Published online Feb 27, 2016. doi: 10.4240/wjgs.v8.i2.173
Peer-review started: May 21, 2015
First decision: August 4, 2015
Revised: September 16, 2015
Accepted: October 16, 2015
Article in press: October 17, 2015
Published online: February 27, 2016
Processing time: 283 Days and 12.4 Hours
Pneumatosis intestinalis (PI) often represents a benign condition that should not be considered as an argument for surgery. We report a patient with PI and obstructing intussusception who underwent urgent colectomy and review the literatures regarding PI with intussusception. A 20-year-old man presented at our hospital with a 3-d intermittent lower abdominal pain history. He underwent steroid therapy for membranoproliferative glomerulonephritis for 4 years. Computed tomography revealed ascending colon intussusception with air within the wall. Intraoperative colonoscopy revealed numerous soft polypoid masses with normal overlying mucosa and right hemicolectomy was performed. Histological examination of colonic wall sections revealed large cysts in the submucosal layer. The pathological diagnosis was PI. Nine cases of intussusception associated with primary PI have been reported. Although primary PI often represents a benign condition that should not be considered as an argument for surgery, if the case involves intussusception and obstruction, emergent laparotomy should be considered.
Core tip: We report a patient with pneumatosis intestinalis (PI) and obstructing intussusception who underwent urgent colectomy and review the literatures regarding PI with intussusception. A 20-year-old man presented at our hospital with abdominal pain, and has undergone steroid therapy for 4 years. Computed tomography revealed ascending colon intussusception with air within the wall, and colectomy was performed. Histological examination of colonic wall sections revealed large cysts in the submucosal layer. Nine cases of intussusception associated with primary PI have been reported. Although primary PI often represents a benign condition, if the case involves intussusception and obstruction, emergent laparotomy should be considered.
- Citation: Itazaki Y, Tsujimoto H, Ito N, Horiguchi H, Nomura S, Kanematsu K, Hiraki S, Aosasa S, Yamamoto J, Hase K. Pneumatosis intestinalis with obstructing intussusception: A case report and literature review. World J Gastrointest Surg 2016; 8(2): 173-178
- URL: https://www.wjgnet.com/1948-9366/full/v8/i2/173.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i2.173
Pneumatosis intestinalis (PI) is a rare condition characterized by the presence of gas within the wall of the gastrointestinal tract. This condition can result from a wide variety of pathologies, including chronic obstructive lung disease, collagen diseases, necrotizing enterocolitis in premature infants, intestinal infections, ischemic bowel disorders, and immunosuppressive drug therapy[1]. PI often represents a benign condition that should not be considered as an argument for surgery[2]; however, immediate surgery may be required in some life-threatening circumstances such as the presence of bowel obstruction, perforation, or ischemia[3].
Here we describe a case of PI in the ascending colon with obstructing intussusception for which urgent surgery was performed, and review the available published literature on PI with intussusception. Written informed consent was obtained from the patient.
The literature search strategy for this study was based on published systematic review guidelines[4]. Literature databases such as PubMed MEDLINE (National Library of Medicine) were searched from 1980 to 2015 using the following medical subject headings: “PI (or Pneumatosis cystoides intestinalis)” and “intussusception” or “PI (or Pneumatosis cystoides intestinalis)” and “invagination”. In addition, references within the retrieved articles were reviewed. We identified 24 manuscripts using this search strategy and selected 8 case reports for this review. Nineteen articles were excluded because their content was not applicable to this review and 7 articles were excluded because they were not written in English.
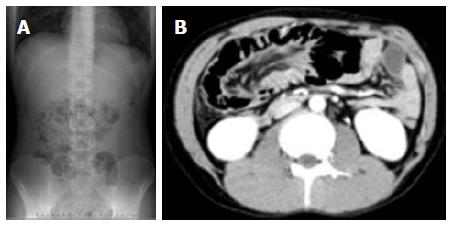
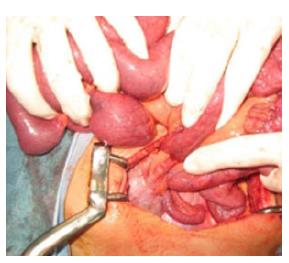
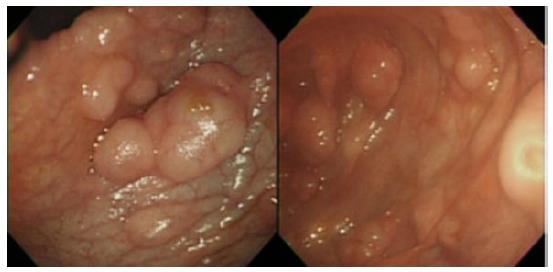
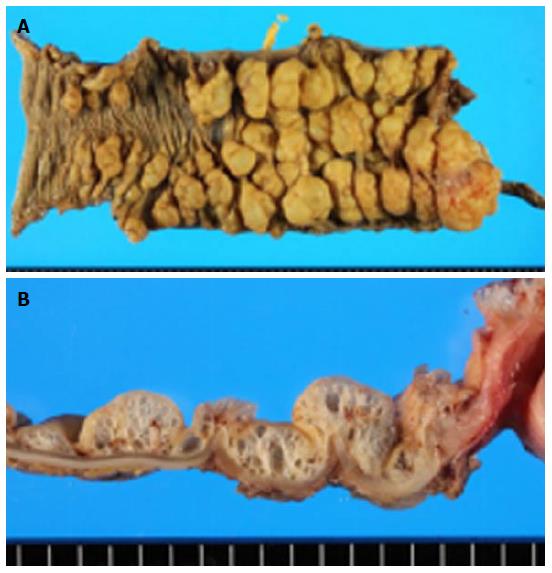
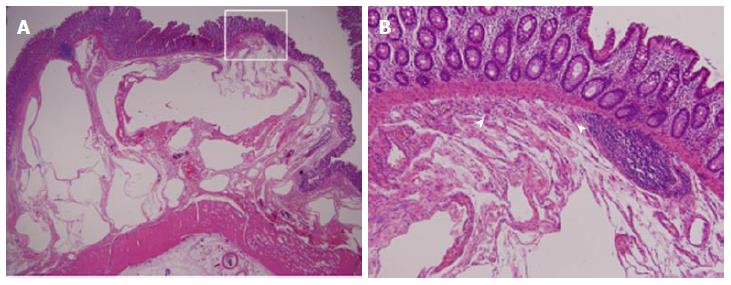
A 20-year-old man presented our hospital with a 3-d history of intermittent lower abdominal pain. He had been on steroid therapy (methylprednisolone 25 mg/d) for membranoproliferative glomerulonephritis for 4 years. A physical examination revealed tenderness in the lower right quadrant of the abdomen. His body temperature was 37.7 °C and pulse was 81 beats per minute. All serum levels tested were within the normal range, with the exception of serum total bilirubin (1.5 mg/dL; normal range, 0.3-1.2 mg/dL). White blood cells (WBCs) (21000/μL), hemoglobin concentration (17.1 g/dL), and the C-reactive protein concentration (0.5 mg/dL) were also elevated, indicating acute inflammation and dehydration, with a level of base excess of 2.4 mmol/L. Abdominal X-ray showed multiple air-filled lucencies in the right upper quadrant and multiple distended loops of small bowel with fluid (Figure 1A). Computed tomography (CT) revealed intussusception of the ascending colon with air within the wall (Figure 1B). We performed an urgent laparotomy under the diagnosis of acute abdomen with obstructing intussusception. The colo-colic intussusception that was caudal to the polypoid lesion easily resolved using Hutchinson’s maneuver and soft polypoid masses were palpable from the cecum to the ascending colon (Figure 2). Intraoperative colonoscopy revealed the presence of numerous soft polypoid masses with normal overlying mucosa (Figure 3). A right hemicolectomy was performed because other polyposis diseases or intussusception relapse could not be ruled out, and to help make a final pathological diagnosis. A gross examination showed that the mucosa of the resected colon appeared normal with no evidence of ulceration or ulcer-related lesions, but instead a number of soft, yellowish cystic masses (Figures 4). A histological examination of sections of the colonic wall revealed large cysts in the submucosal layer (Figure 5A). The cysts were empty, but were surrounded by a distinct fibrous wall and were lined by macrophages that frequently coalesced to form multinucleated giant cells (Figure 5B). Based on these findings, the patient was diagnosed with pneumatosis cystoides intestinalis. The postoperative course was uneventful and the patient was discharged on postoperative day 9. No recurrence was noted on radiographic imaging performed on postoperative 14 mo.
Classically, PI can be subdivided into 2 distinct groups: primary PI, representing 15% of cases, and secondary PI, representing 85% of cases[5]. Secondary PI, where the gas accumulates as linear collections and reflects a pathological condition, has been attributed to endoscopic procedures, immunological disturbances, bowel mucosal disruptions, and intra-abdominal pathologies. In contrast to secondary PI, primary PI is characterized by intramural gas that is cystic and benign in nature and does not always require urgent laparotomy[6]. Although PI may occur in association with acquired immunodeficiency[7], transplant status[8], cancer treatment[9,10], scleroderma[11], cystic fibrosis[12], systemic lupus[13], inflammatory bowel disease[2], intestinal ischemia[14], colitis[15], or trauma[16], the exact etiology of both primary and secondary PI remains unknown.
There is currently no consensus on the appropriate management of PI, although many mechanical, bacterial, and pulmonary hypotheses have been proposed regarding PI etiopathogenesis, and its management can be challenging for surgeons[17]. Many studies have investigated the use of risk factors as predictors of a compromised bowel and the probable need for surgery, such as patient age and the presence of hypotension, peritonitis, renal failure, or serum lactate levels[18]. Other studies have attempted to create algorithms for PI management that, while helpful, are also tedious and may be difficult to apply clinically in circumstances where the patient requires rapid evaluation[19]. In this case, we performed urgent laparotomy because he had intestinal obstruction due to intussusception and several inflammatory symptoms.
Although the course of primary PI may be benign or may not frequently result in a need for urgent surgery, laparotomy should be considered in cases with intestinal obstruction due to intussusception. To our knowledge, 9 reported cases, including the present case, had intussusception associated with primary PI (Table 1)[20-27]. The mean patient age was 19.0 ± 16.0 years (range 0-48 years), which is younger than has been reported previously[19]. It is notable that more than 44% of these patients received an immunosuppressive drug, and few patients appeared to have intestinal ischemia. All patients had the intussusception in the colon, particularly on its right side. Five out of 9 patients had co-morbidities, most of which required an immunosuppressive drug. With the exception of the article placed as reference number 22, no other articles referred to the presence of portal venous gas, which often indicates ischemic bowel disease. Only 2 cases experienced successful reduction of the intussusception with barium enema[22,23], although long-term outcomes were not reported. Among the 4 cases with initial successful reduction of the intussusception by colonoscopy or barium enema, all of these patients eventually needed surgery: One case had persistent abdominal pain after solution of intussusception; in one case, the intussusception could not be completely resolved; one case had bowel obstruction; and for one case the indication of surgery was not clearly stated. For the present case, we performed an urgent laparotomy because of bowel obstruction with intussusception of the ascending colon. Right hemicolectomy for this case was performed because of the possibility of there being another polyposis disease present and because relapse of the intussusception could not be ruled out.
| Ref. | Year | Sex | Immunosuppressive drug | Ischemia | PVG | Site | Treatment | Indication of surgery | Co-morbidity |
| Nagata et al[20] | 23 yr | Male | No | No | No | A/C | CS→Surgery | Abdominal pain | None |
| Emanuel et al[21] | 48 yr | Male | NR | NR | NR | D/C | Surgery | Obstruction | Hybrid perineurioma-schwannoma |
| Sugita et al[22] | 5 yr | Female | Yes | No | Yes | A/C | BE | - | CML |
| Stern et al[23] | 32 yr | Male | No | No | No | A/C | BE | - | None |
| Morrison et al[24] | 3 mo | NR | Yes | Yes | NR | T/C | BE→Surgery | could not resolved intussusception | Peter's anomaly |
| Dubinsky et al[25] | 1 yr | Male | Yes | NR | NR | A/C | Surgery | Obstruction | Crohn's disease |
| Navarro et al[26] | 13 yr | Male | No | No | NR | T/C | BE→Surgery | Obstruction | None |
| Ahrar et al[27] | 29 yr | Male | No | No | NR | A/C | BE→Surgery | NR | None |
| Our case | 20 yr | Male | Yes | No | No | A/C | Surgery | Obstruction | MPGN |
In conclusion, although primary PI often represents a benign condition that should not be considered as an argument for surgery, emergent laparotomy should be considered for cases with intussusception, obstruction, and unsuccessful resolution of intussusception by colonoscopy or barium enema.
A 20-year-old man presented our hospital with a 3-d history of intermittent lower abdominal pain.
The authors performed an urgent laparotomy under the diagnosis of acute abdomen with obstructing intussusception.
A right hemicolectomy was performed because other polyposis diseases or intussusception relapse could not be ruled out.
All serum levels tested were within the normal range, with the exception of serum total bilirubin (1.5 mg/dL; normal range, 0.3-1.2 mg/dL). White blood cells (WBCs) (21000/μL), hemoglobin concentration (17.1 g/dL), and the C-reactive protein concentration (0.5 mg/dL) were also elevated.
Computed tomography revealed intussusception of the ascending colon with air within the wall.
A gross examination showed that the mucosa of the resected colon appeared normal with no evidence of ulceration or ulcer-related lesions, but instead a number of soft, yellowish cystic masses, suggesting that to be pneumatosis cystoides intestinalis.
A right hemicolectomy was performed because other polyposis diseases or intussusception relapse could not be ruled out, and to help make a final pathological diagnosis.
To our knowledge, 9 reported cases, including the present case, had intussusception associated with primary pneumatosis cystoides intestinalis.
Although primary pneumatosis intestinalis (PI) often represents a benign condition that should not be considered as an argument for surgery, emergent laparotomy should be considered for cases with intussusception, obstruction, and unsuccessful resolution of intussusception by colonoscopy or barium enema.
This is an interesting article summarising a case of PI and intususception with a review of the cases in the literature.
P- Reviewer: Lee HC, Sodergren MH S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kurbegov AC, Sondheimer JM. Pneumatosis intestinalis in non-neonatal pediatric patients. Pediatrics. 2001;108:402-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Nathan H, Singhal S, Cameron JL. Benign pneumatosis intestinalis in the setting of celiac disease. J Gastrointest Surg. 2006;10:890-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Donovan S, Cernigliaro J, Dawson N. Pneumatosis intestinalis: a case report and approach to management. Case Rep Med. 2011;2011:571387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Devillé WL, Buntinx F, Bouter LM, Montori VM, de Vet HC, van der Windt DA, Bezemer PD. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2002;2:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 701] [Cited by in RCA: 756] [Article Influence: 32.9] [Reference Citation Analysis (1)] |
| 5. | KOSS LG. Abdominal gas cysts (pneumatosis cystoides intestinorum hominis); an analysis with a report of a case and a critical review of the literature. AMA Arch Pathol. 1952;53:523-549. [PubMed] |
| 6. | Knechtle SJ, Davidoff AM, Rice RP. Pneumatosis intestinalis. Surgical management and clinical outcome. Ann Surg. 1990;212:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 151] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 7. | Gelman SF, Brandt LJ. Pneumatosis intestinalis and AIDS: a case report and review of the literature. Am J Gastroenterol. 1998;93:646-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 8. | Zülke C, Ulbrich S, Graeb C, Hahn J, Strotzer M, Holler E, Jauch KW. Acute pneumatosis cystoides intestinalis following allogeneic transplantation -- the surgeon’s dilemma. Bone Marrow Transplant. 2002;29:795-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Vijayakanthan N, Dhamanaskar K, Stewart L, Connolly J, Leber B, Walker I, Trus M. A review of pneumatosis intestinalis in the setting of systemic cancer treatments, including tyrosine kinase inhibitors. Can Assoc Radiol J. 2012;63:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Petrides C, Kyriakos N, Andreas I, Konstantinos P, Chrysanthos G, Athanasios P, Pikoulis E. Pneumatosis cystoides intestinalis after cetuximab chemotherapy for squamous cell carcinoma of parotid gland. Case Rep Surg. 2015;2015:530680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 11. | Honne K, Maruyama A, Onishi S, Nagashima T, Minota S. Simultaneous pneumatosis cystoides intestinalis and pneumomediastinum in a patient with systemic sclerosis. J Rheumatol. 2010;37:2194-2195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Robertson MB, Choe KA, Joseph PM. Review of the abdominal manifestations of cystic fibrosis in the adult patient. Radiographics. 2006;26:679-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Marinello DK, Rafael D, Paiva Edos S, Dominoni RL. Systemic lupus erythematosus complicated by intestinal vasculitis and pneumatosis intestinalis. Rev Bras Reumatol. 2010;50:596-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Woo K, Major K, Kohanzadeh S, Allins AD. Laparotomy for visceral ischemia and gangrene. Am Surg. 2007;73:1006-1008. [PubMed] |
| 15. | Kreiss C, Forohar F, Smithline AE, Brandt LJ. Pneumatosis intestinalis complicating C. difficile pseudomembranous colitis. Am J Gastroenterol. 1999;94:2560-2561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 16. | Kelly BS, Meyers P, Choe KA, Hurst J, Luchette FA. Traumatic pneumatosis cystoides intestinalis with portal venous air embolism. J Trauma. 1997;42:112-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Boerner RM, Fried DB, Warshauer DM, Isaacs K. Pneumatosis intestinalis. Two case reports and a retrospective review of the literature from 1985 to 1995. Dig Dis Sci. 1996;41:2272-2285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 75] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Tahiri M, Levy J, Alzaid S, Anderson D. An approach to pneumatosis intestinalis: Factors affecting your management. Int J Surg Case Rep. 2015;6C:133-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | DuBose JJ, Lissauer M, Maung AA, Piper GL, O’Callaghan TA, Luo-Owen X, Inaba K, Okoye O, Shestopalov A, Fielder WD. Pneumatosis Intestinalis Predictive Evaluation Study (PIPES): a multicenter epidemiologic study of the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2013;75:15-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Nagata S, Ueda N, Yoshida Y, Matsuda H. Pneumatosis coli complicated with intussusception in an adult: report of a case. Surg Today. 2010;40:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Emanuel P, Pertsemlidis DS, Gordon R, Xu R. Benign hybrid perineurioma-schwannoma in the colon. A case report. Ann Diagn Pathol. 2006;10:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Sugita M, Mori T, Shimada H, Shimasaki N, Morikawa Y, Takahashi T. Colocolic intussusception associated with pneumatosis cystoides intestinalis after cord blood stem cell transplantation. J Pediatr Gastroenterol Nutr. 2004;38:549-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Stern MA, Chey WD. Images in clinical medicine. Pneumatosis coli and colonic intussusception. N Engl J Med. 2001;345:964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Morrison SC, Laya B. Colo-colic intussusception in an infant with pneumatosis. Pediatr Radiol. 2001;31:494-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Dubinsky MC, Deslandres C, Patriquin H, Seidman EG. Pneumatosis intestinalis and colocolic intussusception complicating Crohn’s disease. J Pediatr Gastroenterol Nutr. 2000;30:96-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 26. | Navarro O, Daneman A, Alton DJ, Thorner P. Colo-colic intussusception associated with pneumatosis cystoides intestinalis. Pediatr Radiol. 1998;28:515-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Ahrar K, Watkins GE, Gardiner G. Colocolic intussusception caused by pneumatosis cystoides coli. Abdom Imaging. 1997;22:392-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |