Copyright
©The Author(s) 2020.
World J Biol Chem. Sep 27, 2020; 11(2): 30-51
Published online Sep 27, 2020. doi: 10.4331/wjbc.v11.i2.30
Published online Sep 27, 2020. doi: 10.4331/wjbc.v11.i2.30
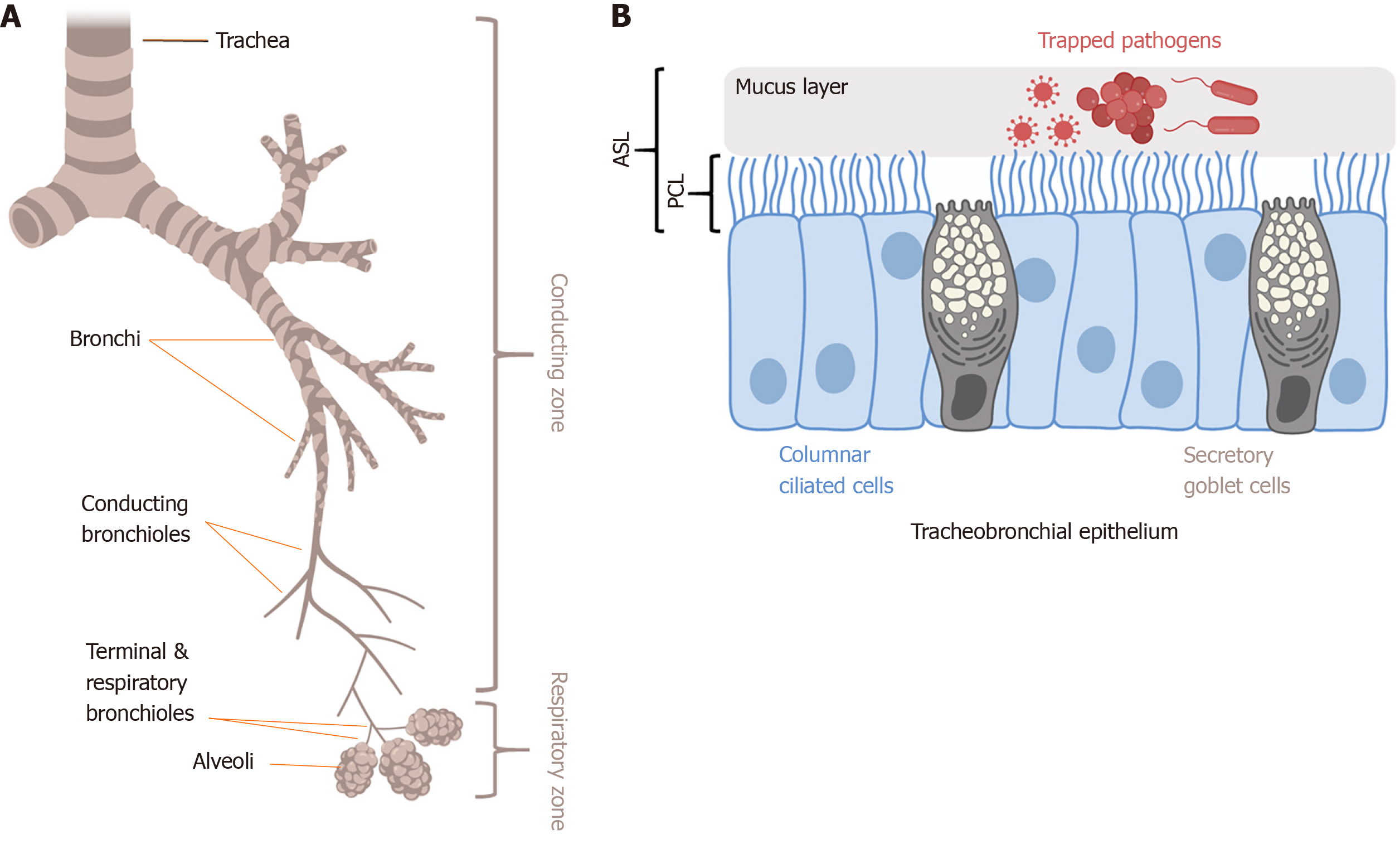
Figure 2 Mucociliary clearance and innate immunity in the lung.
A: Trachea, bronchi, and conducting bronchioles comprise the conducting zone of the airways; B: The conducting airway epithelium is lined with columnar motile ciliated cells and secretory goblet cells. Goblet cells secrete mucins like MUC5AC that polymerize to form mucus, which traps inhaled pathogens and debris; The mucus layer rides on top of a less viscous PCL composed of salt, water, and antimicrobials; Together, the mucus and PCL comprise the airway surface liquid; Coordinated metachronal beating of the motile cilia within the PCL layer pushes the sticky mucus layer up to respiratory tree to the oropharynx, where it is expectorated or swallowed; This process is termed MCC, and is the physical defense of the airway against infection; Epithelial cells also secrete antimicrobial peptide and radicals (NO, H2O2) to directly kill pathogens and produce cytokines and chemokines to activate inflammation; Shown is a representative diagram of tracheal or bronchial epithelium; In lower conducting airways (non-cartilaginous bronchioles < approximately 1 mm in diameter), secretory club cells (also known as bronchiolar exocrine cells) are found instead of goblet cells; As described in the text, there are several potential mechanisms by which protein kinase B may regulate MCC and other innate immune pathways. Figure made using Biorender.com. PCL: Periciliary layer; MCC: Mucociliary clearance; MUC5AC: Mucin 5AC.
- Citation: Gopallawa I, Lee RJ. Targeting the phosphoinositide-3-kinase/protein kinase B pathway in airway innate immunity. World J Biol Chem 2020; 11(2): 30-51
- URL: https://www.wjgnet.com/1949-8454/full/v11/i2/30.htm
- DOI: https://dx.doi.org/10.4331/wjbc.v11.i2.30