Published online Mar 24, 2023. doi: 10.5306/wjco.v14.i3.131
Peer-review started: September 21, 2022
First decision: November 14, 2022
Revised: November 27, 2022
Accepted: February 21, 2023
Article in press: February 21, 2023
Published online: March 24, 2023
Gastrointestinal stromal tumors (GISTs) are the most frequent mesenchymal tumors of gastrointestinal tract. The most common sites of metastases are the liver and the peritoneum, whereas breast metastases from GIST are extremely rare. We present a second case of GIST breast metastasis.
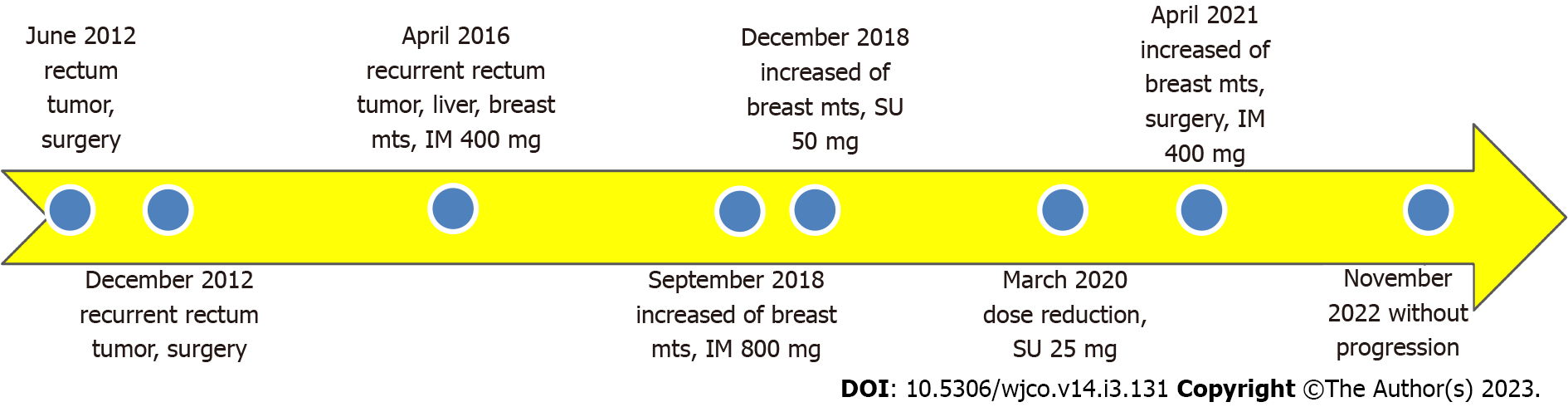
We found a case of breast metastasis from rectum GIST. A 55-year-old female patient presented with rectum tumor with multiply liver lesions and metastasis in the right breast. Abdominal-perineal extirpation of rectum was performed, histology and immunohistochemistry study showed GIST, mixed type with CD117 and DOG-1 positive staining. The patient was taking imatinib 400 mg for 22 mo with stable disease. Because of growth of the breast metastasis the treatment was changed twice: The dose of imatinib was doubled with further progression in the breast lesion and then the patient was receiving sunitinib for 26 mo with partial response in the right breast and stable disease in the liver lesions. The breast lesion increased and right breast resection was done – surgery on local progression, the liver metastases were stable. Histology and immunohistochemistry studies revealed GIST metastasis, CD 117 and DOG 1 positive with KIT exon 11 mutation. After surgery the patient resumed imatinib. Until now the patient has been taking imatinib 400 mg for 19 mo without progression, last follow up was in November 2022.
GISTs breast metastases are extremely rare, we described the second case. At the same time second primary tumors have been reported frequently in patients diagnosed with GISTs and breast cancer is one of the most common second primary tumors in patients with GISTs. That is why it is very important to distinguish primary from metastatic breast lesions. Surgery on local progression made it possible to resume less toxic treatment.
Core Tip: We presented the second case of gastrointestinal stromal tumor (GIST) metastasis to the breast, which is a very extraordinary condition. The most common metastatic sites of GIST are the liver and the peritoneum and at the same time metastasis to the breast from extramammary carcinomas is extremely rare and in this clinical situation it is obligatory to exclude breast cancer. Our patient received two lines of treatment due to metastatic disease and had a local progression on imatinib and sunitinib therapy, growth only lesion in the breast, we removed increased metastasis (surgery on local progression), that allowed to return to less toxic treatment, the patient resumed imatinib until now.
- Citation: Filonenko D, Karnaukhov N, Kvetenadze G, Zhukova L. Unusual breast metastasis of gastrointestinal stromal tumor: A case report and literature review. World J Clin Oncol 2023; 14(3): 131-137
- URL: https://www.wjgnet.com/2218-4333/full/v14/i3/131.htm
- DOI: https://dx.doi.org/10.5306/wjco.v14.i3.131
Gastrointestinal stromal tumors (GISTs) are rare tumors, with an incidence 1%-2% and at the same time are the most frequent mesenchymal tumors of gastrointestinal tract[1]. Approximately 10% to 20% of patients present with metastatic disease[2]. Many evidences showed that gastrointestinal tumors can metastasize to other parts of the body[3]. The most common metastatic sites of GISTs are the liver (60%-70%) and the peritoneum (20%-30%)[4]. Lung metastases (2%-9%), bone and soft tissue (1%-6%) and skin (1%) can occur but very rare. Casuistic bizzare cases of GISTs metastasis to brain[5], core[6], ovary[7,8], and breast[9] are described in the literature. We made a literature review, breast metastases from GIST have been previously described only in one case.
Breast tumors are usually primary. The incidence of metastatic spread from extramammary sites to the breast varies between 0.4% and 1.5% of all breast malignancies. The breast is considered to be resistant to metastasis because it contains large areas of fibrous tissue with a relatively low supply of blood. Most common malignancies that metastasize into the breast are lymphoma, leukemia, melanoma and carcinomas of stomach, ovary, lung, kidney and others[10-12].
In the article we report a second case of GIST patient presenting breast metastasis, highlighting the pathological/molecular features of this unusual site of metastatic presentation and the clinical implications.
The 55-year-old female complained of the tumor in her right breast.
In April 2016 55-year-old female patient presented with recurrent rectum tumor. Abdominal-perineal extirpation of rectum was performed, histology and immunohistochemistry study showed GIST, mixed type with CD117 and DOG-1 positive staining. After the surgery computer tomography (CT) revealed multiply cystic liver lesions that were estimated as metastases, biopsy was not done. At the same time, the patient found lesion in her right breast 30 mm, biopsy was not performed. The patient was taking imatinib 400 mg from June 2016 until August 2018 for 22 mo with stable disease.
In September 2018 Lesion in the right breast increased, liver lesions were stable and the dose of imatinib was doubled, the patient received imatinib 800mg from September until December 2018 with further growth of breast lesion. From December 2018 until March 2020 for 15 mo the patient was receiving sunitinib 50 mg 4/2 regiment. In March 2020 the dose of sunitinib was reduced to 25 mg every day without a break because of hand–food skin reaction grade 2 and then until February 2021 for 11 mo the patient continued the treatment with partial response lesion in the right breast and stable disease in the liver lesions. The toxicity of modified regiment was acceptable. The patient became hypothyroid and received levothyroxine 25 mcg.
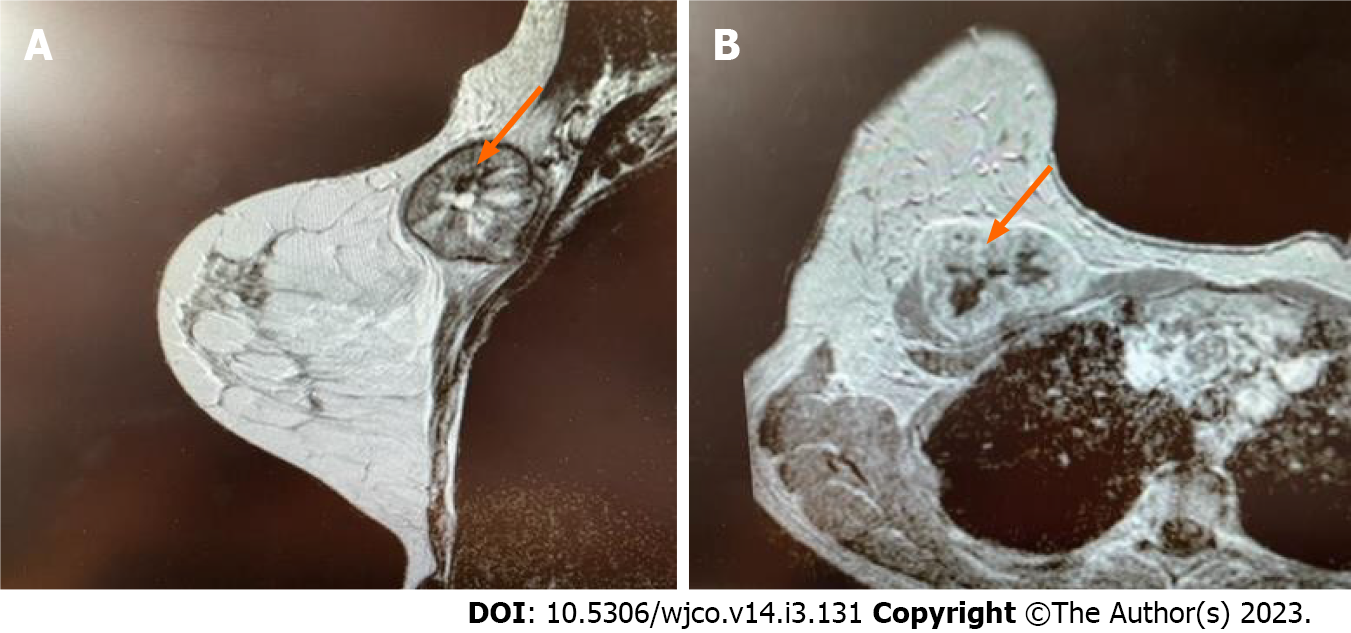
In August 2020 breast ultrasound and magnetic resonance imaging were done at the first time and revealed heterogeneous lesion 47 mm on the border of the upper quadrants of the right breast with central zone of necrosis and peripheral vascularization, BIRADS 5 (Figure 1). The biopsy of the right breast was done to exclude primary breast cancer, histology and immunohistochemistry showed metastasis of GIST, mixed type, 10 mitoses with CD117 and DOG -1 positive staining.
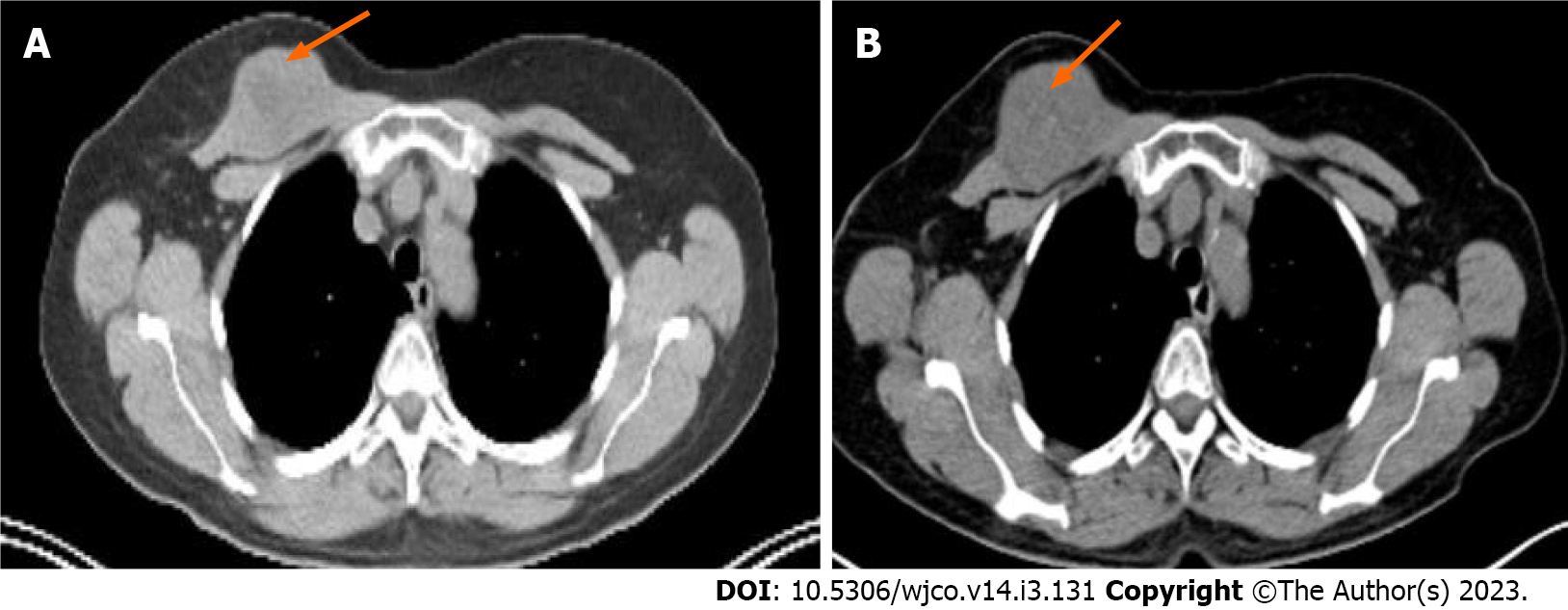
In February 2021 control positron emission tomography-computed tomography (PET-CT) in comparison with September 2020 was obtained and demonstrated progression in the right breast lesion, size increased from 39 mm to 48 mm and FDG uptake increased from 7 to 12 and invasion to the large pectoral muscle was detected (Figure 2). The multiply liver metastases were stable.
The patient had a rectum leiomyoma resection twice in 2012 and 2013 then the patient was on follow up until April 2016.
The patient's other medical history was not noteworthy.
In the right breast on the border of the upper quadrants the solid lesion was revealed, 50 mm in size.
Laboratory testing showed any clinically significant abnormalities.
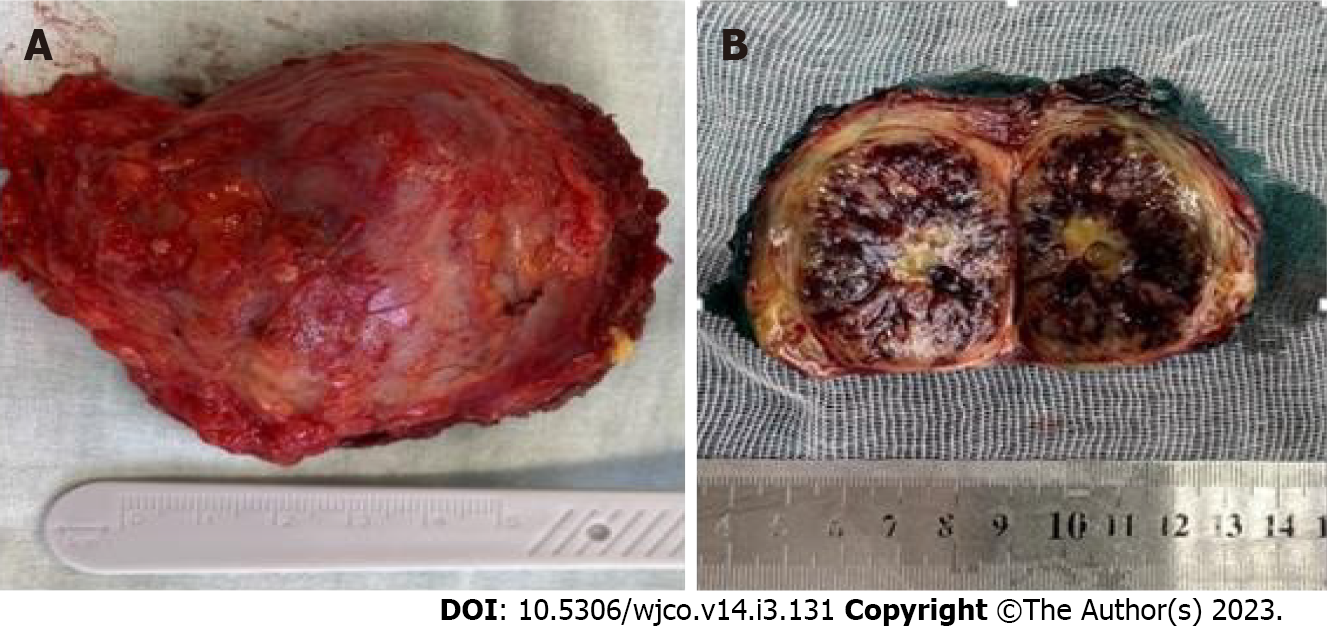
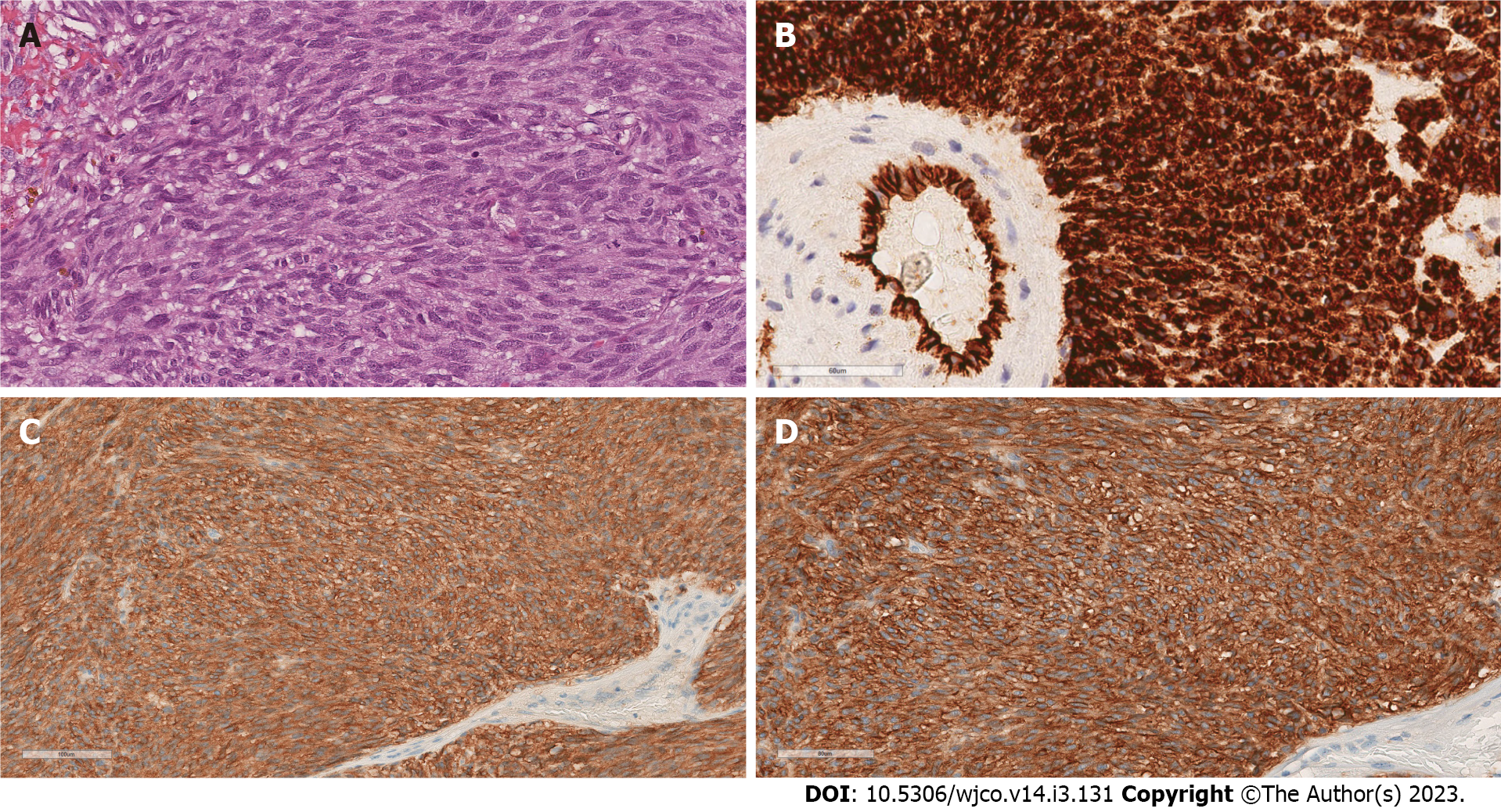
In April 2021, histology and immunohistochemistry studies showed tumor macroscopical size 50 mm with thick fibrous capsule, with histologically negative margins (Figure 3); microscopic examination showed predominantly epithelioid type with focuses of spindle cell that occupied 15% of the square, with prominent hyperchromatic nuclei, high mitotic index (72 mitoses per 50 HPF), small foci of necrosis and large hemorrhagic areas; immunohistochemistry study showed immunophenotype typical for GIST: Strong cytoplasmic expression CD34, membrane-cytoplasmic expression CD117 and DOG-1 (Figure 4).
The clinical situation was estimated as local progression: increase of breast lesion and stable of the liver lesions. Because of growth of the breast metastasis the treatment was changed twice: The patient received double dose of imatinib and sunitinib. Taking into account that the patient had local progression we decided to remove increasing lesion.
The final diagnosis was local progression: Increase of breast lesion and stable of the liver lesions.
In April 2021 right breast resection with partial resection of large pectoral muscle was done. The patient had undergone surgery in 2012, 2013 and 2016 in different clinics, unfortunately histology materials were lost and we had no opportunity to compare histological specimens.
Molecular analysis was performed on the breast metastasis by direct Sanger sequencing and revealed a KIT exon 11 mutation, with a consequent 557-559 deletion.
After surgery we decided to resume imatinib. Previously we changed treatment because of the growth of breast lesion (increased imatinib dose, prescribed sunitinib) and then we removed increased metastasis that is why we decided to return to less toxic treatment.
From April 2021 until now patient has been taking imatinib for 19 mo without progression, PET-CT was done in November 2022. By November 2022 the live duration with metastatic GIST is 77 mo (Figure 5).
We made a literature review, breast metastases from GIST have been previously described only in one case[9]. Hasbay et al[9] reported the clinical case of 46-year-old women with metastases of GIST to liver, bone, abdominal lymph nodes and left breast. We reported the second case of GIST metastases to the breast.
In this case we came across with diagnostic challenges because the most common metastatic sites of GIST are the liver and the peritoneum and at the same time metastasis to the breast from extra
Recently, there is an increasing evidence regarding the association of sporadic GISTs with second neoplasia. In a systematic review and meta-analysis conducted the rate of secondary tumors with GISTs was reported to be 20%[14]. Breast cancers are the most common malignancies together with GISTs.
Taking into account that breast metastasis from GISTs are extremely rare and that second tumors including breast cancer are common, at first in this clinical situation it is obligatory to exclude breast cancer that we have done.
Our patient had a local progression, growth only lesion in the breast, we removed increased metastasis that allowed us to return to less toxic treatment, the patient resumed imatinib. The critical question of whether surgery provides additional benefit over remaining on tyrosine kinase inhibitors (TKIs) therapy alone without surgical resection is unanswered. Randomized trials failed to recruit quickly enough to meet target accrual. In the absence of randomized trials, single-institution and multi-institutional retrospective studies document long-term disease control and longer overall survival for selected patients who undergo metastasectomy of increased lesions while other lesions under control (local progression) on imatinib therapy. Removal of increased metastases let to continue imatinib therapy and not to change the TKIs that have less efficacy and not so favorable profile of toxicity. The median time to progression on sunitinib therapy is 6 mo, on regorafenib only 4 mo. Fairweather et al[15] published the largest series of patients with metastatic GIST treated with TKI undergoing surgical resection (n = 323). The median time to progression during imatinib therapy on local progression was 47 mo from the start of imatinib and 11 mo from cytoreductive surgery, removal increasing lesions[15]. These data are consistent with the result of treatment of our patient; the duration of imatinib therapy after surgery is 19 mo that is more than four times higher than the median PFS on regorafenib therapy.
In conclusion, breast metastases from GISTs are very rare, but it is clinically very important to distinguish primary from metastatic breast lesions.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Guo F, China; Machaku D, Tanzania; Wang Z, China; Zhao G, China S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Miettinen M, Lasota J. Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1185] [Cited by in F6Publishing: 1137] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 2. | Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumors: recent advances in understanding of their biology. Hum Pathol. 1999;30:1213-1220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 559] [Cited by in F6Publishing: 512] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 3. | Tulsi R, Ul Haque MM, Hanif FM, Devi A, Mubarak M, Hassan Luck N. Metastasis of Duodenal Adenocarcinoma to the Urinary Bladder Presenting as Hematuria. J Transl Int Med. 2021;9:143-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Liu P, Tan F, Liu H, Ge J, Liu S, Lei T, Zhao X. Skin Metastasis of Gastrointestinal Stromal Tumors: A Case Series and Literature Review. Cancer Manag Res. 2020;12:7681-7690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Wong CS, Chu YC. Intra-cranial metastasis of gastrointestinal stromal tumor. Chin Med J (Engl). 2011;124:3595-3597. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Bashir U, Qureshi A, Khan HA, Uddin N. Gastrointestinal stromal tumor with skeletal muscle, adrenal and cardiac metastases: an unusual occurrence. Indian J Pathol Microbiol. 2011;54:362-364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | De Leo A, Nannini M, Dondi G, Santini D, Urbini M, Gruppioni E, De Iaco P, Perrone AM, Pantaleo MA. Unusual bilateral ovarian metastases from ileal gastrointestinal stromal tumor (GIST): a case report. BMC Cancer. 2018;18:301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Irving JA, Lerwill MF, Young RH. Gastrointestinal stromal tumors metastatic to the ovary: a report of five cases. Am J Surg Pathol. 2005;29:920-926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Hasbay B, Aytaç HÖ, Kayaselçuk F, Torun N. An Unusual Gastrointestinal Stromal Tumor Presentain: Breast, Liver and Lymph Node Metastasis. Eur J Breast Health. 2017;13:216-218. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 10. | McFarlane ME. Metastasis to the breast: a rare site for secondary malignancy. Int J Surg. 2006;4:204-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Klingen TA, Klaasen H, Aas H, Chen Y, Akslen LA. Secondary breast cancer: a 5-year population-based study with review of the literature. APMIS. 2009;117:762-767. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Wang Y, Hou K, Jin Y, Bao B, Tang S, Qi J, Yang Y, Che X, Liu Y, Hu X, Zheng C. Lung adenocarcinoma-specific three-integrin signature contributes to poor outcomes by metastasis and immune escape pathways. J Transl Int Med. 2021;9:249-263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 13. | Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8287] [Cited by in F6Publishing: 10117] [Article Influence: 3372.3] [Reference Citation Analysis (2)] |
| 14. | Petrelli F, Tomasello G, Barni S, Varricchio A, Costanzo A, Rampulla V, Cabiddu M, Turati L, Russo A, Seghezzi S, Passalacqua R, Ghidini M. Risk of second primary tumors in GIST survivors: A systematic review and meta-analysis. Surg Oncol. 2019;29:64-70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Fairweather M, Balachandran VP, Li GZ, Bertagnolli MM, Antonescu C, Tap W, Singer S, DeMatteo RP, Raut CP. Cytoreductive Surgery for Metastatic Gastrointestinal Stromal Tumors Treated With Tyrosine Kinase Inhibitors: A 2-institutional Analysis. Ann Surg. 2018;268:296-302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |