Published online Apr 10, 2017. doi: 10.5306/wjco.v8.i2.135
Peer-review started: October 15, 2016
First decision: December 15, 2016
Revised: January 26, 2017
Accepted: February 18, 2017
Article in press: February 20, 2017
Published online: April 10, 2017
Gastrointestinal stromal tumors (GISTs) are rare but most common nonepithelial tumor of gastrointestinal tract. They are often found incidentally on computed tomography and endoscopic investigations. Increasing knowledge of the pathogenesis of GISTs and the advent of tyrosine kinase inhibitors revolutionized the management of GISTs. The newer advanced endoscopic techniques have challenged the conventional surgery although the true efficacy and safety of endoscopic approach is not clear at this time. This review article focuses on pathogenesis, diagnosis and management of GISTs.
Core tip: Gastrointestinal stromal tumors (GISTs) are most common mesenchymal tumors in the gastrointestinal tract. The management of GISTs is revolutionized with the advent of tyrosine kinase inhibitors (TKIs) and newer advanced endoscopic techniques. Accurate identification and differentiation of GISTs from other submucosal tumors is achieved with the help of endoscopic ultrasound. The management of small to medium GISTs are feasible by newer advanced endoscopic and/or laparoscopic techniques. Team approach involving endoscopist, pathologist, radiologist, medical oncologist and surgeon is key in optimal management of GISTs. This article focuses on role of TKIs and endoscopist perspective in the management of GISTs.
- Citation: Lanke G, Lee JH. How best to manage gastrointestinal stromal tumor. World J Clin Oncol 2017; 8(2): 135-144
- URL: https://www.wjgnet.com/2218-4333/full/v8/i2/135.htm
- DOI: https://dx.doi.org/10.5306/wjco.v8.i2.135
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal (sub epithelial) tumor, and are frequently found in stomach and small intestine[1]. GISTS are hypothesized to originate from interstitial cells of cajal (ICC) which coordinate gut motility[2]. GISTs are rarely found in the peritoneum, mesentery and omentum[3]. GISTs have varied malignant potential, with about 40% of GISTs that are localized at initial diagnosis give rise to metastasis[4], and about 10%-20% of GISTs present with distant metastasis[5,6]. In Europe, the annual incidence of GISTs is about 10 cases per million[7]. In the United States, the annual incidence of GIST ranges from 4000 to 6000 new cases per year (7-20 cases per million population per year)[8]. The mean age at diagnosis is 63 years[9]; men and women are equally affected. The majority of GISTs are sporadic and may be associated with mutations like NF1, C-kit, platelet derived growth factor receptor-alpha (PDGFRA), succinate dehydrogenase (SDH) and deletions in chromosome 1 involving SDH c[10].
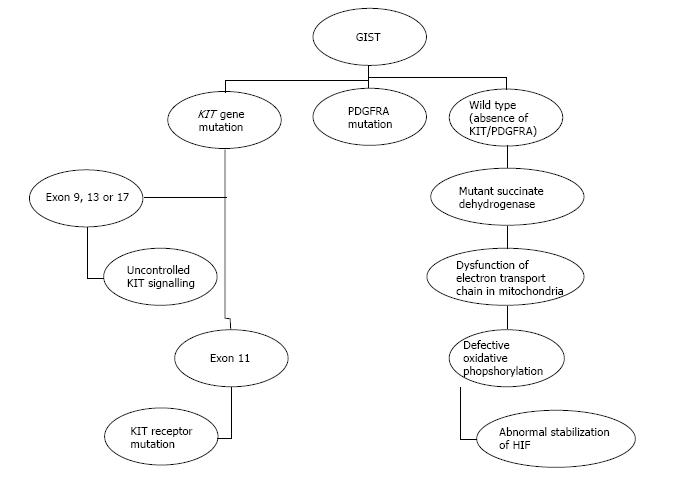
Overall, GISTs are defined by the presence of KIT gene or PDGFRA mutation. Majority (80%) of GISTs have KIT gene mutations and biologic response of KIT receptor is produced without a bound ligand[11]. KIT receptor tyrosine kinase activity in normal cells is regulated by binding of endogenous KIT ligand or stem cell factor (SCF)[12]. In the majority of cases, spontaneous receptor dimerization and activation occurs when exon 11 is affected by KIT gene mutation. However, in few cases, a different mechanism results in uncontrolled KIT signaling if mutation occurs in Exon 9, 13 or 17. In cases with NF1, uncontrolled KIT activation may be present even in the absence of KIT gene mutation (wild type)[13]. A subset of GISTs which are negative for KIT gene mutations are positive for receptor tyrosine kinase PDGFRA mutations. GISTs expressing PDGFRA or KIT gene mutations have similar biologic consequences[14]. About 10% of adult GISTs have neither KIT gene nor PDGFRA mutation[15]. SDH-ubiquinone complex 2 is composed of subunits A, B, C and D which is part of Krebs cycle and respiratory chain[16]. In mutant SDH, dysfunction of electron transport chain in mitochondria leads to defective oxidative phosphorylation, which ultimately leads to abnormal stabilization of hypoxia inducible factors (HIF)[17]. Carney-Stratakis syndrome is caused by germline mutation in SDH subunits B, C or D which leads to GIST and paraganglioma[18].
Histologically GISTs are subdivided in to spindle cell (60%-70%), epithelioid (30%-40%) or both (10%). GISTs with spindle cells are compact, highly cellular, arranged in fascicular or whorled pattern with minimal amount of stroma and contain eosinophilic, basophilic or amphophilic cytoplasm. Epithelioid tumors have abundant cytoplasm which is amphophilic to clear and cellular borders are clearly defined[19]. Antibodies to CD34 and CD117 appear in most GISTs[20]. CD34 is a transmembrane glycoprotein present on vascular endothelium and human hematopoietic progenitor cells[21]. CD34 is expressed in a wide variety of tumors and it is detected in about 50%-80% of GISTs[2,11,20]. CD 117 is expressed in 80%-100% of GISTs and it is not expressed in smooth muscle or neural tumors which helps in distinguishing GISTs from other gastrointestinal mesenchymal tumors[20] (Figure 1).
Clinical manifestations of GISTs are highly variable and it depends on tumor size and location. GISTs are usually asymptomatic and found incidentally by imaging or endoscopy[22]. Symptoms include melena, hematemesis, abdominal pain, discomfort, fullness, early satiety and palpable mass. GISTs in proximal stomach can cause dysphagia and tumors in pylorus can present as gastric outlet obstruction[23]. Rectal GISTs can present with hematochezia[24]. Rarely, they can present as intraperitoneal rupture of large tumor causing hemoperitoneum[25]. GISTs can occur as part of a syndrome; Carneys triad (gastric GIST, pulmonary chondroma, paraganglioma)[26], or neurofibromatosis type 1 (mostly spindle cell GIST)[27]. Overall, about 50% of GISTs have local or distant metastasis at the time of presentation[28], with the liver being the most frequent site of metastasis. Other common sites of metastasis include the bone, peritoneum, retroperitoneum, lung, pleura, and subcutaneous (scar) tissue[29].
Computed tomography (CT) is the primary modality of choice for diagnosing GISTs[30,31]. CT tumor characteristics such as size greater than 10 cm, calcifications, irregular margins, heterogeneous, lobulated, regional lymphadenopathy, ulceration, extraluminal and mesenteric fat infiltration are more likely to be associated with metastasis[29]. CT enterography uses large volumes of oral contrast and it is superior to conventional CT. It has advantage of displaying the entire thickness of the small bowel, better visualization of deep ileal loops without superimposition and evaluation of surrounding mesentery[32]. MRI is more accurate than CT for delineating rectal GISTs and in detecting liver metastasis, hemorrhage and necrosis[33].
Esophagogastroduodenoscopy (EGD) shows most sub epithelial lesions as a bulge with a smooth, intact, normal appearing mucosa in the gastrointestinal tract. Hwang et al[34] did a prospective study and patients were referred for endoscopic ultrasound (EUS) to evaluate sub epithelial masses diagnosed previously by EGD, sigmoidoscopy or colonoscopy. The size of the mass during endoscopic exam was measured by open biopsy forceps for size reference. Results showed endoscopy was 98% sensitive and 64% specific in identifying intramural lesions. Intramural size measurement of endoscopy correlated with EUS (r = 0.88, P < 0.001) but, for extramural lesions, it was suboptimal (r = 0.56)[34]. Overall, the study concluded endoscopy had a high sensitivity but low specificity in identifying the location of sub epithelial lesions and histologic confirmation by EUS-fine-needle aspiration (FNA) should be obtained for masses originating from 3rd (submucosa) and 4th layer (muscularis propria)[34].
Endosonographically GISTs appear as oval or hypoechoic mass arising from the muscularis propria. EUS features suggestive of malignancy include enlarged lymph nodes, size greater than 4 cm, irregular borders and cystic spaces with in the mass[35]. EUS has 92% sensitivity and 100% specificity in differentiating submucosal tumor from extrinsic compression[36]. Chen et al[37], retrospectively evaluated EUS characteristics to predict the malignant potential of GISTs. EUS features of GISTs were compared to National Institutes of Health (NIH) criteria for classification of malignant potential and were divided in to very low/low risk, intermediate/high risk. Results showed that GISTs at high risk for malignancy were associated with EUS characteristics like lesion size (P < 0.0001), cystic change (P = 0.015) and surface ulceration (P = 0.036)[37]. EUS-FNA cannot accurately differentiate benign from malignant GIST due to lack of mitotic activity on smears. The definitive method for assessment of GIST malignant potential requires surgical resection.
Dewitt et al[38] evaluated the diagnostic yield and complications of EUS-Trucut biopsy (EUS-TCB) for gastrointestinal mesenchymal tumor (GIMT). EUS-FNA was performed in 33/38 (87%), and was diagnostic on final cytology in 25/33 (76%) and by FNA-immunochemistry (FNA-IC) in 12/24 (50%). EUS-TCB obtained visible tissue specimen in 37/38 (97%), and diagnostic in the final TCB histology in 30/38 (79%) and TCB-IC in 30/31 (97%)[38]. Overall, the authors concluded that EUS-TCB should be considered as an alternative to EUS-FNA when technically feasible[38].
Na et al[39] evaluated the yield and utility of 19-gauge (G) TCB vs 22-G FNA for diagnosing gastric sub epithelial tumors (SETs). The diagnostic yield of TCB vs FNA were 77.8% vs 38.7% (P < 0.0001). The Accuracy of TCB vs FNA for diagnosing GISTs was 90.9% vs 68.8%; and for non-GIST SETs was 81.1% vs 14.3% respectively. There were 9 technical failures with TCB likely due to stiffness, poor maneuverability of the needle and location of the tumor[39]. The most common procedure associated adverse events were pain, hemorrhage (requiring endoscopic hemostasis) and fever[39]. Procedure related events in TCB vs FNA were [3/90 (3.3%) vs 5/62 (8.1%); P = 0.27] respectively[39].
Positron emission tomography (PET)-CT using 18F-fluorodeoxy glucose (FDG) detects cancer based on changes in tissue metabolism[40,41]. PET-CT is used for initial staging and to monitor disease progression. A baseline 18FDG-PET should be obtained before treatment so that the results can be used to compare with future studies[42]. Liver metastasis from GIST often appear as isodense lesions on CT, but may be detected by PET. Hence PET compliments CT in resolving ambiguity of liver lesions in patients with GISTs[42].
Gayed et al[43] showed that the sensitivity and positive predictive value of 18F-FDG PET were 86% and 98% respectively and it is superior to CT in predicting early response to therapy in recurrent or metastatic GISTs[43]. Yoshikawa et al[40] evaluated the efficacy of PET-CT to predict the malignant potential of GIST. Standardized uptake value maximum (SUVmax) and GIST parameters (Ki-67 labeling index and mitotic index) were compared. SUVmax and Ki67 labeling index were significantly elevated in high risk group when compared to low/intermediate risk group[40]. Tumor response to treatment with imatinib mesylate may be detected by a decrease in CT attenuation units (Hounsfield units, HU)[44]. However, there may be delay in measurement of cellular and macroscopic changes after treatment with imatinib by CT. In contrast, PET using 18F-FDG can detect early effects induced by imatinib and decrease in FDG uptake after the initiation of imatinib treatment indicates good prognosis[45].
The “Response Evaluation Criteria in Solid Tumors” (RECIST) classification was previously used, however, due to limitations in assessing malignant response to immunotherapy such as imatinib, RECIST has been replaced by the Choi criteria[46]. Limitations of RECIST were primarily because the response to therapy can occur not only in tumor size but also in structure like decreased tumor density and enhancement of intratumoral nodules[31,47]. The Choi criteria of contrast-enhanced CT is based on decrease in tumor size by 10% in any dimension or decrease in structure by 15%, and was found to be more predictive of time to tumor progression (TTP) than RECIST[48].
Mitotic index, tumor size, location (gastric vs non-gastric) and tumor rupture are independent risk factors for GIST metastases[4]. Joensuu et al[49] analyzed the association between KIT and PDGFRA mutation and RFS in GIST patients treated with surgery alone. The authors concluded that tumor mutation status should not be interpreted in isolation from other risk factors[49]. The American College of Surgeons Oncology trial (ACOSOG) Z90001 study found that tumor size, location and mitotic rate were important in RFS but not tumor mutation status[50]. Gold et al[51] developed a nomogram by calculating concordance probabilities and by comparing three commonly employed staging systems NIH-Miettinen[52], NIH-Fletcher[53] and Armed Forces Institute of Pathology (AFIP)-Miettinen[54]. The investigators concluded that the nomogram can accurately predict RFS after the resection of localized, primary GIST[51].
Surgery is the treatment of choice for primary and localized GISTs[55]. The goal of surgery is complete tumor resection (negative microscopic and macroscopic margins) with functional preservation (often accomplished by wedge resection), while avoiding tumor rupture and injury to the pseudo capsule[55]. McCarter et al[56] analyzed factors associated with R0 (grossly and histologically negative margin), R1 (grossly negative but histologically positive margins), R2 resection (grossly positive margins) and assessed the risk of recurrence with and without imatinib[56]. Factors associated with R1 resection included tumor size (> or = 10 cm), tumor rupture and location[56]. The authors concluded there was no significant difference in recurrence free survival (RFS) in patients who underwent R1vs R0 resection of GIST with or without adjuvant imatinib[56]. Although the management of R1 resection after complete resection is not clear, options include careful observation (watchful waiting), re-excision and adjuvant imatinib treatment.
Laparoscopic wedge resection (LWR) is recommended for gastric GIST smaller than 5 cm. To prevent tumor seeding in laparoscopy, plastic bag is recommended to collect the tumor sample and direct handling of tumor with forceps is contraindicated. Wedge resection of gastric GIST is considered standard treatment[57] and lymphadenectomy is not indicated as nodal metastasis is rare[28]. LWR has the advantage of early resumption of diet, early return of bowel function, shorter hospital stay and decreased duration of parenteral or epidural analgesia[58]. Lee et al[59] study concluded that LWR can be safely performed and have better outcome in terms of recovery after surgery regardless of tumor size and location. Kim et al[60] study concluded that LWR is safe and feasible for small to medium sized gastroduodenal tumors irrespective of location in cardia or pylorus. However, they recommended careful consideration of direction of stapling for exogastric resection of submucosal tumors located in antrum, lesser curvature and pylorus to prevent gastric outlet obstruction.
Endoscopic enucleation and other related procedures are more feasible for GISTs less than 5 cm[61]. Complete resection of GIST is indicated with endoscopic enucleation in the presence of a pseudo capsule. According to location in the gastric wall, GISTs are classified in to several types such as type 1 [very narrow connection with muscularis propria (MP) layer which protrudes in to the lumen], type 2 (wide based connection with MP layer and protrudes in the luminal side at obtuse angle), type 3 (located in the middle of gastric wall) and type 4 (protrudes into the serosal surface of gastric wall)[61]. This classification is very important when considering endoscopic enucleation. Endoscopic enucleation is best suitable for type 1 because of narrow connection to the MP layer and can be attempted for type 2. Type 3 and type 4 cannot be completely resected by endoscopic enucleation and hence endoscopic full-thickness resection (EFTR), laparoscopic and endoscopic cooperative surgery (LECS), laparoscopic-assisted endoscopic full-thickness resection (LAEFR) and non-exposed wall-inversion surgery (NEWS) should be considered[61]. Endoscopic enucleation includes various techniques like endoscopic submucosal dissection (ESD)[62], endoscopic muscularis dissection (EMD)[63] and endoscopic submucosal tunnel dissection (ESTD)[64]. Bialek et al[62] evaluated the efficacy, safety and outcomes of ESD for gastric sub epithelial tumors. Results showed 47% (17/37) sub epithelial tumors were GISTs, overall rate of R0 resection was 81.1% (30/37), and perforation rate was 5.4%[62]. Liu et al[63] evaluated the feasibility and safety of EMD. Results showed that 51.6% (16/31) were GISTs, 96.8% (30/31) were completely resected, perforation occurred in 12.9% (4/31, all of which were managed by endoscopic methods)[63]. ESTD procedure involves creation of the submucosal tunnel, dissection of the submucosal tumor (SMT) and closure of mucosal entry with hemostatic clips[64]. Gong et al[64] evaluated the feasibility and safety of ESTD in upper gastrointestinal SMTs. Results showed that 58.3% (7/12) were GISTs, complete tumor resection was achieved in all patients, en bloc resection in 83.3% (10/12, other 2 lesions were resected in 2 pieces) and 2 patients had both pneumothorax and subcutaneous emphysema which were managed conservatively[64]. Disadvantages of endoscopic techniques include tumor recurrence and peritoneal seeding secondary to perforation. It is unclear whether there is remnant GIST tissue after dissection causing tumor recurrence, although the dissection site is usually ablated with electrical knife or snare. Perforation occurs due to pseudo capsule injury during difficult MP layer dissection which increases the chance of peritoneal seeding. Peritoneal seeding is associated with poor prognosis because of increased tumor recurrence.
EFTR without laparoscopic assistance procedure involves introducing a single-chamber gastroscope into the stomach with a transparent cap attached to its tip. Dots are marked around the lesion and submucosal injection is done using normal saline with 1% indigo carmine and epinephrine (1:100000). Hook knife and IT knife are used to incise superficial layers overlying the SMT and snare is used to remove the mucosal and submucosal layers of gastric wall. Hook knife and IT knife are used to make circumferential dissection around the border of SMT. To visualize the SMT clearly, submucosal injection can be done again in the lower border of the tumor as needed. After the MP layer is reached and root of the tumor is exposed, gastric fluid is extracted as much as possible. Active perforation is made with the help of hook knife. After the tumor is completely exposed, SMT is removed en bloc with the snare. Dual channel gastroscope can be used for tumors with a broad basement which has the advantage of passing two snares through the accessory channels in to the gastric cavity. Tumor body is grasped with one snare and the other snare is used to en bloc enucleate the tumor along with the attached serosal layer. Titanium clips are used to close the defect in gastric wall. Paracentesis can be performed if there are signs of pneumoperitoneum during the procedure. Feng et al[65] evaluated the efficacy and safety of EFTR in 48 patients with gastric SMTs. Results showed that 43/48 had GIST, no post-EFTR complication such as bleeding or peritonitis, 5 had moderate postoperative abdominal distension because of air filtration (3 had abdominal paracentesis and the other 2 were managed conservatively)[65]. Zhou et al[66] evaluated the efficacy, feasibility and safety of EFTR for gastric SMTs originating from MP layer. Results showed that 16/26 were GISTs, en bloc resection rate was 100% and no major complications[66]. In general, there is a risk of peritoneal seeding with EFTR because it involves creating an active large perforation and hence gentle handling of GIST is necessary to maintain an intact pseudo capsule to prevent peritoneal seeding.
LECS has advantage over LWR especially for gastric SMTs located near esophagogastric junction or pyloric region because SMTs can be located accurately using endoscope and the resection of healthy stomach can be minimized[67]. The best indication for LECS is for gastric GISTs originating from MP layer which are intraluminal[61]. First, Argon plasma coagulation (APC) can be used to mark the periphery of the tumor[67]. A small incision is made on the marked area using standard needle knife after injecting 10% glycerin into submucosal layer. Using the IT knife, three-fourth of the marked area is cut circumferentially. Next, laparoscopic dissection of seromuscular layer is performed by making an artificial perforation and seromuscular dissection is carried out with ultrasonically activated device[67]. The incision is closed with the help of laparoscopic stapling device[67]. Hiki et al[67] analyzed seven patients who underwent LECS for gastric GISTs. Results showed that 6/7 were GISTs, no postoperative complications like bleeding, stenosis or anastomotic leakage, and successful tumor resection was done irrespective of tumor location (esophagogastric junction or pyloric ring). Tsujimoto et al[68] evaluated the feasibility and surgical outcomes of LECS for gastric SMTs. The authors found 16/20 were GISTs, no postoperative complications like bleeding, stenosis or anastomotic leakage, and there was no recurrence of tumor[68].
NEWS is a new technique developed to prevent peritoneal seeding from large active perforation and minimize resected tissue volume of stomach[69]. Mitsui et al[69] evaluated the efficacy and safety of NEWS in 6 patients with suspected gastric GIST. Results showed that 5/6 were GIST, en bloc resection was achieved in all GISTs, perforation occurred in 2/6 cases (1 case had muscle injury leading to perforation during mucosal cutting by endoscopic knife and the other case had laparoscopic mucosal injury leading to perforation during seromuscular cutting), and no postoperative complications[69]. Future studies with large cohort are needed to validate the safety of NEWS before it is standardized for GISTs treatment.
Tumor size, location, mitotic index and tumor rupture are the most important independent prognostic indicators to determine RFS[4]. Multiple stratification schema like National Institutes of Health (NIH) consensus criteria, Armed Forces Institute of Pathology (AFIP) criteria and the modified NIH consensus criteria were developed to predict risk of recurrence[4,70-72]. The most commonly used stratification method is AFIP criteria[73]. AFIP groups 3a and above are considered high risk for recurrence. This corresponds to 5-year recurrence rate of 30% based on nomogram evaluation[73]. DeMatteo et al[74] evaluated the overall survival (OS) in 106 patients who had undergone complete gross tumor removal but were considered high risk for recurrence. It was a phase II Z9000 trial lead by ACOSOG and all patients were treated with imatinib 400 mg per day for 1 year[74]. Results showed that OS for 1, 3 and 5-year was 99%, 97% and 83% respectively after a mean follow up of 7.7 years[74]. RFS rate for 1, 3 and 5-year was 96%, 60% and 40% respectively[74]. In the subsequent trial, patients were randomly assigned to receive imatinib 400 mg per day or placebo for one year[75]. RFS at the end of 1 year for imatinib vs placebo was 98% vs 83% respectively and OS for imatinib vs placebo was 99.2% vs 99.7% respectively[75]. Li et al[76] evaluated RFS in Chinese patients after complete tumor resection of GISTs. All patients in treatment group (56/105) were treated with imatinib 400 mg once a day for 3 years and 49/105 were not treated (control group)[76]. RFS for imatinib vs control group at the end of 1year, 2 year and 3 years were 100% vs 90%, 96% vs 57% and 89% vs 48% respectively[76]. All GISTs with size ≥ 3 cm, small bowel site and high mitotic index were shown to benefit from adjuvant imatinib treatment[50,75]. Joensuu et al[77] evaluated the RFS and OS in KIT-positive GISTs treated with imatinib for 3 year vs 1 year who had undergone complete tumor resection but considered high risk for recurrence. Results showed that RFS for patients treated with imatinib for 3 year vs 1 year were 65.6% vs 47.9% respectively and OS for 3 year vs 1 year were 92% vs 81.7% respectively[77]. Kang et al[78] evaluated the efficacy of adjuvant imatinib for 2 years in high risk GISTs with KIT exon 11 mutation after complete resection at four South Korean centers. The results showed median RFS was 58.9 mo compared to 22.7 mo in pre-imatinib era[78]. They also concluded that imatinib is effective in GIST recurrence even after completion of adjuvant imatinib therapy[78].
National comprehensive cancer network (NCCN) guidelines recommend neoadjuvant imatinib therapy to reduce tumor size before surgery and minimize morbidity in patients with primary GISTs considered unresectable or resectable with high risk morbidity[73]. Eisenberg et al[79] evaluated the safety and efficacy of neoadjuvant imatinib (600 mg/d) in patients with KIT positive primary GIST (≥ 5 cm, 32 patients) or with operable metastatic/recurrent GIST (≥ 2 cm, 20 patients). It was a prospective nonrandomized trial and imatinib was continued postoperatively for 2 years[79]. In primary GIST group, preoperative response was partial in 2 patients (7%), stable in 25 (83%) and unknown in 3 (10%); in metastatic or recurrent group, partial in 1 (4.5%), stable in 20 (91%), and progression in 1 (4.5%)[79]. Only 7 (13%) patients did not have any surgery (5 inoperable or unresectable, 1 patient refusal and 1 physician refusal)[79]. The estimated 2-year rate of TTP, PFS, OS in primary vs metastatic/recurrent GIST was 13.9% vs 13.6%, 82.7% vs 77.3% and 93.3% vs 90.9% respectively[79].
Fiore et al[80] prospectively evaluated the PFS in locally advanced or unresectable primary GISTs treated with preoperative imatinib. All patients who were considered high risk or needed extensive surgery (3 considered unresectable underwent complete resection, 7 who were initially considered to undergo extensive surgery were conservatively operated, 4 who were considered high perioperative risk underwent safe surgery) improved after preoperative imatinib therapy. PFS after 3 years was 77% from the time of initial imatinib treatment[80].
The outcome of advanced GISTs treated with imatinib is not clear. Demetri et al[81] evaluated the efficacy of imatinib on antitumor response, safety and tolerability in advanced GISTs. Results showed that 79 patients (53.7%) had partial response, 41 patients (27.9%) had stable disease and in 7 patients (4.8%) response could not be evaluated[81]. Adverse effects related to imatinib therapy were diarrhea, edema (periorbital and leg), fatigue and gastrointestinal bleeding[81]. Overall, the therapy was well tolerated. Blanke et al[82] conducted a multicenter randomized phase II trial and they evaluated the efficacy and long-term safety of imatinib (group A 400 vs group B 600 mg) in advanced GISTs positive for CD117 antigen. In group A (400 mg, 73 patients), the authors observed GISTs with complete response 0 (0%), partial response 50 (68.5%), stable 10 (13.7%), progressive 11 (15.1%) and unknown 2 (2.7%)[82]. In group B (600 mg, 74 patients), the authors reported GISTS with complete response 2 (2.7%), partial 48 (64.9%), stable 13 (17.6%), progressive 6 (8.1%) and unknown 5 (6.8%)[82]. Overall, imatinib was well tolerated[82]. In the subsequent phase III trial, Blanke et al[83] evaluated PFS or OS with standard imatinib dose (400 mg) vs higher dose (400 mg twice daily) in patients with incurable GISTs. After a median follow up of 4.5 years, median PFS for standard vs high dose imatinib was 18 mo vs 20 mo, median OS for standard vs high dose imatinib was 55 mo vs 51 mo respectively[83]. Treatment response in standard vs high dose imatinib were divided in to complete response (5% vs 3%), partial (40% vs 42%), stable (25% vs 22%), progressive disease (12% vs 10%) and inadequate assessment (10% vs 15%) respectively[83]. This study concluded that 400 mg twice daily imatinib was more toxic than 400 mg dose in treatment of incurable GISTs[83]. Debiec-Rychter et al[84] evaluated the efficacy of standard dose imatinib (400 mg) vs higher dose (400 mg two times daily) in advanced GIST based on mutational status (KIT or PDGFRA). There was a 61% relative risk reduction of PFS in GISTs expressing exon 9 mutation treated with high dose imatinib[84]. Overall, this study concluded that tumor genotype determines PFS and OS in advanced GISTs and also GISTs with KIT exon 9 benefited from 400 mg two times daily imatinib[84].
Heinrich et al[85] showed that presence of KIT exon-11 mutation (71.7%) had better treatment outcome with imatinib when compared to KIT exon-9 (44.4%) and wild-type mutation (44.6%) in advanced GISTs. The authors also showed that there was an improved response rate (complete/partial response) in patients with KIT exon-9 mutation treated with imatinib 800 mg vs 400 mg (67% vs 17%, P = 0.02)[85]. GIST meta-analysis group (MetaGIST) evaluated PFS and OS with imatinib (400 mg vs 800 mg) in advanced GISTs[86]. The results showed that there was a small but significant PFS (P = 0.04) advantage in high dose (400 mg twice daily) group and no difference in OS between both (400 and 800 mg) groups[86].
Demetri et al[87] evaluated patients treated with sunitinib in advanced GISTS who were intolerant or resistant to previous imatinib treatment. They concluded that median TTP with sunitinib vs placebo was 27.3 wk vs 6.4 wk respectively[87]. Overall, sunitinib was well tolerated and side effects like nausea, fatigue, skin discoloration and diarrhea were common[87].
Demetri et al[88] evaluated the efficacy and safety of regorafenib after failure of treatment with imatinib and sunitinib. Results showed that the median PFS in regorafenib vs placebo group were 4.8 mo vs 0.9 mo respectively[88]. There was no statistical significance in terms of OS between regorafenib and placebo group[88]. Drug related adverse events occurred in 130/132 (98.5%) in regorafenib group and 45/66 (68.2%) in placebo group[88]. The most common adverse effects of regorafenib include hypertension (31/132, 23.5%), hand foot skin reaction (26/132, 19.7%) and diarrhea (7/132, 5.3%)[88]. Overall, this study concluded that regorafenib significantly improved PFS in patients with advanced GISTs who failed treatment with imatinib and sunitinib[88].
The goal of follow-up after surgery is early detection and treatment of relapse. CT abdomen and pelvis is used for follow-up. Metastasis of GISTs outside the abdomen is infrequent. MRI or PET-CT can be used as an alternative for follow-up. Annual CT abdomen and pelvis for 5 years is recommended for low risk GISTs after surgery[89]. During adjuvant treatment with imatinib for high risk GISTs, CT abdomen and pelvis is recommended every 6 mo[89]. After adjuvant therapy is stopped, CT is repeated every 3-4 mo for first 2 years and there after every 6-12 mo for 10 years[89].
With increasing availability of EUS and improved knowledge of the pathogenesis of GISTs, accurate identification and differentiation of GISTs from other submucosal tumors are achieved. Although surgery is preferred, newer endoscopic techniques can be attempted by experienced endoscopists with the assistance of surgeons in suitable candidates. Neoadjuvant imatinib therapy is recommended for primary GISTs considered unresectable or resectable with high morbidity to reduce the tumor size before surgery and minimize morbidity. Adjuvant therapy with imatinib in intermediate and high risk GISTs improves OS and RFS. Sunitinib and regorafenib can be used in advanced GISTs after treatment failure with imatinib. Multidisciplinary approach involving endoscopist, pathologist, radiologist, medical oncologist and surgeon is required for optimal management of GIST.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Deng MM, Gu MJ, Lee SW S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Miettinen M, Lasota J. Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1-12. [PubMed] [Cited in This Article: ] |
| 2. | Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152:1259-1269. [PubMed] [Cited in This Article: ] |
| 3. | Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000;13:577-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 323] [Cited by in F6Publishing: 362] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 4. | Joensuu H, Vehtari A, Riihimäki J, Nishida T, Steigen SE, Brabec P, Plank L, Nilsson B, Cirilli C, Braconi C. Risk of recurrence of gastrointestinal stromal tumour after surgery: an analysis of pooled population-based cohorts. Lancet Oncol. 2012;13:265-274. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 576] [Cited by in F6Publishing: 607] [Article Influence: 46.7] [Reference Citation Analysis (0)] |
| 5. | Woodall CE, Brock GN, Fan J, Byam JA, Scoggins CR, McMasters KM, Martin RC. An evaluation of 2537 gastrointestinal stromal tumors for a proposed clinical staging system. Arch Surg. 2009;144:670-678. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Emile JF, Brahimi S, Coindre JM, Bringuier PP, Monges G, Samb P, Doucet L, Hostein I, Landi B, Buisine MP. Frequencies of KIT and PDGFRA mutations in the MolecGIST prospective population-based study differ from those of advanced GISTs. Med Oncol. 2012;29:1765-1772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Ducimetière F, Lurkin A, Ranchère-Vince D, Decouvelaere AV, Péoc’h M, Istier L, Chalabreysse P, Muller C, Alberti L, Bringuier PP. Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS One. 2011;6:e20294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 335] [Cited by in F6Publishing: 377] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 8. | Ma GL, Murphy JD, Martinez ME, Sicklick JK. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiol Biomarkers Prev. 2015;24:298-302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 152] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 9. | Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100:162-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 436] [Cited by in F6Publishing: 409] [Article Influence: 21.5] [Reference Citation Analysis (1)] |
| 10. | Postow MA, Robson ME. Inherited gastrointestinal stromal tumor syndromes: mutations, clinical features, and therapeutic implications. Clin Sarcoma Res. 2012;2:16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577-580. [PubMed] [Cited in This Article: ] |
| 12. | Broudy VC. Stem cell factor and hematopoiesis. Blood. 1997;90:1345-1364. [PubMed] [Cited in This Article: ] |
| 13. | Mussi C, Schildhaus HU, Gronchi A, Wardelmann E, Hohenberger P. Therapeutic consequences from molecular biology for gastrointestinal stromal tumor patients affected by neurofibromatosis type 1. Clin Cancer Res. 2008;14:4550-4555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 14. | Heinrich MC, Corless CL, Duensing A, McGreevey L, Chen CJ, Joseph N, Singer S, Griffith DJ, Haley A, Town A. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299:708-710. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1712] [Cited by in F6Publishing: 1660] [Article Influence: 79.0] [Reference Citation Analysis (0)] |
| 15. | Pantaleo MA, Astolfi A, Indio V, Moore R, Thiessen N, Heinrich MC, Gnocchi C, Santini D, Catena F, Formica S. SDHA loss-of-function mutations in KIT-PDGFRA wild-type gastrointestinal stromal tumors identified by massively parallel sequencing. J Natl Cancer Inst. 2011;103:983-987. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 16. | Janeway KA, Kim SY, Lodish M, Nosé V, Rustin P, Gaal J, Dahia PL, Liegl B, Ball ER, Raygada M. Defects in succinate dehydrogenase in gastrointestinal stromal tumors lacking KIT and PDGFRA mutations. Proc Natl Acad Sci USA. 2011;108:314-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 436] [Cited by in F6Publishing: 433] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 17. | Selak MA, Armour SM, MacKenzie ED, Boulahbel H, Watson DG, Mansfield KD, Pan Y, Simon MC, Thompson CB, Gottlieb E. Succinate links TCA cycle dysfunction to oncogenesis by inhibiting HIF-alpha prolyl hydroxylase. Cancer Cell. 2005;7:77-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1460] [Cited by in F6Publishing: 1480] [Article Influence: 77.9] [Reference Citation Analysis (0)] |
| 18. | Pasini B, McWhinney SR, Bei T, Matyakhina L, Stergiopoulos S, Muchow M, Boikos SA, Ferrando B, Pacak K, Assie G. Clinical and molecular genetics of patients with the Carney-Stratakis syndrome and germline mutations of the genes coding for the succinate dehydrogenase subunits SDHB, SDHC, and SDHD. Eur J Hum Genet. 2008;16:79-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 347] [Cited by in F6Publishing: 306] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 19. | Graadt van Roggen JF, van Velthuysen ML, Hogendoorn PC. The histopathological differential diagnosis of gastrointestinal stromal tumours. J Clin Pathol. 2001;54:96-102. [PubMed] [Cited in This Article: ] |
| 20. | Sarlomo-Rikala M, Kovatich AJ, Barusevicius A, Miettinen M. CD117: a sensitive marker for gastrointestinal stromal tumors that is more specific than CD34. Mod Pathol. 1998;11:728-734. [PubMed] [Cited in This Article: ] |
| 21. | Sueki H, Whitaker D, Buchsbaum M, Murphy GF. Novel interactions between dermal dendrocytes and mast cells in human skin. Implications for hemostasis and matrix repair. Lab Invest. 1993;69:160-172. [PubMed] [Cited in This Article: ] |
| 22. | Levy AD, Remotti HE, Thompson WM, Sobin LH, Miettinen M. Gastrointestinal stromal tumors: radiologic features with pathologic correlation. Radiographics. 2003;23:283-304, 456; quiz 532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 355] [Cited by in F6Publishing: 316] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 23. | Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005;29:52-68. [PubMed] [Cited in This Article: ] |
| 24. | Jiang ZX, Zhang SJ, Peng WJ, Yu BH. Rectal gastrointestinal stromal tumors: imaging features with clinical and pathological correlation. World J Gastroenterol. 2013;19:3108-3116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 32] [Cited by in F6Publishing: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Sorour MA, Kassem MI, Ghazal Ael-H, El-Riwini MT, Abu Nasr A. Gastrointestinal stromal tumors (GIST) related emergencies. Int J Surg. 2014;12:269-280. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Carney JA. Gastric stromal sarcoma, pulmonary chondroma, and extra-adrenal paraganglioma (Carney Triad): natural history, adrenocortical component, and possible familial occurrence. Mayo Clin Proc. 1999;74:543-552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 321] [Cited by in F6Publishing: 344] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 27. | Takazawa Y, Sakurai S, Sakuma Y, Ikeda T, Yamaguchi J, Hashizume Y, Yokoyama S, Motegi A, Fukayama M. Gastrointestinal stromal tumors of neurofibromatosis type I (von Recklinghausen’s disease). Am J Surg Pathol. 2005;29:755-763. [PubMed] [Cited in This Article: ] |
| 28. | DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51-58. [PubMed] [Cited in This Article: ] |
| 29. | Burkill GJ, Badran M, Al-Muderis O, Meirion Thomas J, Judson IR, Fisher C, Moskovic EC. Malignant gastrointestinal stromal tumor: distribution, imaging features, and pattern of metastatic spread. Radiology. 2003;226:527-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 299] [Cited by in F6Publishing: 268] [Article Influence: 12.8] [Reference Citation Analysis (1)] |
| 30. | Gutierrez JC, De Oliveira LO, Perez EA, Rocha-Lima C, Livingstone AS, Koniaris LG. Optimizing diagnosis, staging, and management of gastrointestinal stromal tumors. J Am Coll Surg. 2007;205:479-491 (Quiz 524). [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Valsangkar N, Sehdev A, Misra S, Zimmers TA, O’Neil BH, Koniaris LG. Current management of gastrointestinal stromal tumors: Surgery, current biomarkers, mutations, and therapy. Surgery. 2015;158:1149-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 32. | Paulsen SR, Huprich JE, Fletcher JG, Booya F, Young BM, Fidler JL, Johnson CD, Barlow JM, Earnest F. CT enterography as a diagnostic tool in evaluating small bowel disorders: review of clinical experience with over 700 cases. Radiographics. 2006;26:641-657; discussion 657-662. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 326] [Cited by in F6Publishing: 345] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 33. | Bano S, Puri SK, Upreti L, Chaudhary V, Sant HK, Gondal R. Gastrointestinal stromal tumors (GISTs): an imaging perspective. Jpn J Radiol. 2012;30:105-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Hwang JH, Saunders MD, Rulyak SJ, Shaw S, Nietsch H, Kimmey MB. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc. 2005;62:202-208. [PubMed] [Cited in This Article: ] |
| 35. | Palazzo L, Landi B, Cellier C, Cuillerier E, Roseau G, Barbier JP. Endosonographic features predictive of benign and malignant gastrointestinal stromal cell tumours. Gut. 2000;46:88-92. [PubMed] [Cited in This Article: ] |
| 36. | Rösch T, Kapfer B, Will U, Baronius W, Strobel M, Lorenz R, Ulm K. Accuracy of endoscopic ultrasonography in upper gastrointestinal submucosal lesions: a prospective multicenter study. Scand J Gastroenterol. 2002;37:856-862. [PubMed] [Cited in This Article: ] |
| 37. | Chen TH, Hsu CM, Chu YY, Wu CH, Chen TC, Hsu JT, Yeh TS, Lin CJ, Chiu CT. Association of endoscopic ultrasonographic parameters and gastrointestinal stromal tumors (GISTs): can endoscopic ultrasonography be used to screen gastric GISTs for potential malignancy? Scand J Gastroenterol. 2016;51:374-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | DeWitt J, Emerson RE, Sherman S, Al-Haddad M, McHenry L, Cote GA, Leblanc JK. Endoscopic ultrasound-guided Trucut biopsy of gastrointestinal mesenchymal tumor. Surg Endosc. 2011;25:2192-2202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 39. | Na HK, Lee JH, Park YS, Ahn JY, Choi KS, Kim DH, Choi KD, Song HJ, Lee GH, Jung HY. Yields and Utility of Endoscopic Ultrasonography-Guided 19-Gauge Trucut Biopsy versus 22-Gauge Fine Needle Aspiration for Diagnosing Gastric Subepithelial Tumors. Clin Endosc. 2015;48:152-157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 40. | Yoshikawa K, Shimada M, Kurita N, Sato H, Iwata T, Morimoto S, Miyatani T, Kashihara H, Takasu C, Matsumoto N. Efficacy of PET-CT for predicting the malignant potential of gastrointestinal stromal tumors. Surg Today. 2013;43:1162-1167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 41. | Kamiyama Y, Aihara R, Nakabayashi T, Mochiki E, Asao T, Kuwano H, Oriuchi N, Endo K. 18F-fluorodeoxyglucose positron emission tomography: useful technique for predicting malignant potential of gastrointestinal stromal tumors. World J Surg. 2005;29:1429-1435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 42. | Van den Abbeele AD. The lessons of GIST--PET and PET/CT: a new paradigm for imaging. Oncologist. 2008;13 Suppl 2:8-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 213] [Cited by in F6Publishing: 193] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 43. | Gayed I, Vu T, Iyer R, Johnson M, Macapinlac H, Swanston N, Podoloff D. The role of 18F-FDG PET in staging and early prediction of response to therapy of recurrent gastrointestinal stromal tumors. J Nucl Med. 2004;45:17-21. [PubMed] [Cited in This Article: ] |
| 44. | Chen MY, Bechtold RE, Savage PD. Cystic changes in hepatic metastases from gastrointestinal stromal tumors (GISTs) treated with Gleevec (imatinib mesylate). AJR Am J Roentgenol. 2002;179:1059-1062. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 45. | Van den Abbeele AD, Badawi RD. Use of positron emission tomography in oncology and its potential role to assess response to imatinib mesylate therapy in gastrointestinal stromal tumors (GISTs). Eur J Cancer. 2002;38 Suppl 5:S60-S65. [PubMed] [Cited in This Article: ] |
| 46. | Pisters PW, Patel SR. Gastrointestinal stromal tumors: current management. J Surg Oncol. 2010;102:530-538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 47. | Choi H, Charnsangavej C, de Castro Faria S, Tamm EP, Benjamin RS, Johnson MM, Macapinlac HA, Podoloff DA. CT evaluation of the response of gastrointestinal stromal tumors after imatinib mesylate treatment: a quantitative analysis correlated with FDG PET findings. AJR Am J Roentgenol. 2004;183:1619-1628. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 360] [Cited by in F6Publishing: 388] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 48. | Benjamin RS, Choi H, Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA, Charnsangavej C. We should desist using RECIST, at least in GIST. J Clin Oncol. 2007;25:1760-1764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 434] [Cited by in F6Publishing: 404] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 49. | Joensuu H, Rutkowski P, Nishida T, Steigen SE, Brabec P, Plank L, Nilsson B, Braconi C, Bordoni A, Magnusson MK. KIT and PDGFRA mutations and the risk of GI stromal tumor recurrence. J Clin Oncol. 2015;33:634-642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 109] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 50. | Corless CL, Ballman KV, Antonescu CR, Kolesnikova V, Maki RG, Pisters PW, Blackstein ME, Blanke CD, Demetri GD, Heinrich MC. Pathologic and molecular features correlate with long-term outcome after adjuvant therapy of resected primary GI stromal tumor: the ACOSOG Z9001 trial. J Clin Oncol. 2014;32:1563-1570. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 200] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 51. | Gold JS, Gönen M, Gutiérrez A, Broto JM, García-del-Muro X, Smyrk TC, Maki RG, Singer S, Brennan MF, Antonescu CR. Development and validation of a prognostic nomogram for recurrence-free survival after complete surgical resection of localised primary gastrointestinal stromal tumour: a retrospective analysis. Lancet Oncol. 2009;10:1045-1052. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 329] [Cited by in F6Publishing: 350] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 52. | Miettinen M, El-Rifai W, H L Sobin L, Lasota J. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol. 2002;33:478-483. [PubMed] [Cited in This Article: ] |
| 53. | Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459-465. [PubMed] [Cited in This Article: ] |
| 54. | Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006;130:1466-1478. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 55. | Nishida T, Blay JY, Hirota S, Kitagawa Y, Kang YK. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer. 2016;19:3-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 284] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 56. | McCarter MD, Antonescu CR, Ballman KV, Maki RG, Pisters PW, Demetri GD, Blanke CD, von Mehren M, Brennan MF, McCall L. Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg. 2012;215:53-59; discussion 59-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 57. | Choi SM, Kim MC, Jung GJ, Kim HH, Kwon HC, Choi SR, Jang JS, Jeong JS. Laparoscopic wedge resection for gastric GIST: long-term follow-up results. Eur J Surg Oncol. 2007;33:444-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 87] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 58. | Goh BK, Chow PK, Chok AY, Chan WH, Chung YF, Ong HS, Wong WK. Impact of the introduction of laparoscopic wedge resection as a surgical option for suspected small/medium-sized gastrointestinal stromal tumors of the stomach on perioperative and oncologic outcomes. World J Surg. 2010;34:1847-1852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 59. | Lee HH, Hur H, Jung H, Park CH, Jeon HM, Song KY. Laparoscopic wedge resection for gastric submucosal tumors: a size-location matched case-control study. J Am Coll Surg. 2011;212:195-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Kim DJ, Lee JH, Kim W. Laparoscopic resection for 125 gastroduodenal submucosal tumors. Ann Surg Treat Res. 2014;86:199-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Kim HH. Endoscopic treatment for gastrointestinal stromal tumor: Advantages and hurdles. World J Gastrointest Endosc. 2015;7:192-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 54] [Cited by in F6Publishing: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 62. | Białek A, Wiechowska-Kozłowska A, Pertkiewicz J, Polkowski M, Milkiewicz P, Karpińska K, Ławniczak M, Starzyńska T. Endoscopic submucosal dissection for treatment of gastric subepithelial tumors (with video). Gastrointest Endosc. 2012;75:276-286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 63. | Liu BR, Song JT, Qu B, Wen JF, Yin JB, Liu W. Endoscopic muscularis dissection for upper gastrointestinal subepithelial tumors originating from the muscularis propria. Surg Endosc. 2012;26:3141-3148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 64. | Gong W, Xiong Y, Zhi F, Liu S, Wang A, Jiang B. Preliminary experience of endoscopic submucosal tunnel dissection for upper gastrointestinal submucosal tumors. Endoscopy. 2012;44:231-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 65. | Feng Y, Yu L, Yang S, Li X, Ding J, Chen L, Xu Y, Shi R. Endolumenal endoscopic full-thickness resection of muscularis propria-originating gastric submucosal tumors. J Laparoendosc Adv Surg Tech A. 2014;24:171-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 66. | Zhou PH, Yao LQ, Qin XY, Cai MY, Xu MD, Zhong YS, Chen WF, Zhang YQ, Qin WZ, Hu JW. Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surg Endosc. 2011;25:2926-2931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 209] [Cited by in F6Publishing: 228] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 67. | Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, Miki A, Ohyama S, Seto Y. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008;22:1729-1735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 297] [Cited by in F6Publishing: 317] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 68. | Tsujimoto H, Yaguchi Y, Kumano I, Takahata R, Ono S, Hase K. Successful gastric submucosal tumor resection using laparoscopic and endoscopic cooperative surgery. World J Surg. 2012;36:327-330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 69. | Mitsui T, Niimi K, Yamashita H, Goto O, Aikou S, Hatao F, Wada I, Shimizu N, Fujishiro M, Koike K. Non-exposed endoscopic wall-inversion surgery as a novel partial gastrectomy technique. Gastric Cancer. 2014;17:594-599. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 70. | Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol. 2002;10:81-89. [PubMed] [Cited in This Article: ] |
| 71. | Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23:70-83. [PubMed] [Cited in This Article: ] |
| 72. | Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39:1411-1419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 699] [Cited by in F6Publishing: 785] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 73. | Balachandran VP, DeMatteo RP. Gastrointestinal stromal tumors: who should get imatinib and for how long? Adv Surg. 2014;48:165-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 74. | DeMatteo RP, Ballman KV, Antonescu CR, Corless C, Kolesnikova V, von Mehren M, McCarter MD, Norton J, Maki RG, Pisters PW. Long-term results of adjuvant imatinib mesylate in localized, high-risk, primary gastrointestinal stromal tumor: ACOSOG Z9000 (Alliance) intergroup phase 2 trial. Ann Surg. 2013;258:422-429. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 119] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 75. | Dematteo RP, Ballman KV, Antonescu CR, Maki RG, Pisters PW, Demetri GD, Blackstein ME, Blanke CD, von Mehren M, Brennan MF. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;373:1097-1104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 986] [Cited by in F6Publishing: 913] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 76. | Li J, Gong JF, Wu AW, Shen L. Post-operative imatinib in patients with intermediate or high risk gastrointestinal stromal tumor. Eur J Surg Oncol. 2011;37:319-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 77. | Joensuu H, Eriksson M, Sundby Hall K, Hartmann JT, Pink D, Schütte J, Ramadori G, Hohenberger P, Duyster J, Al-Batran SE. One vs three years of adjuvant imatinib for operable gastrointestinal stromal tumor: a randomized trial. JAMA. 2012;307:1265-1272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 664] [Cited by in F6Publishing: 632] [Article Influence: 52.7] [Reference Citation Analysis (0)] |
| 78. | Kang YK, Kang BW, Im SA, Lee JL, Park SR, Kang WK, Chang HM, Kim TW, Oh DY, Jung KH. Two-year adjuvant imatinib mesylate after complete resection of localized, high-risk GIST with KIT exon 11 mutation. Cancer Chemother Pharmacol. 2013;71:43-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 79. | Eisenberg BL, Harris J, Blanke CD, Demetri GD, Heinrich MC, Watson JC, Hoffman JP, Okuno S, Kane JM, von Mehren M. Phase II trial of neoadjuvant/adjuvant imatinib mesylate (IM) for advanced primary and metastatic/recurrent operable gastrointestinal stromal tumor (GIST): early results of RTOG 0132/ACRIN 6665. J Surg Oncol. 2009;99:42-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 285] [Cited by in F6Publishing: 261] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 80. | Fiore M, Palassini E, Fumagalli E, Pilotti S, Tamborini E, Stacchiotti S, Pennacchioli E, Casali PG, Gronchi A. Preoperative imatinib mesylate for unresectable or locally advanced primary gastrointestinal stromal tumors (GIST). Eur J Surg Oncol. 2009;35:739-745. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 81. | Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472-480. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3203] [Cited by in F6Publishing: 3013] [Article Influence: 137.0] [Reference Citation Analysis (0)] |
| 82. | Blanke CD, Demetri GD, von Mehren M, Heinrich MC, Eisenberg B, Fletcher JA, Corless CL, Fletcher CD, Roberts PJ, Heinz D. Long-term results from a randomized phase II trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008;26:620-625. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 716] [Cited by in F6Publishing: 712] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 83. | Blanke CD, Rankin C, Demetri GD, Ryan CW, von Mehren M, Benjamin RS, Raymond AK, Bramwell VH, Baker LH, Maki RG. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26:626-632. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 746] [Cited by in F6Publishing: 737] [Article Influence: 46.1] [Reference Citation Analysis (1)] |
| 84. | Debiec-Rychter M, Sciot R, Le Cesne A, Schlemmer M, Hohenberger P, van Oosterom AT, Blay JY, Leyvraz S, Stul M, Casali PG. KIT mutations and dose selection for imatinib in patients with advanced gastrointestinal stromal tumours. Eur J Cancer. 2006;42:1093-1103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 640] [Cited by in F6Publishing: 613] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 85. | Heinrich MC, Owzar K, Corless CL, Hollis D, Borden EC, Fletcher CD, Ryan CW, von Mehren M, Blanke CD, Rankin C. Correlation of kinase genotype and clinical outcome in the North American Intergroup Phase III Trial of imatinib mesylate for treatment of advanced gastrointestinal stromal tumor: CALGB 150105 Study by Cancer and Leukemia Group B and Southwest Oncology Group. J Clin Oncol. 2008;26:5360-5367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 441] [Cited by in F6Publishing: 439] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 86. | Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1,640 patients. J Clin Oncol. 2010;28:1247-1253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 337] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 87. | Demetri GD, van Oosterom AT, Garrett CR, Blackstein ME, Shah MH, Verweij J, McArthur G, Judson IR, Heinrich MC, Morgan JA. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368:1329-1338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1942] [Cited by in F6Publishing: 1830] [Article Influence: 101.7] [Reference Citation Analysis (0)] |
| 88. | Demetri GD, Reichardt P, Kang YK, Blay JY, Rutkowski P, Gelderblom H, Hohenberger P, Leahy M, von Mehren M, Joensuu H. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295-302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 942] [Cited by in F6Publishing: 938] [Article Influence: 85.3] [Reference Citation Analysis (0)] |
| 89. | Joensuu H, Martin-Broto J, Nishida T, Reichardt P, Schöffski P, Maki RG. Follow-up strategies for patients with gastrointestinal stromal tumour treated with or without adjuvant imatinib after surgery. Eur J Cancer. 2015;51:1611-1617. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |