Published online Feb 26, 2017. doi: 10.4331/wjbc.v8.i1.81
Peer-review started: October 7, 2016
First decision: November 10, 2016
Revised: December 28, 2016
Accepted: January 11, 2017
Article in press: January 14, 2017
Published online: February 26, 2017
It is worthwhile to measure serum thyroglobulin (TG) level in thyroid cancer before subjecting patients to surgery for two reasons. Firstly, if the level is high, it may give a clue to the local and metastatic tumour burden at presentation; secondly, if the level is normal, it identifies the patients who are unlikely to show rising TG levels in the presence of thyroid cancer. Those who have high serum TG before surgery will show up recurrence as rising serum TG during the postoperative period. Those who do not have high serum TG before surgery will not show up rising serum TG in the presence of recurrent disease. In the latter situation, normal TG level gives only a false reassurance regarding recurrence of disease. Nevertheless, rising serum TG during the postoperative period must be interpreted cautiously because this could be due to the enlargement of non-cancerous residual thyroid tissue inadvertently left behind during surgery.
Core tip: Although serum thyroglobulin (TG) is widely used as a tool to detect recurrence of thyroid cancer, it is widely held that preoperative TG measurement is unnecessary. It is true that preoperative TG level is hardly of much diagnostic value, but without a preoperative TG report, it is not possible to safely utilize serial serum TG subsequently as a monitoring tool. Routine measurement of serum TG before surgery is, therefore, recommended.
- Citation: Indrasena BSH. Use of thyroglobulin as a tumour marker. World J Biol Chem 2017; 8(1): 81-85
- URL: https://www.wjgnet.com/1949-8454/full/v8/i1/81.htm
- DOI: https://dx.doi.org/10.4331/wjbc.v8.i1.81
Serial measurement of thyroglobulin (TG) is being practised by many clinicians to detect recurrence of thyroid cancer after surgery[1-3]. Apart from that, there is hardly any use of TG as a diagnostic modality of thyroid cancer because it is not tumour specific[4]. The serum level of TG reflects the thyroid tissue burden in the body regardless of underlying pathology whether benign or malignant. Since the serum levels are proportional to the volume of thyroid tissue, it can be used successfully to evaluate the “cancer burden” at presentation as well as to assess the adequacy of surgery, monitor the recurrences and progression of disease before and after cancer treatment. Its use as a monitoring tool is only valid provided certain precautions are seriously taken into account. Otherwise, false reassurance is inevitable in the presence of on going disease.
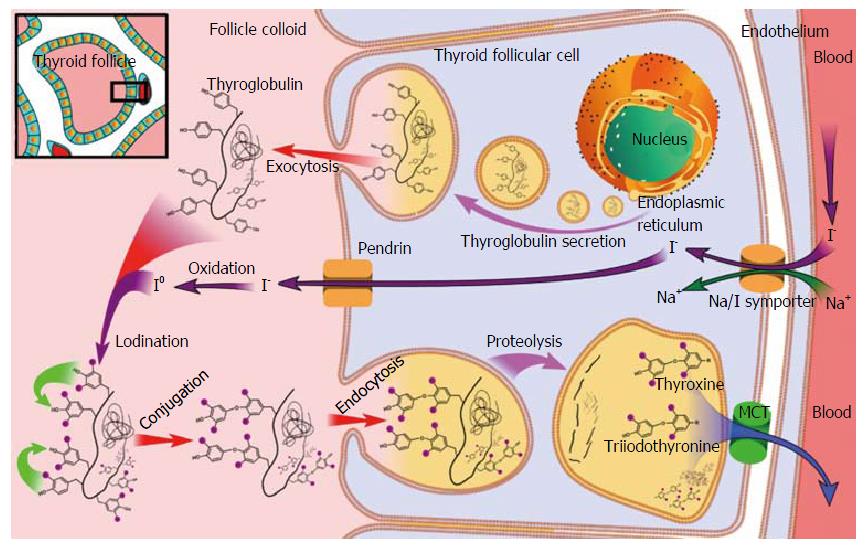
TG is a glycoprotein molecule synthesised exclusively by the thyroid follicular cells. These are stored as colloid within the thyroid follicles, iodinated and degraded to thyroxin and tri-iodothyronine. The whole process is regulated by thyroid stimulating hormone (TSH) (Figure 1).
TG in serum has a half-life of 65 h[5]. The serum level TG is proportional to the volume of thyroid tissue in the body at a rate 1 ng/mL per 1 g of thyroid mass. Since the size of the normal thyroid gland is 20-25 g, the reference range has to be generally about 20 to 25 ng/mL. However, the normal serum TG level depends on the gender and the level of iodine intake of the patient. The gender specific reference range has been given as 1.40-29.2 ng/mL for males and 1.50-38.5 ng/mL for females[6]. In countries with iodine deficiency the reference range may be higher[7,8]. This is because of elevated TSH in serum in the presence of iodine deficiency; TSH stimulates the thyroid follicular cells to synthesise more TG. Apart from gender and iodine intake, the measured TG level is also influenced by autoantibodies against TG (anti-TGAb), cigarette smoking and TSH status unrelated to iodine intake. The measured serum TG levels are masked by the presence of anti-TGAb in blood. Anti-TGAb bind to the TG molecules masking the epitopes on the TG molecule to which the antibodies of the radio immuno assay (RIA) test bind. As a result, the measured TG level by RIA in such patients, will be falsely low. Anti-TGAb can be seen in cases of Hashimoto’s disease, Graves’ disease, 20% of patients with thyroid carcinoma[9], and 10% of normal population without any thyroid disease[10].
TG can be elevated in any thyroid pathology. Serum TG level is proportional to the thyroid mass rather than the type of pathology[8]. As a guide, one gram of normal thyroid tissue is equivalent to 1 ng/mL of TG in serum in euthyroid state; in a TSH suppressed state, this is equivalent to 0.5 ng/mL. After total thyroidectomy, theoretically, the level has to drop to zero because no thyroid tissue is expected to leave behind after total thyroidectomy. Persistent presence of TG after total thyroidectomy, even at low concentrations, points to the possibility of inadequate surgery leading to residual thyroid tissue at the thyroid bed (in the absence of local or distant metastases). After hemithyroidectomy, the preoperative level should theoretically drop to 50% of preoperative value. After near total thyroidectomy, i.e., total lobectomy on one side plus isthmusectomy plus subtotal lobectomy on the other side (leaving behind overall 1/8th of the size of a normal sized gland weighing 25 g), a TG level of 3-4 ng/mL can be expected to present in serum when TSH is normal, and 1.5-2 ng/mL when TSH has been suppressed with high doses of thyroxine.
The serum TG level post surgery reflects the amount of residual thyroid mass. In the absence of metastatic disease, this reflects the size of the thyroid remnant left behind during surgery. Since TG has a half-life close to 3 d, it can be shown that the TG level has to be less than 0.5 ng/mL at the end of three weeks after total or near total thyroidectomy for a goitre of a size of three times normal. This can be used as a guide to initiate radio active iodine treatment for remnant ablation, the residual thyroid mass being as a result of inadequate surgery or metastatic disease. However, although such a hypothesis carries high positive predictive value, a negative result does not reliably exclude the possibility of residual disease. The TG serum level at 3 wk post surgery not only depends on the residual thyroid mass but also the size of the gland at the time of surgery as well as TG producing capacity of the tumour.
TG can be secreted by differentiated cancer cells of the thyroid. This includes nearly two thirds of differentiated thyroid cancers (follicular neoplasms, all papillary carcinomas, Hurthle cell tumours of the thyroid), up to 50% of poorly differentiated and anaplastic carcinomas of thyroid and some medullary carcinomas. The cancerous nodules can be stained with immunohistochemical methods to specifically demonstrate TG. TG has been demonstrated in cancerous follicles both in the thyroid as well as in metastatic deposits in lymph nodes and elsewhere.
The use of TG as a screening and diagnostic tool of differentiated thyroid cancer is poor (Sensitivity and specificity is 70% and 80% respectively for follicular carcinoma) because both benign and malignant thyroid glands secrete TG[11]. Elevated TG levels can be seen in benign conditions like Graves’ disease and thyroiditis, as well as in thyroid cancer. Further, there is a subset of thyroid cancer patients (12%) whose TG level is low or low-normal as opposed to a minority whose blood level is very high (> 1000 ng/mL). A level > 5000 ng/mL is indicative of metastatic disease[12]. Patients who develop cancer as a result of mutations of TG gene may not express TG even though they have a hypothyroid goitre (high TSH) as well as cancer[13].
Those who have high serum TG one month after thyroidectomy are more likely to develop cancer recurrence, the value being proportional to the burden of remaining metastatic disease[14]. However, high serum TG could be due to distant metastatic disease or incomplete excision of the gland during thyroidectomy. Holsinger et al[15] reported that 57% of patients who were supposed to have had total thyroidectomy for thyroid cancer had residual thyroid tissue at the thyroid bed when tested by postoperative radioactive iodine uptake test. Therefore, the surgeon must be sure that the whole thyroid gland has been removed before utilizing TG as a prognostic indicator. Or else the patient must have undergone remnant ablation with radioactive iodine before TG testing.
TG has been used frequently to monitor recurrent disease after thyroidectomy. Not only the first recurrence but also subsequent recurrences can be detected by monitoring serum TG level. The TG level has to be done every 6 to 12 mo. However, certain points need to be kept in mind when utilizing TG alone as a tumour marker to detect recurrence. TG can rise after thyroidectomy when the residual thyroid gland enlarges even though it does not harbour malignant cells. This could happen after near total thyroidectomy (total lobectomy on one side plus isthmusectomy plus subtotal lobectomy on the other side) when about 4 g of the gland is left behind purposely on one side, or glandular tissue left behind inadvertently in the neck because of difficult thyroidectomy. In such instances, serum TG could give false positive result. Therefore, more often than not, surgeons prefer to subject all patients to remnant ablation therapy after thyroidectomy for cancer. Such patients are more suitable for monitoring by TG than otherwise.
It may not be able to see high serum TG after thyroidectomy if the TG level before surgery had been low or normal. Therefore, it is necessary to recognise patients who would not have rising TG in the presence of recurrence before using TG as a tumour marker. This can only be done if the serum TG level before the surgery is known. Those who have normal or low serum TG before surgery will not show rising serum TG when there is recurrence of disease[16]. This happens irrespective of the anti-TGAb status of the patient[17]. Such patients must be offered iodine scintigraphy to detect recurrence. Furthermore, there is a possibility of transforming a differentiated thyroid cancer to anaplastic variety over time[18]. In such a case, TG will not rise in the presence of recurrence.
It may take nearly one month (7 to 10 t1/2) for the TG to disappear from the circulation after total thyroidectomy in the absence of metastases[5].
Since there is a theoretical possibility of releasing TG in to the circulation following trauma, it would be a valid precaution to measure TG before FNAC test or 2 wk after FNAC, although there are no references to strongly recommend this approach.
In postoperative patients, thyroxin must preferably be stopped at least six weeks before the measurement of serum TG if the patient has been on thyroxine or two weeks before if the patient has been on liothyronine (tri-iodothyronine). The idea is to allow TSH level to rise from the suppressive levels to higher levels making the residual cancer tissue to synthesise and secrete TG stimulated by TSH. This is also the standard practice in postoperative use of radioactive iodine for diagnostic and therapeutic purposes. Alternatively, to minimize the risks associated with stopping thyroxin for six weeks, thyroxine can be stopped only for three weeks before the TG test, but the test may have to be repeated after six weeks of cessation of thyroxin if TG and TSH are normal[19]. Another alternative is to stop thyroxine six weeks before and to put the patient on liothyronine for four weeks and do the test two weeks later after stopping liothyronine. Liothyronine has a shorter half-life than thyroxine. Recombinant human TSH can also be used, instead, to stimulate residual thyroid tissue without stopping thyroid suppression treatment.
Interpretation of serum TG measurements could be a quite complex task. It may be elevated in both benign and malignant disease of the thyroid gland. Therefore, its use as a diagnostic tool of cancer is negligible. TG level 3-4 wk post surgery can be used to assess the size of the residual thyroid mass either locally or distally, and guide remnant ablation therapy. Rising levels in the postoperative period could happen due to progression of cancer or growth of residual thyroid tissue at the thyroid bed following inadequate surgery. It may remain normal in malignant thyroid disease both pre and post operatively due to non-secreting varieties of thyroid cancer or due to the presence of anti-TGAb in serum, and such cases could only be detected by checking TG levels before surgery.
The changes of TG that can be expected at different stages of the disease and how different TG levels assist in decision making and the management of thyroid cancer has been summarised in Table 1.
| Stage of disease | Serum TG level | Uses and further action | ||
| Low | Normal | Elevated | ||
| Before surgery | Anti-TGAb or TG non-secreting tumour | TG can not be used subsequently to monitor disease activity | ||
| Benign or malignant thyroid disease | TG can be used subsequently to monitor disease activity | |||
| 3-4 wk after surgery | Anti-TGAb, successful local surgery or no metastatic disease | Do 125-Iodine scan to screen for residual local disease and distant metastases | ||
| Incomplete local surgery, metastatic disease or recurrence | Remnant ablation therapy (131-Iodine or further surgery) is indicated | |||
| Long term follow-up | Anti-TGAb | Do other tests to monitor disease activity | ||
| Cure or stable disease | Disease activity can be monitored by periodic TG measurements | |||
| Recurrence or progression | Further investigations and treatment | |||
Manuscript source: Invited manuscript
Specialty type: Biochemistry and molecular biology
Country of origin: Sri Lanka
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gupta VK, Salvatore B, Shi YF, Xie L S- Editor: Song XX L- Editor: A E- Editor: Li D
| 1. | Ringel MD, Nabhan F. Approach to follow-up of the patient with differentiated thyroid cancer and positive anti-thyroglobulin antibodies. J Clin Endocrinol Metab. 2013;98:3104-3110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Gibelli B, Tredici P, De Cicco C, Bodei L, Sandri MT, Renne G, Bruschini R, Tradati N. Preoperative determination of serum thyroglobulin to identify patients with differentiated thyroid cancer who may present recurrence without increased thyroglobulin. Acta Otorhinolaryngol Ital. 2005;25:94-99. [PubMed] [Cited in This Article: ] |
| 3. | Frilling A, Görges R, Tecklenborg K, Gassmann P, Bockhorn M, Clausen M, Broelsch CE. Value of preoperative diagnostic modalities in patients with recurrent thyroid carcinoma. Surgery. 2000;128:1067-1074. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 69] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Yalcin S, Ulger BV, Parlak O, Ucar AE, Sarikaya SM, Ozer M, Korukluoglu B, Yalcin B, Kusdemir A. The role of preoperative serum thyroglobulin and thyroid auto-antibody levels before histopathological diagnosis of thyroid cancers. Turk J Med Sci. 2011;41:487-493. [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 5. | Hocevar M, Auersperg M, Stanovnik L. The dynamics of serum thyroglobulin elimination from the body after thyroid surgery. Eur J Surg Oncol. 1997;23:208-210. [PubMed] [Cited in This Article: ] |
| 6. | Giovanella L, Imperiali M, Ferrari A, Palumbo A, Furlani L, Graziani MS, Castello R. Serum thyroglobulin reference values according to NACB criteria in healthy subjects with normal thyroid ultrasound. Clin Chem Lab Med. 2012;50:891-893. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ovadia YS, Gefel D, Turkot S, Aharoni D, Fytlovich S, Troen AM. Elevated Serum Thyroglobulin and Low Iodine Intake Are Associated with Nontoxic Nodular Goiter among Adults Living near the Eastern Mediterranean Coast. J Thyroid Res. 2014;2014:913672. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Knudsen N, Bülow I, Jørgensen T, Perrild H, Ovesen L, Laurberg P. Serum Tg--a sensitive marker of thyroid abnormalities and iodine deficiency in epidemiological studies. J Clin Endocrinol Metab. 2001;86:3599-3603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Ringel MD, Ladenson PW. Controversies in the follow-up and management of well-differentiated thyroid cancer. Endocr Relat Cancer. 2004;11:97-116. [PubMed] [Cited in This Article: ] |
| 10. | Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87:489-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2027] [Cited by in F6Publishing: 2065] [Article Influence: 93.9] [Reference Citation Analysis (1)] |
| 11. | Hocevar M, Auersperg M. Role of serum thyroglobulin in the pre-operative evaluation of follicular thyroid tumours. Eur J Surg Oncol. 1998;24:553-557. [PubMed] [Cited in This Article: ] |
| 12. | Oltmann SC, Leverson G, Lin SH, Schneider DF, Chen H, Sippel RS. Markedly elevated thyroglobulin levels in the preoperative thyroidectomy patient correlates with metastatic burden. J Surg Res. 2014;187:1-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Agretti P, De Marco G, Di Cosmo C, Ferrarini E, Montanelli L, Bagattini B, Vitti P, Tonacchera M. Congenital hypothyroidism caused by a novel homozygous mutation in the thyroglobulin gene. Eur J Pediatr. 2013;172:959-964. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Lima N, Cavaliere H, Tomimori E, Knobel M, Medeiros-Neto G. Prognostic value of serial serum thyroglobulin determinations after total thyroidectomy for differentiated thyroid cancer. J Endocrinol Invest. 2002;25:110-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Holsinger FC, Ramaswamy U, Cabanillas ME, Lang J, Lin HY, Busaidy NL, Grubbs E, Rahim S, Sturgis EM, Lee JE. Measuring the extent of total thyroidectomy for differentiated thyroid carcinoma using radioactive iodine imaging: relationship with serum thyroglobulin and clinical outcomes. JAMA Otolaryngol Head Neck Surg. 2014;140:410-415. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Brendel AJ, Lambert B, Guyot M, Jeandot R, Dubourg H, Roger P, Wynchauk S, Manciet G, Lefort G. Low levels of serum thyroglobulin after withdrawal of thyroid suppression therapy in the follow up of differentiated thyroid carcinoma. Eur J Nucl Med. 1990;16:35-38. [PubMed] [Cited in This Article: ] |
| 17. | Westbury C, Vini L, Fisher C, Harmer C. Recurrent differentiated thyroid cancer without elevation of serum thyroglobulin. Thyroid. 2000;10:171-6. [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Camargo R, Limbert E, Gillam M, Henriques MM, Fernandes C, Catarino AL, Soares J, Alves VA, Kopp P, Medeiros-Neto G. Aggressive metastatic follicular thyroid carcinoma with anaplastic transformation arising from a long-standing goiter in a patient with Pendred’s syndrome. Thyroid. 2001;11:981-988. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Golger A, Fridman TR, Eski S, Witterick IJ, Freeman JL, Walfish PG. Three-week thyroxine withdrawal thyroglobulin stimulation screening test to detect low-risk residual/recurrent well-differentiated thyroid carcinoma. J Endocrinol Invest. 2003;26:1023-1031. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Mikael Häggström. Medical gallery of Mikael Häggström. Wiki Journal of Medicine. 2014;. [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 31] [Article Influence: 3.1] [Reference Citation Analysis (1)] |