Published online Apr 27, 2024. doi: 10.4240/wjgs.v16.i4.1165
Peer-review started: December 22, 2023
First decision: January 9, 2024
Revised: January 18, 2024
Accepted: March 28, 2024
Article in press: March 28, 2024
Published online: April 27, 2024
Crohn's disease (CD) is a chronic inflammatory disease of the gastrointestinal tract, often requiring intestinal resection as a common treatment. However, re
To measure the influence of anastomosis techniques on the long-term relapse rate of CD by conducting a meta-analysis.
PubMed, Scopus, and Cochrane Library were searched until October 8, 2023. Patients who underwent intestinal resection due to CD were included. The in
From 2011 to 2023, six articles met the inclusion and exclusion criteria. The results indicated that Kono-S ana
Kono-S anastomosis has the potential to expedite the recuperation of CD and diminish relapse hazards; however, additional larger trials are necessary to authenticate its effectiveness.
Core Tip: There is no agreement in academic studies regarding the impact of Kono-S and traditional anastomosis on patients' recurrence after Crohn's surgery. Here, we present a primary inclusive meta-analysis exploring the effect of Kono-S and traditional anastomosis on the recurrence of Crohn's disease following surgery. The hospital stay post-surgery, the incidence of postoperative complications, the proportion of Clavien-Dindo ≥ IIIa, the postoperative recurrence rate, and the Rutgeerts score were examined in patients who underwent the two techniques.
- Citation: Wang ZZ, Zhao CH, Shen H, Dai GP. Impact of different anastomosis methods on post-recurrence after intestinal resection for Crohn's disease: A meta-analysis. World J Gastrointest Surg 2024; 16(4): 1165-1175
- URL: https://www.wjgnet.com/1948-9366/full/v16/i4/1165.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i4.1165
Crohn's disease (CD) is a chronic granulomatous enteritis that can affect any part of the digestive tract, with a particular predilection to the terminal ileum and cecum[1]. The disease is characterized by clinical features, such as abdominal pain, diarrhea, weight loss, and recurrent episodes, which could result in severe malnutrition in patients[2]. In Europe, the annual incidence rate of CD stands at 12.7 cases/100000 individuals, while in North America, it is nearly 20.2 cases/100000 individuals. Furthermore, the incidence rate has demonstrated a consistent upward trend in recent years[3]. Recent research has indicated that CD pathogenesis is linked to several factors, such as genetic susceptibility, imbalanced intestinal microbial communities, environmental factors, abnormal immune regulation, and excessive expression of in
Intestinal anastomosis is an essential determinant of CD recurrence after surgery[11]. The traditional techniques of anastomosis, including end-to-end anastomosis (EEA), end-to-side anastomosis (ESA), and side-to-side anastomosis (SSA), are widely used due to their ease of operation and high repeatability[12]. Recently, there have been several reports on a new anastomosis technique, known as Kono-S anastomosis, which aims to decrease the likelihood of postoperative recurrence in patients. This anastomosis technique excludes the mesentery from the anastomosis, limits lumen defor
To gather additional experimental evidence, we conducted independent searches on PubMed, EMBASE, and Cochrane Library databases. Our selection criteria included articles with human participants, reported in English. We imposed no restrictions on publication time and type of articles. For the intervention group, we used Kono-S anastomosis whereas traditional anastomosis was used as the control group, following the PICOS scheme. The participants consisted of pa
The following combination was used for the EMBASE database: (1) "crohn disease"/ exp OR "crohn disease"; (2) postoperative; (3) intestinal resection; (4) Kono-S anastomosis; (5) Kono-S Anastomosis; (6) anastomosis; (7) 4 OR 5; (8) 2 OR 3; and (9) 1 AND 7 AND 8.
The same keywords were inserted into the Cochrane Library, which used the following search strategy: (1) MeSH descriptor: (Crohn Disease) explode all trees; (2) (Kono-S anastomosis): ti, ab, kw; (3) (Kono-S Anastomosis): ti, ab, kw; (4) (Anastomosis): ti, ab, kw; (5) 2 OR 3 OR 4; (6) (postoperative): ti, ab, kw; (7) (intestinal resection): ti, ab, kw; (8) 6 OR 7; and (9) 1 AND 5 AND 8.
In the field of management, the search scope is expanded through extensive cross-checking of the reference lists of all articles that meet the inclusion criteria. The search deadline for all databases was October 8, 2023. This study was conducted based on the PRISMA 2020 statement guidelines, with complete reporting of the meta-analysis data[16].
The primary studies' titles and abstracts were screened independently by the same two authors. Employing Cohen’s kappa statistic, the authors evaluated their agreement during the initial article screening. Non-conforming and duplicate articles were excluded after reviewing the topic, abstract, and keywords. The meta-analysis applied the following criteria: a clear, comprehensive, and objective style, simple language, consistent citation, standard structure, formal register, meticulous and precise vocabulary, and grammatical accuracy.
The inclusion criteria consisted of the following: (1) Studies evaluating patients who had undergone intestinal resection due to CD; (2) studies in which the intervention measure used was Kono-S anastomosis, while the control group received traditional anastomosis (including EEA, ESA, and SSA); (3) studies where relevant data for extraction were available in the results report; (4) randomized clinical trials (RCTs) and observational studies; and (5) studies evaluating the influence of Kono-S anastomosis on the occurrence of CD recurrence after intestinal resection. Review articles, letters, comments, case reports, as well as studies that did not evaluate postoperative recurrence indicators, were excluded from this ana
We examined all pertinent literature, tables, and charts and extracted relevant data as shown in Tables 1 and 2. The primary contents encompassed the following: (1) The name of the primary author, their country, publication date, and research type; (2) fundamental clinical data for patients with CD in the Kono-S anastomosis group and the traditional anastomosis group; and (3) postoperative observation measures, such as the hospital stay post-surgery, total incidence of postoperative complications, Clavien-Dindo scores ≥ IIIa (%), total recurrence rate, and Rutgeerts score[17]. If further information was required, we reached out to the corresponding author of the paper for assistance via email. Furthermore, any discrepancies among the reviewers were resolved through sound and sensible discussion.
| Ref. | Country | Type of study | Total number of patients | Kono-S anastomosis | Traditional anastomosis | ||||
| No. of patients | Age | M/F | No. of patients | Age | M/F | ||||
| Shimada et al[15], 2019 | Japan | Retro/cohort study | 215 | 117 | 39.00 ± 3.13 | 84/33 | 98 | 35.06 ± 11.29 | 74/24 |
| Tyrode et al[19], 2023 | France | Retro/cohort study | 85 | 30 | 36.11 ± 14.01 | 13/17 | 55 | 33.83 ± 12.79 | 24/31 |
| Kelm et al[20], 2022 | Germany | Retro/cohort study | 51 | 22 | 38.41 ± 11.00 | 14/8 | 29 | 38.42 ± 13.57 | 14/15 |
| Alibert et al[21], 2023 | France | Retro/cohort study | 432 | 155 | 38.20 ± 13.90 | 79/76 | 277 | 37.60 ± 14.20 | 107/170 |
| Kono et al[22], 2011 | Japan | Retro/cohort study | 142 | 69 | 32.36 ± 9.09 | 57/12 | 73 | 29.38 ± 10.06 | 58/15 |
| Luglio et al[23], 2020 | Italy | RCT | 79 | 36 | 34.75 ± 5.91 | 18/18 | 43 | 43.10 ± 7.55 | 22/21 |
| Ref. | Hospital stay (d) | Postoperative morbidity (%) | Recurrence rate (%) | Mean Rutgeerts score | Clavien-Dindo ≥ IIIa (%) |
| Shimada et al[15] | |||||
| Kono-S anastomosis | NR | 64/117(54.70) | 4/117 (3.4) | NR | NR |
| Traditional anastomosis | NR | 68/98(69.39) | 24/98 (24.5) | NR | NR |
| Tyrode et al[19] | |||||
| Kono-S anastomosis | 6.71 ± 1.56 | 2/30(6.66) | 17/30 (56.66) | NR | 5/30 (16.67) |
| Traditional anastomosis | 7.00 ± 1.52 | 6/55(10.90) | 27/55 (49.10) | NR | 9/55 (16.36) |
| Kelm et al[20] | |||||
| Kono-S anastomosis | 8.1 ± 2.34 | 15/22(68.19) | 7/22 (31.82) | 1.70 ± 0.32 | 3/22 (13.64) |
| Traditional anastomosis | 8.1 ± 2.56 | 9/29(31.03) | 13/29 (44.83) | 2.50 ± 0.86 | 4/29 (13.79) |
| Alibert et al[21] | |||||
| Kono-S anastomosis | 6.20 ± 4.00 | 70/155(45.16) | NR | NR | 7/155 (4.52) |
| Traditional anastomosis | 7.80 ± 5.60 | 79/277(28.52) | NR | NR | 21/277 (7.58) |
| Kono et al[22] | |||||
| Kono-S anastomosis | NR | 3/69(4.34) | 49/69 (71.01) | 2.58 ± 0.63 | NR |
| Traditional anastomosis | NR | 7/73(9.59) | 58/73 (79.45) | 3.34 ± 0.42 | NR |
| Luglio et al[23] | |||||
| Kono-S anastomosis | 7.00 ± 3.00 | 16.67 | 8/36 (22.22) | 1.05 ± 1.06 | NR |
| Traditional anastomosis | 7.60 ± 3.08 | 25.58 | 27/43 (62.79) | 2.30 ± 1.32 | NR |
The Cochrane Risk Bias Assessment Tool was implemented to gauge bias risks in RCTs. The potential for bias was evaluated by examining factors, such as random sequence generation, allocation concealment, blinding, completeness of outcome data, selective reporting, and other possible sources of bias. Based on three aspects: Selectivity, comparability, and outcome, the Newcastle-Ottawa Scale (NOS) score was employed to assess the quality of cohort studies. The funnel plot was utilized to assess the prospect of publication bias by analyzing the scatter points' distribution.
RevMan 5.3 was utilized to perform a meta-analysis. The OR and the average difference between groups (MD) were employed as summary measures of dichotomous and continuous variables, respectively. The 95%CI was applied to both methods. In cases where studies provided median and quartile ranges, the average SD was calculated[18]. Heterogeneity was evaluated using the I2 test. If I2 < 50% and P > 0.1, we ascertained that heterogeneity among the studies was low; thus, a fixed-effects model was applied. However, if P < 0.1 and I2 > 50%, we determined that heterogeneity among the studies was high, and a random-effects model was employed for analyzing the sources of heterogeneity. To assess publication bias, we generated funnel plots. We conducted sensitivity analyses using the one-by-one exclusion method. If there was a significant change in the I2 value after removing an item, the study results were regarded as the origin of heterogeneity. All statistical analysis was significant at the P < 0.05 level.
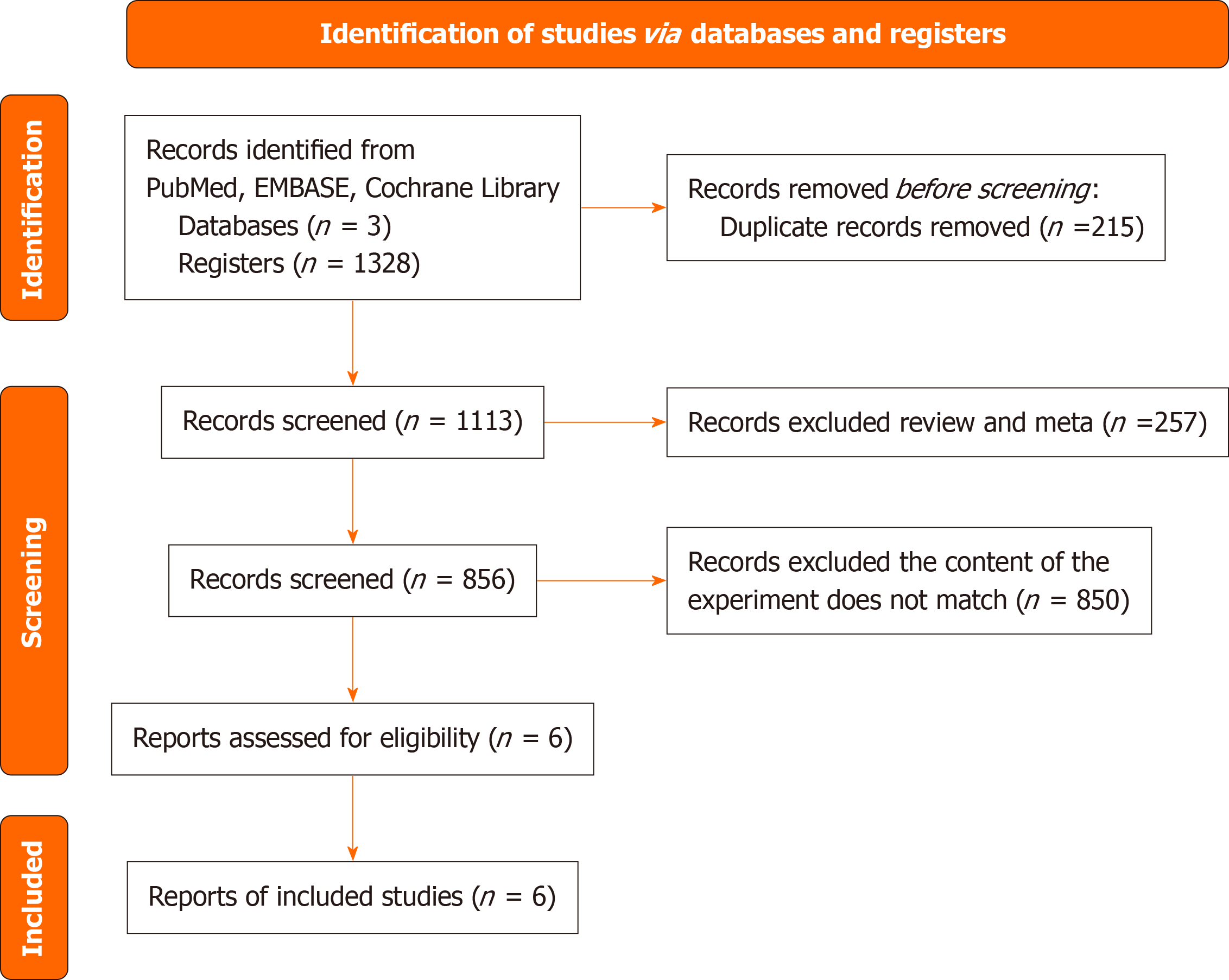
A total of 1328 articles were collected. Among them, 215 were repetitive and therefore removed. We then analyzed the titles and abstracts of the remaining 1113 articles. Among these, 76 articles were meta-analyses, 181 were review articles, and 850 did not involve the experimental comparison of Kono-S and traditional anastomosis. Finally, we chose six articles[15,19-23] for a full-text review, from which, we extracted all of the necessary literature data. A meta-analysis of six articles was conducted, all published between 2011 and 2023. The studies consisted of 1 randomized controlled trial and 5 retrospective cohort studies (Figure 1), collectively involving 1004 patients with CD. Among these patients, 429 under
The evaluation of RCT literature quality was conducted based on several criteria, such as random number generation, allocation blindness, researcher and subject blindness, result evaluation blindness, result integrity, reporting bias, and other factors. Based on the Cochrane risk bias assessment tool, the included randomized controlled study[23] exhibited a low risk in random sequence generation; nevertheless, the blind allocation component was unclear. Minimal risk was observed in incomplete results data, as well as in selective results reporting. Furthermore, other potential bias factors meeting the requirements of this article were assessed as low risk. The literature's quality was evaluated concerning selection bias, comparability bias, and result evaluation bias according to the NOS scale. A research quality score of 9 was achieved by one paper[15], while three papers[19,20,22] received a research quality score of 8. Additionally, one paper[21] secured a research quality score of 7. Table 3 summarizes the quality evaluation of all retrospective cohort studies. There was no disagreement between the two authors regarding the eligibility of the full-text articles (Cohen's kappa = 1).
| Ref. | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at the start of the study | Comparability of cohorts based on the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts | Total scores |
| Shimada et al[15] | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Tyrode et al[19] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| Kelm et al[20] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 8 |
| Alibert et al[21] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| Kono et al[22] | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
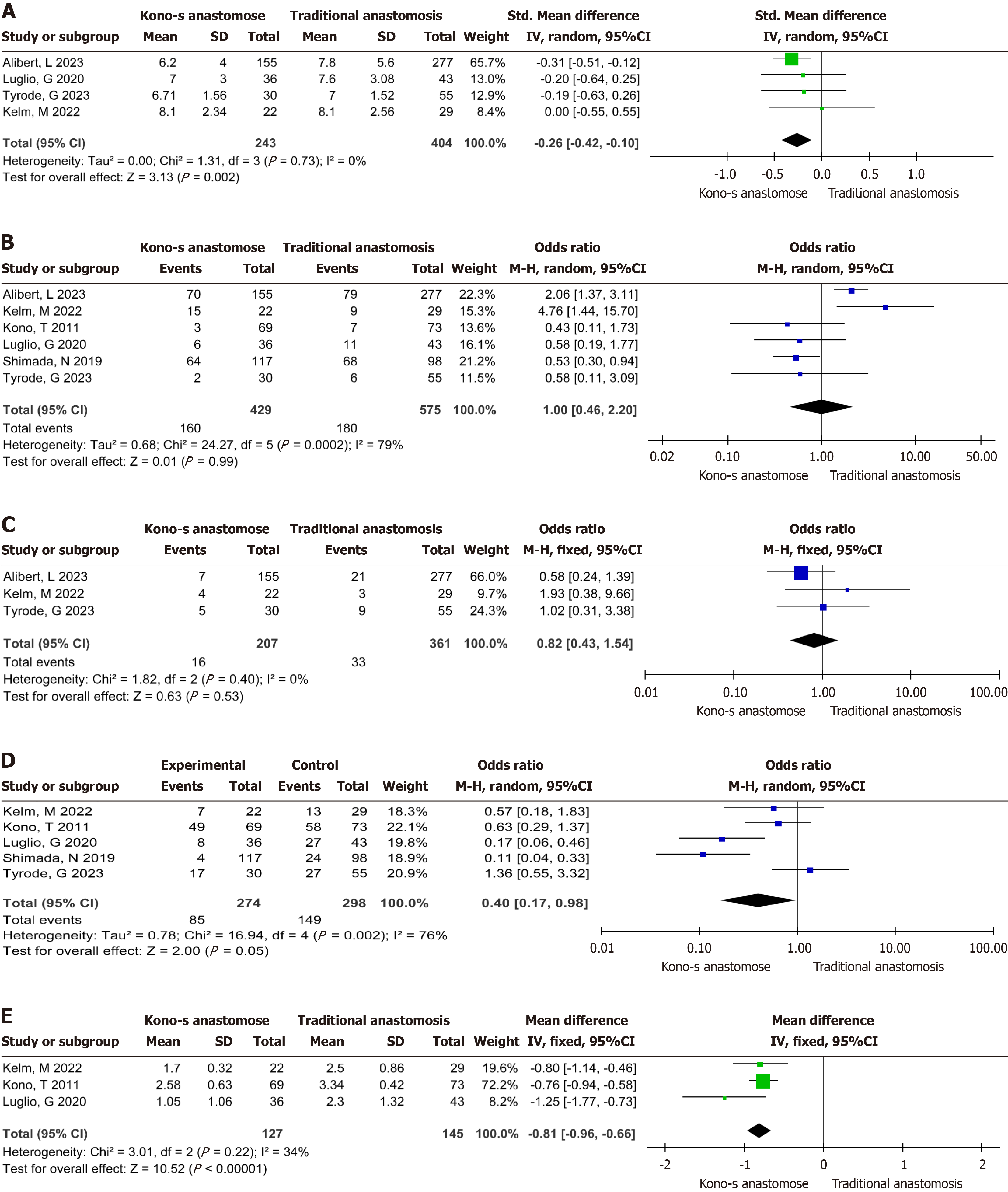
The impact of alternative anastomosis methods (Kono-S and traditional) on the hospital stay following intestinal resection for CD was evaluated using a meta-analysis. The fixed effect model indicated moderate heterogeneity among the in
The impact of various anastomosis methods (Kono-S and traditional), post intestinal resection, on the overall incidence of postoperative complications in CD was evaluated through a meta-analysis. The analysis revealed a high degree of heterogeneity among the included literature in the fixed effect model (I2 = 79%, P = 0.02). Notably, even after using the random effect model, the included literature remained significantly heterogeneous (I2 = 79%, P = 0.02). After conducting sen
No heterogeneity was observed among the included studies, with I2 = 0% and P = 0.40 under the fixed effect model. The study findings indicate that the Kono-S anastomosis method did not significantly affect the proportion of Clavien-Dindo ≥ IIIa in patients with CD, compared with other conventional anastomosis techniques [MD = 0.82, 95%CI: 0.43 to 1.54, P = 0.53, Figure 2C].
The impact of Kono-S and traditional anastomosis methods on the overall recurrence rate of CD following intestinal resection was analyzed through a meta-analysis. The fixed effect model revealed a high level of heterogeneity amongst the included studies, with I2 = 76% and P = 0.002. Subsequently, the random effect model also indicated a high level of heterogeneity among the included literature. Sensitivity analysis revealed that the studies conducted by Shimada et al[15] and Luglio et al[23] had the most significant influence on the results, possibly originating as the primary source of heterogeneity. The study results demonstrate that Kono-S anastomosis yields a statistically significant reduction in the total recurrence rate of patients with CD compared with other traditional anastomosis methods [MD = 0.40, 95%CI: 0.17 to 0.98, P = 0.05, Figure 2D].
A meta-analysis indicated low heterogeneity (I2 = 34%, P = 0.22) using the fixed-effect model. The study results indicate that Kono-S anastomosis is a more effective method in reducing postoperative Rutgeerts scores for patients with CD compared to other conventional anastomosis techniques. This difference was statistically significant [MD = -0.81, 95%CI: -0.96 to -0.66, P < 0.001, Figure 2E].
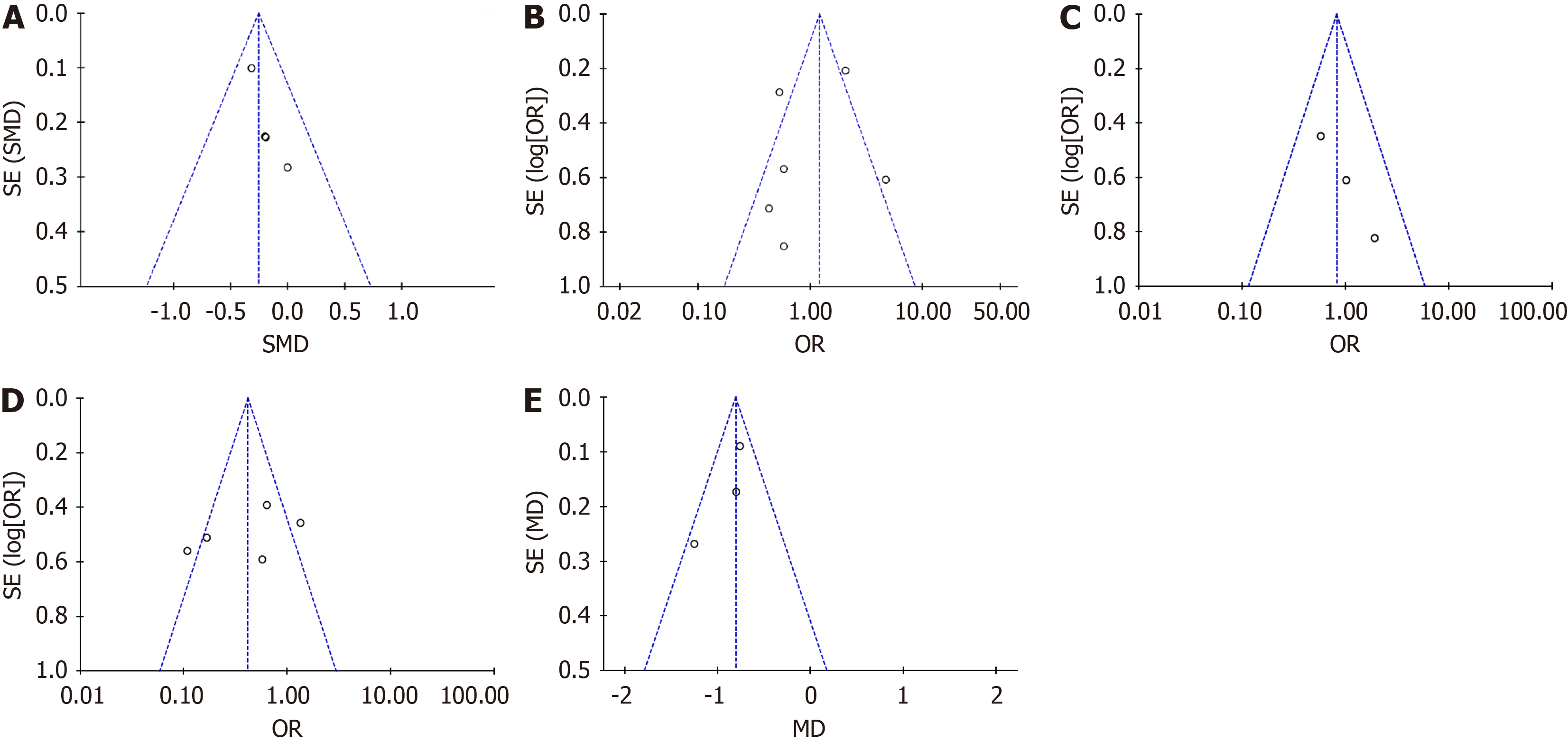
A funnel plot was created for each impact indicator identified within the six included articles. Continuous variables for the length of hospital stay post-surgery and Rutgeerts score were analyzed, along with binary variables for the total incidence of postoperative complications, proportion of Clavien-Dindo ≥ IIIa, and total postoperative recurrence rate. Technical abbreviations were explained upon first use. The funnel plot meta-analysis demonstrated that hospital stay post-surgery, proportion of Clavien-Dindo ≥ IIIa, and Rutgeerts score were all aligned using a vertical line. The research was evenly dispersed on both sides of the center line, creating a pyramidal dotted line range, with no evident separation phenomenon (Figure 3; no conspicuous bias). However, the meta-analysis funnel plot of the remaining impact indicators exhibited bias, possibly due to inadequate literature included in this study.
Since its introduction by Kono et al[22] in 2003, the efficacy of the EEA technique for anti-mesenteric function has been a subject of debate. The Kono-S anastomosis procedure involves employing a linear cutter to section the intestine, after which the intestinal ends are sutured together to form a support column. Subsequently, a functional end-to-end manual suture is performed[24,25]. Kono et al[22] posited that anastomosis effectively prevents postoperative recurrence in patients with CD. Historical data comparison revealed that the endoscopic recurrence rate of patients who underwent Kono-S anastomosis was lower than those who underwent traditional anastomosis. However, the persuasiveness of a single study is limited. Therefore, this study used meta-analysis to compare and analyze the impact of Kono-S anastomo
The meta-analysis results of this study showed that Kono-S anastomosis could shorten the hospital stay of patients with CD, compared with other traditional anastomosis methods [MD = -0.26, 95%CI: -0.42 to -0.10, P = 0.002]. Notably, no heterogeneity was observed in the included literature. Many studies evaluating recurrence factors tend to overlook the postoperative hospitalization time, which can indicate the patient's recovery rate. Regarding surgical operations, Kono-S anastomosis preserves a portion of the mesenteric blood perfusion, potentially resulting in a reduction of ischemic injury at the anastomosis[11,22]. Adequate blood supply creates favorable biological circumstances for anastomotic healing, consequently lowering the risk of early complications like anastomotic leakage and stenosis[26]. This in turn avoids additional surgery and extended hospital stays caused by complications. Furthermore, Kono-S anastomosis optimizes the anatomical position and three-dimensional structure of the intestinal segment, promoting swift recovery of postoperative intestinal peristalsis function, early elimination, and bowel movements in patients, and faster rehabilitation. These factors may explain why Kono-S anastomosis is advantageous for hastening the postoperative recovery of patients with CD.
Regarding postoperative complications in these patients, the number of incidences, such as intestinal obstruction, anastomotic leakage, infection, and fever were tallied for the purposes of comparing the safety of the two anastomosis methods. The outcomes indicated that the Kono-S anastomosis had no considerable impact on the overall occurrence of postoperative complications in patients with CD when compared to the traditional anastomosis method [MD = 1.00, 95%CI: 0.46 to 2.20, P = 0.99]. However, this meta-analysis has a relatively small sample size, as only 6 studies, comprising a total of 1004 patients, were included. There is some degree of uncertainty, making it necessary to interpret the results with caution. Additionally, the incidence of complications is correlated with various factors, including the surgical procedure, perioperative treatment, and the patient's underlying health condition[27]. Therefore, due to these confound
Regarding the postoperative recurrence rate of patients with CD, the study findings demonstrate that the Kono-S anastomosis method resulted in lower total recurrence rates compared to other traditional methods [MD = 0.40, 95%CI: 0.17 to 0.98, P = 0.05]. Endoscopic anastomotic recurrence is typically evaluated through the Rutgeerts score (≥ IIIa) at 6 to 12 months. Therefore, we performed a meta-analysis of Rutgeerts score. Our findings indicate that Kono-S anastomosis can significantly reduce Rutgeerts score in patients with CD following surgery when compared to traditional anastomosis [MD = -0.81, 95%CI: -0.96 to -0.66, P < 0.001]. These findings align with those of a meta-analysis published in 2020, which showed that Kono-S anastomosis presents a reduced risk of recurrence in comparison to traditional anastomosis[30]. Although the sample size for this study is limited, the outcomes are clinically significant as postoperative recurrence directly impacts patients' life quality and prognosis. On the contrary, Kono-S anastomosis could enhance healing con
The limitations of this study stem from its small sample size and sole location of data collection at a single center. We anticipate the need for more studies of high quality to verify this outcome and establish the precise mechanism by which Kono-S anastomosis diminishes recurrence. It is important to recognize that the effectiveness of this surgical approach is contingent upon rigorous regulation of operative procedures and the selection of suitable candidates. Future research must develop a uniform training program for Kono-S anastomosis and delineate the patient cohorts who can gain the maximum benefit from this technique.
To summarize, this study showed that Kono-S anastomosis is a suitable technique for patients with CD. It has proven to speed up postoperative recovery and is particularly effective in reducing long-term recurrence when compared to other conventional anastomosis methods. While this study has limitations, including a limited number of included studies and sample size, the results still provide robust support for the clinical application of Kono-S anastomosis. It is recommended that clinicians select the appropriate anastomotic technique based on the specific conditions of patients, and we anticipate further validation of the long-term efficacy of Kono-S through larger sample studies in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hawkins J, United States; Triggi M, Greece S-Editor: Lin C L-Editor: A P-Editor: Xu ZH
| 1. | Freeman HJ. Natural history and long-term clinical course of Crohn's disease. World J Gastroenterol. 2014;20:31-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 101] [Cited by in F6Publishing: 99] [Article Influence: 9.9] [Reference Citation Analysis (4)] |
| 2. | Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet. 2017;389:1741-1755. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1121] [Cited by in F6Publishing: 1373] [Article Influence: 196.1] [Reference Citation Analysis (3)] |
| 3. | Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769-2778. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2677] [Cited by in F6Publishing: 3178] [Article Influence: 454.0] [Reference Citation Analysis (0)] |
| 4. | Khanna S, Raffals LE. The Microbiome in Crohn's Disease: Role in Pathogenesis and Role of Microbiome Replacement Therapies. Gastroenterol Clin North Am. 2017;46:481-492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Petagna L, Antonelli A, Ganini C, Bellato V, Campanelli M, Divizia A, Efrati C, Franceschilli M, Guida AM, Ingallinella S, Montagnese F, Sensi B, Siragusa L, Sica GS. Pathophysiology of Crohn's disease inflammation and recurrence. Biol Direct. 2020;15:23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 6. | Ballester Ferré MP, Boscá-Watts MM, Mínguez Pérez M. Crohn's disease. Med Clin (Barc). 2018;151:26-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Seyedian SS, Nokhostin F, Malamir MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life. 2019;12:113-122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 210] [Cited by in F6Publishing: 232] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 8. | Rodríguez-Lago I, Gisbert JP. The Role of Immunomodulators and Biologics in the Medical Management of Stricturing Crohn's Disease. J Crohns Colitis. 2020;14:557-566. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Barnes EL. Postoperative Crohn's disease management. Curr Opin Gastroenterol. 2020;36:277-283. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Cottone M, Mocciaro F, Orlando A. Infliximab prevents Crohn's disease recurrence after ileal resection. Expert Rev Gastroenterol Hepatol. 2009;3:231-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Meima-van Praag EM, Buskens CJ, Hompes R, Bemelman WA. Surgical management of Crohn's disease: a state of the art review. Int J Colorectal Dis. 2021;36:1133-1145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Bislenghi G, Devriendt S, Wolthuis A, D'Hoore A. Totally stapled Kono-S anastomosis for Crohn's disease. Tech Coloproctol. 2022;26:213-216. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 13. | Dasharathy SS, Limketkai BN, Sauk JS. What's New in the Postoperative Management of Crohn's Disease? Dig Dis Sci. 2022;67:3508-3517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Horisberger K, Birrer DL, Rickenbacher A, Turina M. Experiences with the Kono-S anastomosis in Crohn's disease of the terminal ileum-a cohort study. Langenbecks Arch Surg. 2021;406:1173-1180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Shimada N, Ohge H, Kono T, Sugitani A, Yano R, Watadani Y, Uemura K, Murakami Y, Sueda T. Surgical Recurrence at Anastomotic Site After Bowel Resection in Crohn's Disease: Comparison of Kono-S and End-to-end Anastomosis. J Gastrointest Surg. 2019;23:312-319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17946] [Cited by in F6Publishing: 21945] [Article Influence: 7315.0] [Reference Citation Analysis (0)] |
| 17. | Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn's disease. Gastroenterology. 1990;99:956-963. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1226] [Cited by in F6Publishing: 1114] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 18. | Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785-1805. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 836] [Cited by in F6Publishing: 1527] [Article Influence: 190.9] [Reference Citation Analysis (0)] |
| 19. | Tyrode G, Lakkis Z, Vernerey D, Falcoz A, Clairet V, Alibert L, Koch S, Vuitton L. KONO-S Anastomosis Is Not Superior to Conventional Anastomosis for the Reduction of Postoperative Endoscopic Recurrence in Crohn's Disease. Inflamm Bowel Dis. 2023;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 20. | Kelm M, Reibetanz J, Kim M, Schoettker K, Brand M, Meining A, Germer CT, Flemming S. Kono-S Anastomosis in Crohn's Disease: A Retrospective Study on Postoperative Morbidity and Disease Recurrence in Comparison to the Conventional Side-To-Side Anastomosis. J Clin Med. 2022;11. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 21. | Alibert L, Betton L, Falcoz A, Manceau G, Benoist S, Zerbib P, Podevin J, Maggiori L, Brouquet A, Tyrode G, Vuitton L, Vernerey D, Lefevre JH, Lakkis Z. Does KONO-S anastomosis reduce recurrence in Crohn's disease compared to conventional ileocolonic anastomosis? A nationwide propensity score-matched study from GETAID Chirurgie Group (KoCoRICCO study). J Crohns Colitis. 2023;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Kono T, Ashida T, Ebisawa Y, Chisato N, Okamoto K, Katsuno H, Maeda K, Fujiya M, Kohgo Y, Furukawa H. A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn's disease. Dis Colon Rectum. 2011;54:586-592. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 23. | Luglio G, Rispo A, Imperatore N, Giglio MC, Amendola A, Tropeano FP, Peltrini R, Castiglione F, De Palma GD, Bucci L. Surgical Prevention of Anastomotic Recurrence by Excluding Mesentery in Crohn's Disease: The SuPREMe-CD Study - A Randomized Clinical Trial. Ann Surg. 2020;272:210-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 84] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 24. | Alshantti A, Hind D, Hancock L, Brown SR. The role of Kono-S anastomosis and mesenteric resection in reducing recurrence after surgery for Crohn's disease: a systematic review. Colorectal Dis. 2021;23:7-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 25. | Fichera A, Zoccali M, Kono T. Antimesenteric functional end-to-end handsewn (Kono-S) anastomosis. J Gastrointest Surg. 2012;16:1412-1416. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Fornaro R, Caristo G, Stratta E, Oliva A, Giovinazzo D, Mascherini M, Frascio M. Crohn's disease and postoperative recurrence. The role of anastomotic configurations and the kono-s anastomosis. Ann Ital Chir. 2019;90:111-120. [PubMed] [Cited in This Article: ] |
| 27. | Kann BR. Anastomotic Considerations in Crohn's Disease. Clin Colon Rectal Surg. 2023;36:63-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 28. | Saeed M, Algahiny AT, Elmitwalli OSMMS, Ahmed MMMRM, Juma IM. An Analysis of the Literature and a Case Study on the Successful Surgical Treatment of a Crohn's Patient Using a Kono-S Anastomosis. Euroasian J Hepatogastroenterol. 2023;13:36-39. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 29. | Katsuno H, Maeda K, Hanai T, Masumori K, Koide Y, Kono T. Novel antimesenteric functional end-to-end handsewn (Kono-S) anastomoses for Crohn's disease: a report of surgical procedure and short-term outcomes. Dig Surg. 2015;32:39-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 30. | Ng CH, Chin YH, Lin SY, Koh JWH, Lieske B, Koh FH, Chong CS, Foo FJ. Kono-S anastomosis for Crohn's disease: a systemic review, meta-analysis, and meta-regression. Surg Today. 2021;51:493-501. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | Ibrahim R, Abounozha S, Kheder A, Alawad A. Does anastomotic technique affects the recurrence rate of Crohn's disease after ileocolic resection? Ann Med Surg (Lond). 2021;62:164-167. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 32. | Clark DA, Smith N, Clark I, Giddings H, Rajan R. Time for an Australian and New Zealand randomized controlled trial to study the modified Kono S anastomosis. ANZ J Surg. 2022;92:3132-3134. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |