for human melanoma black 45, is characteristic of AMLs and may differentiate AMLs from other similar appearing lesions such as liposarcomas, lipomas, leiomyosarcomas or, leiomyomas[7].
Our patient had a giant symptomatic exophytic AML. Though radiological findings were suggestive of AML, our patient was operated upon with a preoperative diagnosis of retroperitoneal liposarcoma due to the small image-guided biopsy which was reported as liposarcoma. This is likely to be due to a non-representative sample of the lesion. Though various conservative approaches including radiofrequency ablation, cryoablation, microwave ablation, selective angio-embolization are described to manage AML[8], our patient would have otherwise also required surgical excision in view of the large size, the symptomatic nature, and the risk of potential life-threatening hemorrhage. However, a correct preoperative diagnosis would have helped us to take a more conservative resection.
We conclude that a giant exophytic renal AML can pose a serious diagnostic challenge and may be confused with a retroperitoneal liposarcoma. A discordance of the radiological and core biopsy findings in a suspected case of exophytic renal AML must lead to re-evaluation of the case and repeat biopsies may further clarify the diagnosis.
A 42-years-old lady came to our hospital with complaints of abdominal pain and distension of two months duration. The physical examination of the patient revealed large retroperitoneal lump present on the left side of the abdomen.
The clinical diagnosis was a retroperitoneal mass, likely to be malignant in nature.
The differential diagnosis included retroperitoneal sarcoma, renal neoplasm, multicystic kidney, cold abscess, or hydatid cyst.
Routine blood investigations did not reveal any abnormality.
Abdominal computed tomography revealed a large perirenal mass lesion displaying prominent vessels. There were also two fairly well defined, predominantly fat density rounded lesions in the left kidney; the smaller lesion was continuous with the large perirenal mass.
Preoperative image guided biopsy of the retroperitoneal mass suggested liposarcoma.
In view of preoperative pathological diagnosis of liposarcoma, the patient underwent a margin-negative resection of the retroperitoneal mass (multi visceral resection - enbloc excision of retroperitoneal mass with left nephrectomy and segmental descending colectomy).
The final histopathological report of the resected specimen confirmed angiomyolipoma.
AML is a tumor of tri-phasic morphology - blood vessels, smooth muscles, and fat cells. Majority of the AML tumors are benign in nature with almost no malignant potential.
A large exophytic renal AML may be confused with a retroperitoneal sarcoma on a small biopsy specimen. A discordance of the radiological and core biopsy findings in a suspected case of exophytic renal AML must alert the surgeon and a re-evaluation of the case with repeat biopsies may clarify the diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
CARE Checklist (2013) statement: This manuscript has completed the CARE Checklist (2013).
P- Reviewer: Vikey AK, Sukocheva OA, Yang T, Gadbail AR S- Editor: Dou Y L- Editor: A E- Editor: Bian YN
| 1. | Garg PK, Jain BK, Kumar A, Bhatt S, Vibhav V. Fat poor angiomyolipoma with lymphadenopathy: Diagnostic dilemma. Urol Ann. 2012;4:126-129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Kori C, Akhtar N, Vamsidhar PN, Gupta S, Kumar V. Giant exophytic renal angiomyolipoma mimicking as retroperitoneal sarcoma; a case report with review of literature. J Clin Diagn Res. 2015;9:XJ01-XJ02. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Jinzaki M, Silverman SG, Akita H, Mikami S, Oya M. Diagnosis of Renal Angiomyolipomas: Classic, Fat-Poor, and Epithelioid Types. Semin Ultrasound CT MR. 2017;38:37-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Israel GM, Bosniak MA, Slywotzky CM, Rosen RJ. CT differentiation of large exophytic renal angiomyolipomas and perirenal liposarcomas. AJR Am J Roentgenol. 2002;179:769-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 93] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Ellingson JJ, Coakley FV, Joe BN, Qayyum A, Westphalen AC, Yeh BM. Computed tomographic distinction of perirenal liposarcoma from exophytic angiomyolipoma: a feature analysis study. J Comput Assist Tomogr. 2008;32:548-552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Wang LJ, Wong YC, Chen CJ, See LC. Computerized tomography characteristics that differentiate angiomyolipomas from liposarcomas in the perinephric space. J Urol. 2002;167:490-493. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Minja EJ, Pellerin M, Saviano N, Chamberlain RS. Retroperitoneal extrarenal angiomyolipomas: an evidence-based approach to a rare clinical entity. Case Rep Nephrol. 2012;2012:374107. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Jawahar A, Kazan-Tannus J. Retroperitoneal extrarenal angiomyolipoma at the surgical bed 8 years after a renal angiomyolipoma nephrectomy: A case report and review of literature. Urol Ann. 2017;9:288-292. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |