Published online Apr 10, 2016. doi: 10.5306/wjco.v7.i2.265
Peer-review started: September 8, 2015
First decision: October 16, 2015
Revised: October 19, 2015
Accepted: December 18, 2015
Article in press: December 21, 2015
Published online: April 10, 2016
Processing time: 218 Days and 9.7 Hours
Parathyroid hormone mediated hypercalcemia is not always exclusively primary hyperparathyroidism and rarely could be due to ectopic parathyroid hormone secretion from tumor cells. We present a case of 86-year-old female with metastatic gall bladder adenocarcinoma diagnosed eight months back who presented with generalized fatigue and poor oral intake and was found to be hypercalcemic with elevated parathyroid hormone levels. Imaging with technetium 99 m sestamibi scintigraphy with dual phase, subtraction thyroid scan (dual isotope scintigraphy), magnetic resonance imaging and ultrasonography did not demonstrate any parathyroid lesion in normal or ectopic sites. We believe that the tumor cells were the source of ectopic parathyroid hormone secretion as we had excluded all the other possibilities with extensive combined imaging thereby increasing the sensitivity of our testing. We report the first case of metastatic gall bladder adenocarcinoma with paraneoplastic ectopic parathyroid hormone secretion.
Core tip: Gallbladder carcinoma rarely can cause hypercalcemia with very few reported cases but they were all due to parathyroid hormone (PTH) related peptide. We present the first case of metastatic gallbladder adenocarcinoma with hypercalcemia due to ectopic PTH secretion from tumor cells. PTH mediated hypercalcemia is not exclusively primary hyperparathyroidism and awareness of this rare paraneoplastic presentation will prevent unnecessary parathyroid surgeries. Moreover this case prompts physicians to look for another ectopic source in the absence of parathyroid lesion which would facilitate early diagnosis of an underlying malignancy.
- Citation: Yogarajah M, Sivasambu B, Shiferaw-Deribe Z. Gallbladder adenocarcinoma and paraneoplastic parathyroid hormone mediated hypercalcemia. World J Clin Oncol 2016; 7(2): 265-269
- URL: https://www.wjgnet.com/2218-4333/full/v7/i2/265.htm
- DOI: https://dx.doi.org/10.5306/wjco.v7.i2.265
Hypercalcemia is a commonly encountered metabolic disorder which can range from mild asymptomatic hypercalcemia to severe symptomatic hypercalcemia. The imbalance between calcium absorption, urine excretion and bone resorption leads to elevated levels of calcium levels as seen in excessive bone resorption, increased gastro intestinal absorption of calcium and impaired urinary excretion of calcium. The most common etiologies are primary hyperparathyroidism and malignancy which constitute more than 90% of the hypercalcemia cases. 20%-30% of patients with malignancy develop hypercalcemia and is considered to be a poor prognostic factor[1]. Hypercalcemia of malignancy has been described since early 1920 and has been evolving with the humoral factor involvement first proposed in 1941 followed by discovery of parathyroid hormone related peptide (PTHrP) in 1987. Humoral hypercalcemia of malignancy due to ectopic parathyroid hormone (PTH) secretion by tumor cells is a very rare entity with only few reported cases. We report the first case of metastatic gallbladder adenocarcinoma presenting with hypercalcemia secondary to ectopic PTH secretion.
An 86-year-old female was brought to the emergency department due to generalized weakness, loss of appetite and poor oral intake for 5 d. She denied any fever, increased urine output or constipation. Review of the systems was unrevealing. Her granddaughter whom the patient lives with stated that the patient was lethargic and was occasionally confused for the last 5 d. Eight months back patient was diagnosed to have gall bladder adenocarcinoma with hepatic and peritoneal metastasis and underwent cholecystectomy, however decided not to continue any further treatment with chemotherapy. She had no other medical problems and was not on any medications. Physical examination revealed evidence of dehydration with dry mucous membranes but she was hemodynamically stable. Patient was found to be lethargic however was arousable and oriented to time, place and person. All other systems examination was negative.
Initial labs revealed mild macrocytic anemia with a hemoglobin of 11.4 g/dL. The leucocyte count and platelet count was normal. There was evidence of mild dehydration with mildly increased blood urea nitrogen at 29 mg/dL (NR 8-20) and normal creatinine. She had significantly elevated corrected total calcium of 15.5 mg/dL with albumin of 3 g/dL. Phosphorous was 2 mg/dL (NR = 2.4-4.7). The liver enzymes showed an alkaline phosphatase of 142 IU/L (NR = 32-91) and other liver enzymes and bilirubin were normal.
Patient was hydrated and was started on calcitonin for immediate control of calcium levels and subsequently was given intravenous pamidronate of 90 mg. Hypercalcemia resolved by day 3 of admission and she became more awake and alert.
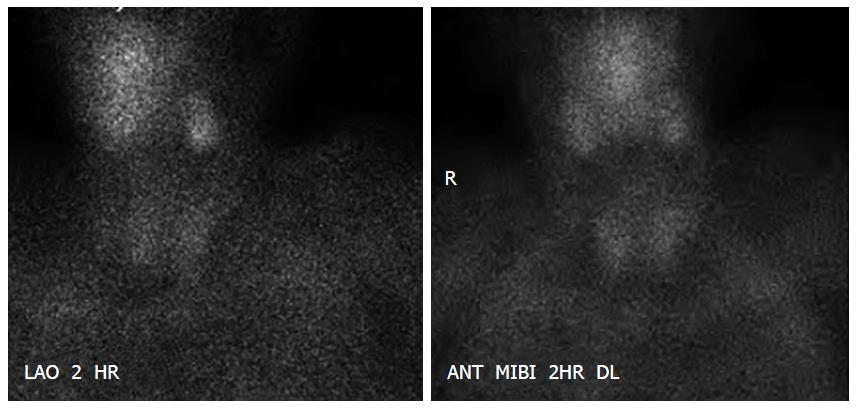
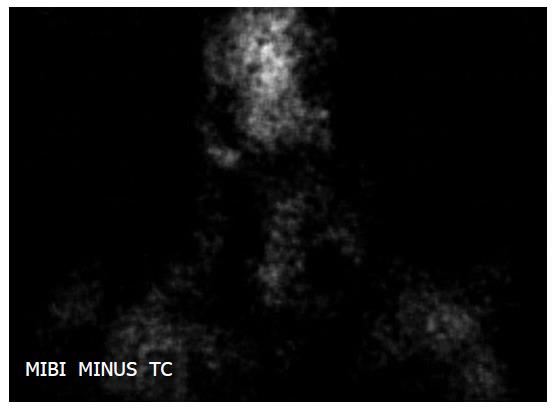
Further evaluation to determine the etiology of hypercalcemia showed a significantly elevated PTH of 162 pg/mL (normal range 15-65) and normal PTHrP, 25-hydroxyvitamin D and 1,25 dihydroxyvitamin D levels suggestive of a biochemical diagnosis of primary hyperparathyroidism. To localise the parathyroid lesion imaging with technetium-99 m (Tc-99 m) sestamibi scintigraphy with dual phase (Figure 1) and subtraction thyroid scan (dual isotope scintigraphy) with technetium pertechnetate (Figure 2) were done and reviewed by experienced nuclear medicine radiologist however did not reveal any parathyroid lesion.
PTH was repeated again and was persistently high at 185 pg/mL with normal PTHrP. Additional imaging with magnetic resonance imaging and ultrasonography was obtained to increase the sensitivity of the testing however was negative for parathyroid lesion in anatomical and ectopic sites but did show a 1.1 cm nodule in the left lobe of the thyroid gland. The possibility of ectopic parathyroid tissue was considered and ultrasound guided fine needle aspiration of thyroid gland performed did not demonstrate any parathyroid tissue and cytology revealed benign follicular adenoma. Thyroid function test was normal. A bone scan was negative for metastasis.
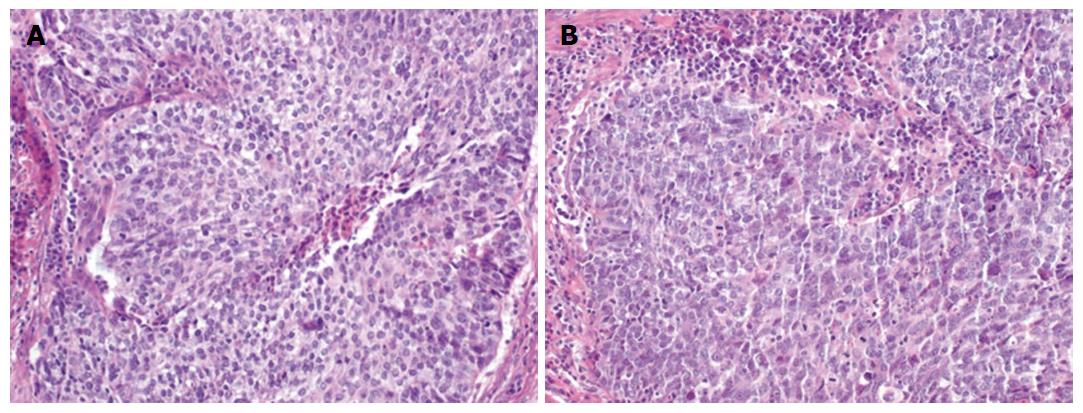
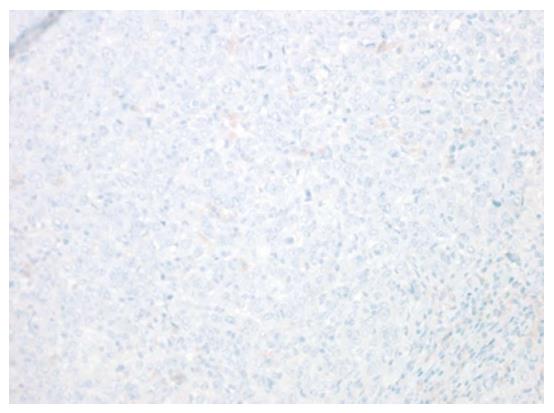
Patient had biochemical evidence of PTH mediated hypercalcemia but had no parathyroid lesions in anatomical and ectopic sites after extensive multiple imaging confirming the ectopic nature of the PTH secretion. The calcium levels prior to this admission was reviewed and was always normal with sudden dramatic elevation during this admission which is usually unlikely with primary hyperparathyroidism in which gradual increase of calcium is noted. This elevated PTH likely could be explained by ectopic PTH secretion by tumor cells in a patient with history of metastatic gallbladder cancer. We reviewed the previous histological slides of the primary tumor (Figure 3) and did immunohistochemical staining for PTH (Figure 4) but it was negative, as at the time of diagnosis patient was not hypercalcemic and likely tumor cells did not demonstrate PTH.
Patient developed another episode of hypercalcemia after 18 d of pamidronate administration and was started on cinacalcet after which her calcium levels remained controlled. Patient did not want to pursue with chemotherapy which would have been the best option to control the hypercalcemia and preferred to be in comfort care and was placed on home hospice.
Hypercalcemia could be a paraneoplastic manifestation that could occur due to multiple mechanisms. The commonest cancers associated with hypercalcemia are breast cancer, lung cancer and multiple myeloma[1]. Hypercalcemia of malignancy could result due to bone metastasis and induction of osteoclasts via cytokines or could occur in the absence of bone metastases due to humoral factors such as PTHrP or calcitriol secreted by the tumor. In 1941 Fuller Albright first described humoral hypercalcemia of malignancy which he postulated is occurring due to PTH or a similar peptide[2]. In 1987 PTHrP was discovered and attributed to the development of humoral hypercalcemia of malignancy. PTHrP is encoded in a different gene to that of PTH and therefore the amino acids sequence and immunoreactivity are distinct though both have a common receptor.
Hypercalcemia is classified based on PTH levels with a normal or high value pointing towards PTH mediated hypercalcemia as seen in primary hyperparathyroidism and suppressed levels favoring the diagnosis PTH independent hypercalcemia as seen in humoral hypercalcemia. Elevated PTHrP will lead to suppressed PTH levels and presence of elevated PTH levels highly suggests concurrent primary hyperparathyroidism. However there are reported cases of humoral hypercalcemia in which the tumor cells secreted both PTH and PTHrP[3].
Our patient had significantly elevated PTH and normal PTHrP suggesting a diagnosis of primary hyperparathyroidism. However with combined imaging of technetium 99 m sestamibi scintigraphy with dual phase, subtraction thyroid scan (dual isotope scintigraphy), ultrasonography and magnetic resonance imaging with T1 and T2 weighted images we were unable to demonstrate any parathyroid lesion in anatomical or ectopic sites excluding the possibility of primary hyperparathyroidism. The sensitivity of sestamibi scan combined with ultrasonography is 95% in detecting parathyroid lesions[4]. When magnetic resonance imaging is added, the sensitivity to detect parathyroid lesions increases to 96.2% and sensitivity to detect ectopic parathyroid lesions increases to 100%[5].
Ectopic secretion of PTH by tumor cells as a mechanism of hypercalcemia of malignancy has been reported very rarely with various malignancies. Doyle et al[6] reviewed the cases of malignancies associated with ectopic PTH secretion since the discovery of PTHrP, and the techniques used to demonstrate PTH and found 17 reported cases so far with their case being the 18th case.
Gall bladder adenocarcinoma is not commonly associated with paraneoplastic hypercalcemia and has been scarcely described in literature[7-10]. However the hypercalcemia was associated with elevated PTHrP[7] and this is the first case of Gall bladder adenocarcinoma with ectopic PTH secretion.
Various techniques has been used in demonstrating ectopic PTH secretion. Immunohistochemical staining for PTH, PTH mRNA synthesis of tumor cells similar to that of parathyroid cells identified by Northern Blot, PTH gene expression, venous sampling with high level of PTH in the draining vein and sestamibi scan were the methods used to confirm ectopic PTH secretion.
Unfortunately we were unable to demonstrate PTH in the tumor cells. Initial primary tumor cells did not show PTH on immunohistochemical staining as likely at that point there was no PTH expression and patient also didn’t have hypercalcemia. She developed hypercalcemia after 8 mo of diagnosis of metastatic gall bladder adenocarcinoma and repeating the biopsy to demonstrate PTH in the tumor cell at the hypercalcemic phase was not at the best interest of the patient who was not willing for any further intervention. The only explanation for the significantly elevated PTH in the absence of a parathyroid lesion and ectopic parathyroid could only be ectopic PTH secretion by the tumor cells.
Treatment of ectopic PTH mediated hypercalcemia of malignancy is challenging with no definitive management. In most cases treatment of the underlying malignancy helped in controlling the hypercalcemia. Transcatheter arterial embolization has been utilized in treating hepatocellular carcinoma with PTH secretion[11]. Hypercalcemia of malignancy is treated with bisphosphonates and in refractory cases denusomab has been approved by Food and Drug Administration. However ectopic PTH secretion biochemically mimic’s primary hyperparathyroidism. In patients with primary hyperparathyroidism who are not candidates for surgery bisphosphonates are preferred when there is evidence of osteoporosis or osteopenia. In the absence bone loss cinacalcet is the choice. Cinacalcet lowers PTH and calcium by increasing sensitivity of calcium-sensing receptor (CaSR). Under and over expression of CaSR in various malignancies has been found and the role of cinacalcet in treating cancer needs further studies and therefore the role in treating ectopic PTH induced hypercalcemia of malignancy is still obscure[12].
We started our patient on pamidronate and though she initially had a response she relapsed later with recurrent hypercalcemia. There was no option for chemotherapy to control the hypercalcemia as patient refused. She was started on cinacalcet to lower her calcium and responded well.
We present the first case of hypercalcemia due to ectopic PTH secretion of metastatic gallbladder adenocarcinoma. Awareness of this rare presentation will prevent unnecessary parathyroid surgeries. Moreover this case prompts physicians to look for another ectopic source in the absence of parathyroid lesion which would facilitate early diagnosis of an underlying malignancy.
An 86-year-old female was brought to the emergency department due to generalized weakness, loss of appetite and poor oral intake for 5 d and a history of metastatic gallbladder carcinoma.
She had evidence of dehydration with dry mucous membranes. She was found to be lethargic however was arousable and oriented to time, place and person.
Dehydration due to poor oral intake, sepsis.
Corrected total calcium was 15.5 mg/dL. Further workup showed parathyroid hormone of 162 pg/mL (normal range 15-65).
Technetium-99 m sestamibi scintigraphy with dual phase, subtraction thyroid scan (dual isotope scintigraphy) with technetium pertechnetate, magnetic resonance imaging and ultrasonography did not show and parathyroid lesion.
Biopsy of the thyroid nodule showed benign follicular adenoma and no ectopic parathyroid gland.
IV pamidronate followed by Cinnacalcet to control Ca as patient refused chemotherapy.
Gallbladder carcinoma rarely can cause hypercalcemia with very few reported cases but they were all due parathyroid hormone (PTH) related peptide. The authors present the first case of metastatic gallbladder adenocarcinoma with hypercalcemia due to ectopic PTH secretion from tumor cells.
The authors present the first case of hypercalcemia due to ectopic PTH secretion of metastatic gallbladder adenocarcinoma. Awareness of this rare presentation will prevent unnecessary parathyroid surgeries. Moreover this case prompts physicians to look for another ectopic source in the absence of parathyroid lesion which would facilitate early diagnosis of an underlying malignancy.
The paper is well written.
P- Reviewer: Kabir A, Lasithiotakis K, Mocellin S, Vetvicka V S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Stewart AF. Clinical practice. Hypercalcemia associated with cancer. N Engl J Med. 2005;352:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 639] [Cited by in RCA: 514] [Article Influence: 25.7] [Reference Citation Analysis (1)] |
| 2. | Albright F. Case 27461. N Engl J Med. 1941;225:789-791. [DOI] [Full Text] |
| 3. | Uchimura K, Mokuno T, Nagasaka A, Hayakawa N, Kato T, Yamazaki N, Kobayashi T, Nagata M, Kotake M, Itoh M. Lung cancer associated with hypercalcemia induced by concurrently elevated parathyroid hormone and parathyroid hormone-related protein levels. Metabolism. 2002;51:871-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Lumachi F, Zucchetta P, Marzola MC, Boccagni P, Angelini F, Bui F, D’Amico DF, Favia G. Advantages of combined technetium-99m-sestamibi scintigraphy and high-resolution ultrasonography in parathyroid localization: comparative study in 91 patients with primary hyperparathyroidism. Eur J Endocrinol. 2000;143:755-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 102] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Shah S, Win Z, Al-Nahhas A. Multimodality imaging of the parathyroid glands in primary hyperparathyroidism. Minerva Endocrinol. 2008;33:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Doyle MA, Malcolm JC. An unusual case of malignancy-related hypercalcemia. Int J Gen Med. 2013;7:21-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Imoto Y, Muguruma N, Kimura T, Kaji M, Miyamoto H, Okamura S, Ito S, Nakasono M, Hirokawa M, Sano T. [A case of parathyroid hormone-related peptide producing gallbladder carcinoma presenting humoral hypercalcemia of malignancy]. Nihon Shokakibyo Gakkai Zasshi. 2007;104:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Watanabe Y, Ogino Y, Ubukata E, Sakamoto Y, Matsuzaki O, Shimizu N. A case of a gallbladder cancer with marked hypercalcemia and leukocytosis. Jpn J Med. 1989;28:722-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Cuadrado Gómez LM, Audibert Mena L, Pontes Navarro JC, Medina Iglesias P. [Hypercalcemia as paraneoplastic syndrome in gallbladder carcinoma. Presentation of a case]. Med Clin (Barc). 1988;91:557-558. [PubMed] |
| 10. | Villabona CM, Esteve M, Vidaller A, Escobedo AP, Pac MP, Petriz L. Hypercalcemic crisis in gallbladder cancer. Acta Gastroenterol Belg. 1986;49:532-535. [PubMed] |
| 11. | Koyama Y, Ishijima H, Ishibashi A, Katsuya T, Ishizaka H, Aoki J, Endo K. Intact PTH-producing hepatocellular carcinoma treated by transcatheter arterial embolization. Abdom Imaging. 1999;24:144-146. [PubMed] |
| 12. | Brennan SC, Thiem U, Roth S, Aggarwal A, Fetahu ISh, Tennakoon S, Gomes AR, Brandi ML, Bruggeman F, Mentaverri R. Calcium sensing receptor signalling in physiology and cancer. Biochim Biophys Acta. 2013;1833:1732-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |