Published online Sep 15, 2023. doi: 10.4239/wjd.v14.i9.1412
Peer-review started: July 4, 2023
First decision: July 19, 2023
Revised: July 27, 2023
Accepted: August 7, 2023
Article in press: August 7, 2023
Published online: September 15, 2023
Early diabetic nephropathy (DN) is a complication of diabetes mellitus. It mainly affects kidney microvessels and glomerular function, and its timely and effective treatment is critical for early DN. However, the effects of treatments comprising simple Western medicine are not optimal. With the promotion and imple
To investigate the effect of sitagliptin tablets combined with Yiqi yangyin huoxue decoction on clinical efficacy and hemorheology in patients with early DN.
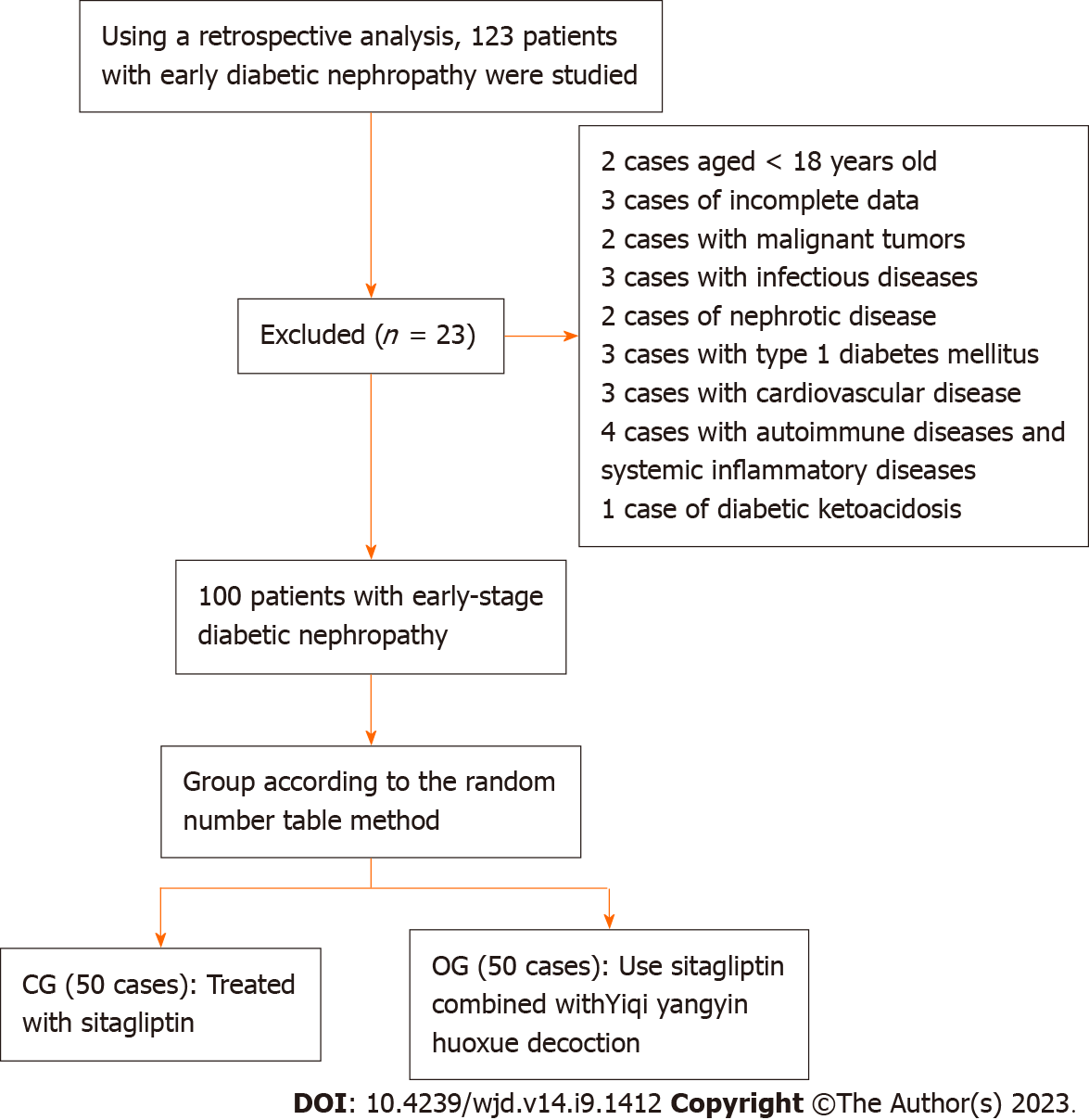
Through a retrospective analysis, 123 patients with early DN were admitted to the endocrinology clinic of the Changzhou NO. 7 People’s Hospital from January 2021 to October 2022 and were selected as study subjects. After rigorous screening, 100 patients with early DN were enrolled. The control group (CG, n = 50) and the observation group (OG, n = 50) were divided according to the treatment method. The CG were treated with sitagliptin, and the OG were treated with sitagliptin plus the Yiqi yangyin huoxue decoction. Both groups were treated for 3 mo. For both groups, the baseline data and clinical efficacy were compared, and changes in blood glucose levels, lipid levels, renal function, and hematological indicators before (T0) and after (T1) treatment were assessed.
The total effective rate for the OG was 94.00% and that of the CG was 80.00% (P < 0.05). After treatment (T1), the levels of fasting blood glucose, 2 h postprandial glucose, total cholesterol, triacylglycerol, and low-density lipoprotein cholesterol in OG patients were obviously lower than those in the CG (P < 0.05), and cystatin C, homocysteine, urinary microalbumin, and blood creatinine values in OG patients were also obviously lower than those in the CG (P < 0.05); erythrocyte deposition, plasma viscosity, whole blood high shear viscosity, and whole blood low shear viscosity were markedly lower in OG patients than in the CG (P < 0.05).
Sitagliptin combined with Yiqi yangyin huoxue decoction has a remarkable effect when used to treat patients with early DN. Further, it is helpful in improving hemorheological indices and controlling disease progression.
Core Tip: Early diabetic nephropathy (DN) mainly involves kidney microvessels and glomerular functions, and its timely and effective treatment is critical. In clinical practice, the overall treatment effect of medication alone is not ideal. The development of traditional Chinese medicine has demonstrated its superiority for the treatment of many diseases. In the present study, sitagliptin tablets combined with a blood decoction were used to treat patients with early DN. The results showed that sitagliptin combined with Yiqi yangyin huoxue decoction had a significant effect on the treatment of early DN, which was helpful in improving hemorheological indices.
- Citation: Ling J, Yang YH. Effect of sitagliptin combined with Yiqi yangyin huoxue decoction on clinical efficacy and hemorheology in early diabetic nephropathy. World J Diabetes 2023; 14(9): 1412-1421
- URL: https://www.wjgnet.com/1948-9358/full/v14/i9/1412.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i9.1412
Diabetes mellitus (DM) is a metabolic disease characterized by defective insulin secretion and activity. The prevalence of diabetes in China has been increasing, and that of DM in people over 18 years of age is as high as 11.2%[1]. Approximately 20%–40% of patients with diabetes in China have diabetic nephropathy (DN), and 21.8% of type 2 diabetes patients have this condition[2]. Early DN renal injury involves the glomeruli, renal tubules, renal interstitium, and renal blood vessels, with an increase in persistent urinary albumin excretion and a progressive decrease in the glomerular filtration rate, Early DN with glucose and lipid metabolism disorders, insulin resistance, hemodynamic changes, oxidative stress, inflammation, autophagy disorders, and other mechanisms[2-3]. Some patients with Type 2 DM (T2DM) have elevated urinary albumin levels upon diagnosis. If the microalbuminuria period is not treated promptly, it will rapidly progress to a lengthy albuminuria period until end-stage renal disease develops[4]. End-stage treatment of DN is more difficult than that of other renal diseases, with high disability rates. Accordingly, delaying the progression of DN is the focus of current research.
Presently, the key to clinical and early stage DN management is timely and effective treatment, such that disease development can be effectively controlled, which is beneficial for improving prognosis. Western medicine mainly involves lifestyle adjustments, a low-protein diet, lowering glucose and blood pressure, adjusting fat, reducing proteinuria, and improving renal function, as fundamental treatment principles[5]. Sitagliptin is a dipeptidyl peptidase-4 inhibitor that effectively improves fasting and postprandial blood glucose[6] in patients with T2DM[6]. Clinically, sitagliptin attenuates the oxidative stress response in kidney tissues, delays the progression of DN, and prevents the deterioration of renal function[7]. However, owing to the poor prognosis of DN, the overall treatment impact of individual medications is not ideal; therefore, other therapeutic drugs must be used in combination to improve the curative effect on early DN. With the development of traditional Chinese medicine (TCM), targeted protection of the potentially involved viscera, the predictable control of disease progress, and intervention-based treatment, significant results have been achieved for many diseases[8]. Therefore, this study was based on the basic pathogenesis of early DN with Qi and Yin insufficiency, dampness and heat, the application of sitagliptin tablets with Yiqi yangyin huoxue decoction for the treatment of early DN patients, an observation of its clinical impact on early DN patients, and its influence on blood rheology for early clinical intervention and to delay the progression of DN.
Through a retrospective analysis, 123 patients with early DN admitted to the endocrinology clinic of the Changzhou NO. 7 People’s Hospital from January 2021 to October 2022 were selected as the study participants. After rigorous screening, 100 patients with early DN were enrolled. The control group (CG, n = 50) and the observation group (OG, n = 50) were divided according to the treatment method.
The inclusion criteria were as follows: (1) All patients were between 18 and 75 years of age, independent of sex; (2) All patients met the diagnostic criteria for T2DM; and (3) Baseline data, clinical characteristics, laboratory indicators, and other data of all patients were complete. The exclusion criteria were as follows: (1) Patients with type 1 DM or other special types of DM; (2) Patients with infectious diseases, liver disease, cardiovascular disease, urinary system diseases, and kidney diseases; (3) Patients with malignant tumors; (4) Those unable to cooperate in clinical treatment or with mental illness; (5) Pregnant or lactating women; (6) Recent cases of diabetic ketoacidosis; and (7) Patients whose renal lesions were not induced by DM.
Diagnostic criteria for T2DM were as follows, based on the 1999 World Health Organization expert consultation report[9,10]: (1) Typical diabetes symptoms (polydipsia, polyuria, polyphagia, unexplained weight loss) plus random blood glucose ≥ 11.1 mmol/L; (2) Fasting blood glucose (FBG) ≥ 7.0 mmol/L; and (3) Oral glucose tolerance test 2 h blood glucose test ≥ 11.1 mmol/L, for patients without diabetes symptoms, which needed to be repeated on another day. Diagnostic criteria for early DN[11] were as follows: Referring to the 2012 updated Kidney Disease Outcomes Quality Initiative Clinical Practice Guidelines for Diabetes and Chronic Kidney Disease, excluding other causes (24 h infection, fever, congestive heart failure) of chronic kidney disease, the urine microalbumin (mg/L)/urine creatinine (g/L) (UACR) was significantly elevated in two of three consecutive examinations (30 mg/g ≤ UACR ≤ 300 mg/g). DN staging using the international universal Mogensen staging[12] was performed as follows: Mogensen I, II, and III stages represent early DN; the urinary albumin excretion rate in early DN was examined three consecutive times within 3 mo and was approximately 20–200 μg/min or 30–300 mg/d. Diagnostic criteria for TCM symptoms[13] were as follows: Consistent with Qi and Yin insufficiency and blood stasis syndrome, the main symptoms were turbid urine, dull complexion, hand-foot-heart heat, fatigue, limb edema, and low back pain; secondary symptoms were frequent urination, palpitations, dry throat, dry mouth, skin nails, and limb numbness; and the tongue pulse was as follows: Tongue thin, red or dark purple, sublingual vein, ecchymosis, and a weak or string pulse.
All enrolled participants received basic treatment as follows: (1) Diabetes health knowledge education, focusing on explaining the relevant knowledge of early DN to the participants and persuading patients to correctly understand and treat such diseases so that they can maintain a good mood throughout the treatment process; (2) Diet control, developing a high-quality, low-protein diet for each patient, a personalized diet plan, and a low-salt diet for patients with hypertension; (3) Exercise guidance, according to the specific circumstances of the patient, personalized exercise should be arranged for the patient to ensure that aerobic exercise and anaerobic exercises are performed alternately, with the exercise time for each patient being ≥ 150 min per week, thus gradually improving the exercise level of the patient; (4) Blood glucose-lowering therapy, based on the actual blood glucose status of the patient, oral medicine or insulin was selected and the blood glucose index was monitored in real time to ensure that it was stable and met the inclusion criteria; FBG was controlled between 5 and 8 mmol/L, and 2 h postprandial glucose (2 h PG) was controlled between 7 and 10 mmol/L; and (5) Symptomatic treatment, other treatments that did not interfere with the purpose of the study and non-angiotensin receptor blockers drugs were used to regulate blood pressure to ensure that this met the inclusion criteria.
The CG patients were treated with sitagliptin (Merck Sharp & Dohme Ltd., Chinese medicine approval word: J20140095, specification: 100 mg, seven tablets and four boards) at 100 mg/time, po, qd, and treatment was performed for 3 mo. OG patients were orally administered sitagliptin combined with Yiqi yangyin huoxue decoction daily in the morning and evening once each, after meals, and treatment was performed for 3 mo. The Yiqi yangyin huoxue decoction proposed by the investigator and the prescription composition are listed in Table 1.
| Type | Dosage, g |
| Astragalus | 20 |
| Chinese yam | 15 |
| Poria cocos | 10 |
| Dwarf lilyturf root | 10 |
| Danpi | 10 |
| Common peony root | 10 |
| Prepared Rehmannia root | 10 |
| Dogberry | 15 |
| Sealwort | 10 |
| Root of Zhejiang figwort | 10 |
| Ligusticum wallichii | 10 |
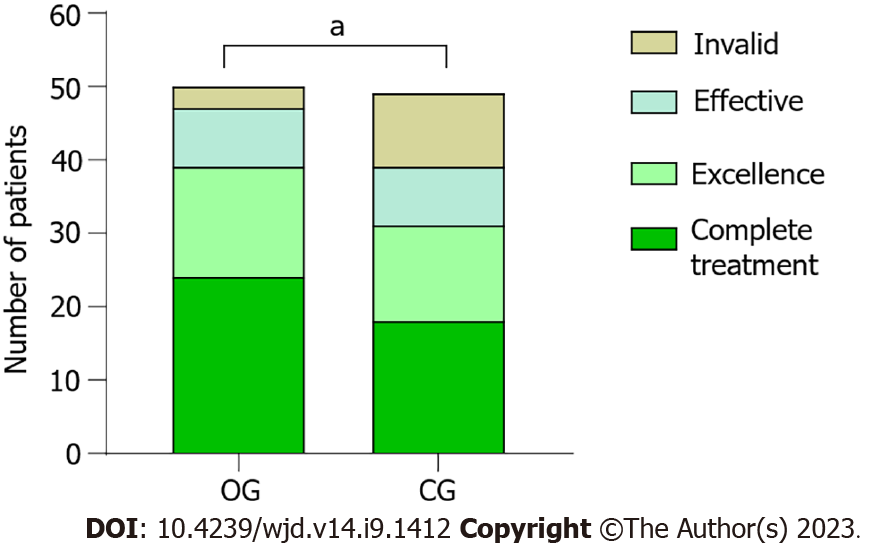
(1) General observation measures included sex, age, disease duration, systolic blood pressure (SBP), diastolic blood pressure (DBP), and body mass index (BMI); (2) Based on the Guiding Principles for Clinical Research on the Treatment of Diabetes with New TCM and the Guiding Principles for Clinical Research of New TCM in the Treatment of Chronic Nephritis, complete cure: 24 h urine albumin excretion rate (UAER) normal, renal function is normal; excellent: 24 h UAER reduced by 40%, normal or basically normal renal function; effective, 24 h UAER reduced by < 40%, renal function is normal or improved; invalid: Clinical manifestations and laboratory examination are not improved or aggravated; (3) Improvements in pre-treatment (T0) and posttreatment (T1) blood glucose levels, namely FBG and 2 h PG; (4) The blood lipid contents before treatment (T0) and after treatment (T1), namely total cholesterol, triacylglycerol, and low-density lipoprotein cholesterol (LDL-C), were compared between the two groups; (5) Pre-and post-treatment (T0) renal functions, including improvements in cystatin C (Cys-C), homocysteine (HCY), urinary microalbumin (U-mAlb), and blood creatinine (Cr) levels, were also compared; and (6) Blood rheological indices before (T0) and after treatment (T1), including changes in red blood cell deposition, plasma viscosity, high resection viscosity of whole blood, and low resection viscosity of whole blood, were assessed.
Data were analyzed using SPSS statistical software version 25.0. The measurement data were expressed as the mean ± SD and analyzed based on a t-test. Count data are expressed as the frequency percentage (n%) and were compared by performing a χ2 test. Statistical significance was set at P < 0.05.
The number of patients included and the flow chart of the analysis method are shown in Figure 1. There was no statistically significant difference in gender, age, course of disease, SBP, DBP, and BMI clinical data between the two groups of patients (P > 0.05) are presented in Table 2.
| Index | OG (n = 50) | CG (n = 50) | χ2/t value | P value |
| Sex (male/female) | 28/22 | 26/24 | 0.161 | 0.688 |
| Age (yr) | 51.24 ± 4.43 | 51.28 ± 4.28 | −0.046 | 0.963 |
| Disease course (yr) | 1.48 ± 0.47 | 1.49 ± 0.57 | −0.188 | 0.851 |
| SBP (mmHg) | 123.47 ± 10.28 | 124.16 ± 11.33 | −0.319 | 0.750 |
| DBP (mmHg) | 78.26 ± 4.15 | 79.51 ± 4.36 | −1.480 | 0.142 |
| BMI (kg/m2) | 25.21 ± 1.27 | 25.19 ± 1.44 | 0.038 | 0.970 |
After 3 mo of treatment, the total effective rate was 94.00% for OG patients; the total effective rate was 80.00% for CG patients, the difference between the two groups is statistically significant (P < 0.05; Figure 2).
After treatment (T1), the FBG and 2 h PG levels in the OG patients were markedly lower than those in the CG patients (P < 0.05; Figure 3).
At T0, a comparison of TC, TG, and LDL-C contents was not significantly differ between the two groups (P > 0.05), and at T1, the contents of TC, TG, and LDL-C in the OG were markedly lower than those in the CG (P < 0.05; Table 3).
| Group | Time | OG (n = 50) | CG (n = 50) | t-value | P value |
| TC (mmol/L) | T0 | 7.05 ± 1.21 | 7.08 ± 1.19 | −0.166 | 0.868 |
| T1 | 4.97 ± 0.73 | 6.13 ± 0.84 | −7.366 | < 0.001 | |
| TC (mmol/L) | T0 | 1.65 ± 0.17 | 1.63 ± 0.14 | 0.637 | 0.525 |
| T1 | 1.32 ± 0.28 | 1.49 ± 0.21 | −3.475 | < 0.001 | |
| LDL-C (mmol/L) | T0 | 4.13 ± 0.68 | 4.09 ± 0.71 | 0.219 | 0.827 |
| T1 | 1.87 ± 0.42 | 2.45 ± 0.67 | −5.196 | < 0.001 |
At T0, serum Cys-C, HCY, mAlb, and Cr contents was not significantly differ between the two groups (P > 0.05); however, At T1, serum Cys-C, HCY, U-mAlb, and Cr values of patients in the OG were markedly lower than those of patients in the CG (P < 0.05; Table 4).
| Group | Time | OG (n = 50) | CG (n = 50) | t-value | P value |
| Cys-C (mg/L) | T0 | 1.59 ± 0.43 | 1.57 ± 0.45 | 0.333 | 0.74 |
| T1 | 1.57 ± 0.45 | 1.48 ± 0.39 | −2.566 | 0.012 | |
| HCY (μmol/L) | T0 | 30.41 ± 5.73 | 30.44 ± 5.69 | −0.018 | 0.986 |
| T1 | 19.28 ± 3.15 | 22.36 ± 4.28 | −4.097 | < 0.001 | |
| U-mAlb (mg/L) | T0 | 195.67 ± 15.28 | 195.73 ± 15.14 | −0.017 | 0.987 |
| T1 | 162.38 ± 11.54 | 174.63 ± 13.45 | −4.887 | < 0.001 | |
| Cr (μmol/L) | T0 | 102.54 ± 9.47 | 102.71 ± 9.24 | −0.096 | 0.924 |
| T1 | 89.24 ± 7.36 | 96.53 ± 8.47 | -4.591 | < 0.001 |
At T1, erythrocyte deposition, plasma viscosity, whole blood high shear viscosity, and whole blood low shear viscosity in the OG were markedly lower than those in the CG (P < 0.05; Table 5).
| Group | Time | OG (n = 50) | CG (n = 50) | t-value | P value |
| Red blood cell deposition (%) | T0 | 46.88 ± 5.23 | 46.91 ± 5.19 | −0.029 | 0.977 |
| T1 | 37.15 ± 4.13 | 43.96 ± 4.87 | −7.542 | < 0.001 | |
| Plasma viscosity (mPa·s) | T0 | 3.26 ± 0.38 | 3.29 ± 0.43 | −0.490 | 0.625 |
| T1 | 1.52 ± 0.25 | 2.27 ± 0.31 | −13.465 | < 0.001 | |
| Whole blood high shear viscosity (mPa·s) | T0 | 5.94 ± 1.13 | 5.59 ± 1.07 | 1.598 | 0.113 |
| T1 | 4.06 ± 0.75 | 5.13 ± 0.81 | −6.854 | < 0.001 | |
| Whole blood low shear viscosity (mPa·s) | T0 | 10.29 ± 2.34 | 10.33 ± 2.29 | −0.108 | 0.914 |
| T1 | 7.70 ± 1.25 | 8.72 ± 1.64 | −3.527 | 0.001 |
The basic pathogenesis of diabetes is dryness-heat due to insufficiency. Qi Yin deficiency and meridian obstruction are the pathological causes of diabetes. The early stage of diabetes is dominated by Yin deficiency with heat excess, but when it progresses to the stage of DN, the disease is mostly at the stage of Qi and Yin insufficiency, and blood stasis becomes an important aspect of its pathogenesis[14]. Clinically, early DN is commonly characterized by the insufficiency of both Qi and Yin, as well as blood stasis of the venation. Its pathogenesis includes meridian infarction, blocked veins, and deficiency of both Qi and Yin. For DN (see TCM), the following are noted: Urinary turbidity, fatigue, hot hands and feet, dull complexion, swollen limbs, low back pain or frequent urination, palpitations and restlessness, dry throat and mouth, skin and nail lesions, numbness of limbs, tongue thinning and exhibiting a dark red or purple texture, tortuous sublingual veins, ecchymosis, and weak or astringent veins[15]. Therefore, the early detection of DN is beneficial for controlling disease progression. Owing to the poor efficacy of drug treatment alone, we used western medicine and TCM for targeted treatment.
This study shows that the clinical effectiveness of Yiqi yangyin huoxue decoction for the treatment of early DN, as well as that compared with conventional western medicine treatment. We found that the total response rate of patients in the OG was markedly better than that in the CG, indicating that sitagliptin and Yiqi yangyin huoxue decoction, used to treat early diabetic kidney disease, have a good synergistic effect, which can effectively relieve the clinical symptoms of early diabetic kidney disease, improve renal function, and reverse or delay early kidney injury. Our study also found that after treatment, compared with those before treatment, the levels of serum FBG, 2 h PG, TC, TG, and LDL-C were markedly lower in the OG compared to those in the CG. This shows that sitagliptin combined with Yiqi yangyin huoxue decoction can effectively reduce blood glucose and lipid levels, improve the state of hyperglycemia and hyperlipidemia, inhibit thrombosis formation, and slowed disease progression in patients with early DN. This could be because sitagliptin is a dipeptidyl peptidase-4 inhibitor. It is also a type of hypoglycemic drug that has an inhibitory effect on pancreatic islet α-cell hyperplasia and ultimately increases insulin secretion, such that blood sugar can be effectively regulated[16,17]. There are many drugs in the Yiqi yangyin huoxue decoction that have related effects. For example, when used in combination with astragalus and Rehmannia, blood sugar levels can be effectively reduced. By combining the tonifying effect of astragalus with the nourishing and kidney-strengthening effect of Rehmannia, the Qi and blood of the patient can also be replenished. Astragalus membranaceus can enhance immunity, help to resist oxidation, and have a certain regulatory effect on blood lipid and blood glucose levels in the body[18]. Further, Rehmannia glutinosa can improve hormone levels, especially the level of adrenaline, and has a certain improving effect on blood sugar and blood lipids in the body.
Oxidative stress reactions comprise one component of the pathogenesis of DN, and the reactive oxygen species produced by this reaction have an important impact on renal function. CysC is a small-molecule protein that is relatively stable in blood and is mostly used clinically to evaluate renal function. Moreover, it is an independent risk factor for diabetic complications. When renal function is impaired, serum levels increase significantly[19]. HCY is a non-essential amino acid with a sulfur-containing group, demethylated by methionine, and is closely related to renal function and metabolism. Research has shown that HCY can promote the excessive generation of oxygen free radicals and hydrogen peroxide, leading to the aggravation of renal tissue damage and acceleration of disease progression in DN[20]. U-mALB is a negatively charged protein secreted by the liver, and the vast majority of it fails to cross the glomerular filtration membrane charge barrier. An increase in urinary U-mALB content indicates altered glomerular permeability, and glomerular filtration membrane charge barrier is impaired[21]. Serum Cr is also a biochemical index used to evaluate renal function; its increase is related to a decrease in the glomerular filtration rate, and with this, renal function damage or renal failure is considered[22]. The results of our study showed that the levels of CysC, HCY, mALB, and Cr in the OG were markedly lower than those in the CG, indicating that sitagliptin combined with Yiqi yangyin huoxue decoction could reduce albuminuria, improve tubular function, and exert protective effects on renal function. Astragalus in Yiqi yangyin huoxue decoction can improve the balance of water and sodium in the body, change the permeability of blood vessels to reduce proteinuria, and effectively regulate renal function in patients with early DN[23]. Ligusticum wallichii can effectively prevent the production of advanced glycosylation end products in the renal cortex and inhibit the apoptosis of renal cells, thus improving renal function.
Microcirculation disorders are an important pathological basis of DN. Microangiopathy is the pathological basis of typical clinical manifestations, such as proteinuria, in patients with early DN[24]. Hemodynamic abnormalities are also important causes of proteinuria and glomerulosclerosis in patients with DN[25]. The results of this study showed that after treatment, the erythrocyte deposition, plasma viscosity, whole blood high shear viscosity, and whole blood low shear viscosity in the OG were markedly lower than those in the CG. This indicated that sitagliptin combined with Yiqi yangyin huoxue decoction could significantly improve blood rheological indices in patients with early DN. The Yiqi yangyin huoxue decoction uses A. membranaceus and prepared Rehmannia root as monarch drugs. Astragalus membranaceus has a slightly warm and sweet taste, which is beneficial for reducing water-swelling, supplementing Qi, consolidating the surface, strengthening the spleen, and tonifying the middle. The Rehmannia root is a processed product of R. glutinosa. It has sweet and bitter tastes and is beneficial for the heart, liver, and lung meridians. It nourishes the blood, promotes fluid production, clears heat, and cools the blood. When used in combination, it has the effect of strengthening Qi and Yin. The use of Chinese yam, Dogberry, Poria cocos, Sealwort, and Dwarf lilyturf root as medicinal herbs has a role in nourishing Qi in patients, and it is the main treatment for patients with spleen deficiency caused by fatigue and lumbar debility. The roots of Zhejiang figwort, Danpi, L. wallichii, and common peony root act as adjuvants, prevent thrombosis, improve hypercoagulability, promote blood circulation, and resolve blood stasis; after entering the body, they can improve blood viscosity, speed up blood flow, and reduce glomerular filtration, nourish the kidney, repair the kidney, and work together to complement each other, and thus, they have a marked influence on the treatment of diseases. Limitations of this study are as follows. Owing to time and sample size limitations, the selected subjects were all admitted to our hospital. Next, we will expand the sample size in clinical practice or conduct multicenter research and further explore the mechanism underlying the effects of Yiqi yangyin huoxue decoction for the treatment of early DN.
In conclusion, treatment with sitagliptin combined with Yiqi yangyin huoxue decoction in patients with Qi insufficiency and early DN has a significant effect, which is helpful in improving blood glucose, blood lipids, renal function, and hematological indicators and helping control disease progression, which is worthy of further clinical research.
Early diabetic nephropathy (DN) is a major complication of diabetes, a disease induced by glomerular sclerosis caused by a long-term glucose metabolism disorder. Progressive renal damage, edema, polyuria, and proteinuria are the main clinical symptoms of this disease. The main treatment plan comprising Western medicine for early DN is lipid-lowering and blood pressure regulation; however, the treatment effect is not good. Therefore, we used traditional Chinese medicine (TCM) to control disease progression from the root cause.
With the development of TCM, we already know that the main pathogenic mechanism of early DN is “Kidney deficiency and blood stasis, Qi and Yin insufficiency.” Therefore, we used western medicine combined with a TCM program for targeted treatment.
This study aimed to use sitagliptin tablets combined with Yiqi yangyin huoxue decoction to treat patients with early diabetic nephropathy, to observe the clinical efficacy and blood rheology in these patients, and to provide a basis for early clinical intervention to delay the progression of this disease.
Using a retrospective approach, patients with early DN were randomized into control group (CG) (n = 50) and observation group (OG) (n = 50). CG patients were treated with sitagliptin, and OG patients were treated with sitagliptin plus the Yiqi yangyin huoxue decoction. Both groups were treated for 3 mo.
The total response rate of the patients in the OG was 94.00%, and the total response rate of those in the CG was 80.00%. After treatment (T1), fasting blood glucose, 2 h postprandial glucose, total cholesterol, triacylglycerol, low-density lipoprotein cholesterol, cystatin C, homocysteine, urinary microalbumin, and blood creatinine levels in OG patients were markedly lower than those in the CG; further, red blood cell deposition, plasma viscosity, and hyperviscosity of whole blood in OG patients were markedly lower than those in the CG (all P < 0.05).
Sitagliptin combined with Yiqi yangyin huoxue decoction has achieved remarkable results in patients with early DN, helping to improve blood glucose, blood lipid, renal function, and hematological indicators.
In this retrospective study, patients with early DN were randomized into the CG and OG; the CG patients were treated with sitagliptin, and The OG patients were treated with sitagliptin plus Yiqi yangyin huoxue decoction; both groups were treated for 3 mo. Comparing the baseline data and clinical efficacy between the two groups, changes in blood glucose, blood lipid, renal function, and the hematology index were observed before (T0) and after treatment (T1). Thus, we explored the efficacy of sitagliptin in combination with Yiqi yangyin huoxue decoction for early DN treatment and its effect on blood rheology.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ceriello A, Italy; Olvera-Barrios A, United Kingdom S-Editor: Li L L-Editor: A P-Editor: Yu HG
| 1. | Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, Shi B, Sun H, Ba J, Chen B, Du J, He L, Lai X, Li Y, Chi H, Liao E, Liu C, Liu L, Tang X, Tong N, Wang G, Zhang JA, Wang Y, Xue Y, Yan L, Yang J, Yang L, Yao Y, Ye Z, Zhang Q, Zhang L, Zhu J, Zhu M, Ning G, Mu Y, Zhao J, Teng W, Shan Z. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 759] [Cited by in F6Publishing: 721] [Article Influence: 180.3] [Reference Citation Analysis (1)] |
| 2. | Lu WN, Li H. [The interpretation of national guidelines for the prevention and control of diabetes in primary care (2018), early diagnosis, standard evaluation and treatment of diabetic kidney disease]. Zhonghua Nei Ke Za Zhi. 2019;58:789-792. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 3. | Barrera-Chimal J, Jaisser F. Pathophysiologic mechanisms in diabetic kidney disease: A focus on current and future therapeutic targets. Diabetes Obes Metab. 2020;22 Suppl 1:16-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 4. | Aggarwal N, Kare PK, Varshney P, Kalra OP, Madhu SV, Banerjee BD, Yadav A, Raizada A, Tripathi AK. Role of angiotensin converting enzyme and angiotensinogen gene polymorphisms in angiotensin converting enzyme inhibitor-mediated antiproteinuric action in type 2 diabetic nephropathy patients. World J Diabetes. 2017;8:112-119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 7] [Cited by in F6Publishing: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Rando MM, Guthoff M, Tiwari V, Biscetti F. Editorial: Diagnosis, prevention and treatment in diabetic nephropathy. Front Endocrinol (Lausanne). 2022;13:1011665. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 6. | Kushiyama A, Kikuchi T, Tanaka K, Tahara T, Takao T, Onishi Y, Yoshida Y, Kawazu S, Iwamoto Y. Prediction of the effect on antihyperglycaemic action of sitagliptin by plasma active form glucagon-like peptide-1. World J Diabetes. 2016;7:230-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 2] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Scott R, Morgan J, Zimmer Z, Lam RLH, O'Neill EA, Kaufman KD, Engel SS, Raji A. A randomized clinical trial of the efficacy and safety of sitagliptin compared with dapagliflozin in patients with type 2 diabetes mellitus and mild renal insufficiency: The CompoSIT-R study. Diabetes Obes Metab. 2018;20:2876-2884. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Guo MF, Dai YJ, Gao JR, Chen PJ. Uncovering the Mechanism of Astragalus membranaceus in the Treatment of Diabetic Nephropathy Based on Network Pharmacology. J Diabetes Res. 2020;2020:5947304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Grimaldi A, Heurtier A. [Diagnostic criteria for type 2 diabetes]. Rev Prat. 1999;49:16-21. [PubMed] [Cited in This Article: ] |
| 10. | Roden M. [Diabetes mellitus: definition, classification and diagnosis]. Wien Klin Wochenschr. 2016;128 Suppl 2:S37-S40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis. 2012;60:850-886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 829] [Cited by in F6Publishing: 873] [Article Influence: 72.8] [Reference Citation Analysis (0)] |
| 12. | Mogensen CE, Schmitz A, Christensen CK. Comparative renal pathophysiology relevant to IDDM and NIDDM patients. Diabetes Metab Rev. 1988;4:453-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 53] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Dou Z, Xia Y, Zhang J, Li Y, Zhang Y, Zhao L, Huang Z, Sun H, Wu L, Han D, Liu Y. Syndrome Differentiation and Treatment Regularity in Traditional Chinese Medicine for Type 2 Diabetes: A Text Mining Analysis. Front Endocrinol (Lausanne). 2021;12:728032. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Liu XJ, Hu XK, Yang H, Gui LM, Cai ZX, Qi MS, Dai CM. A Review of Traditional Chinese Medicine on Treatment of Diabetic Nephropathy and the Involved Mechanisms. Am J Chin Med. 2022;50:1739-1779. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 15. | Sun GD, Li CY, Cui WP, Guo QY, Dong CQ, Zou HB, Liu SJ, Dong WP, Miao LN. Review of Herbal Traditional Chinese Medicine for the Treatment of Diabetic Nephropathy. J Diabetes Res. 2016;2016:5749857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 16. | Scott LJ. Sitagliptin: A Review in Type 2 Diabetes. Drugs. 2017;77:209-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 17. | Wang D, Zhang G, Chen X, Wei T, Liu C, Chen C, Gong Y, Wei Q. Sitagliptin ameliorates diabetic nephropathy by blocking TGF-β1/Smad signaling pathway. Int J Mol Med. 2018;41:2784-2792. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Tian H, Lu J, He H, Zhang L, Dong Y, Yao H, Feng W, Wang S. The effect of Astragalus as an adjuvant treatment in type 2 diabetes mellitus: A (preliminary) meta-analysis. J Ethnopharmacol. 2016;191:206-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Liu L, Wang H, Ning J, Han J, Yu C, Guan Q. The Predictability of Cystatin C for Peripheral Arterial Disease in Chinese Population with Type 2 Diabetes Mellitus. J Diabetes Res. 2022;2022:5064264. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 20. | Ding S, Yang Y, Zheng Y, Xu J, Cheng Y, Wei W, Yu F, Li L, Li M, Wang M, Wang Z, Xiang G. Diagnostic Value of the Combined Measurement of Serum HCY and NRG4 in Type 2 Diabetes Mellitus with Early Complicating Diabetic Nephropathy. J Pers Med. 2023;13. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 21. | Song LL, Wang N, Zhang JP, Yu LP, Chen XP, Zhang B, Yang WY. Postprandial glucagon-like peptide 1 secretion is associated with urinary albumin excretion in newly diagnosed type 2 diabetes patients. World J Diabetes. 2023;14:279-289. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 22. | Qi MY, He YH, Cheng Y, Fang Q, Ma RY, Zhou SJ, Hao JQ. Icariin ameliorates streptozocin-induced diabetic nephropathy through suppressing the TLR4/NF-κB signal pathway. Food Funct. 2021;12:1241-1251. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 23. | Lu Z, Zhong Y, Liu W, Xiang L, Deng Y. The Efficacy and Mechanism of Chinese Herbal Medicine on Diabetic Kidney Disease. J Diabetes Res. 2019;2019:2697672. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 24. | Verma N, Liu M, Ly H, Loria A, Campbell KS, Bush H, Kern PA, Jose PA, Taegtmeyer H, Bers DM, Despa S, Goldstein LB, Murray AJ, Despa F. Diabetic microcirculatory disturbances and pathologic erythropoiesis are provoked by deposition of amyloid-forming amylin in red blood cells and capillaries. Kidney Int. 2020;97:143-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 25. | Lee S, Lee MY, Nam JS, Kang S, Park JS, Shin S, Ahn CW, Kim KR. Hemorheological Approach for Early Detection of Chronic Kidney Disease and Diabetic Nephropathy in Type 2 Diabetes. Diabetes Technol Ther. 2015;17:808-815. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |