Copyright
©The Author(s) 2023.
World J Diabetes. Jan 15, 2023; 14(1): 26-34
Published online Jan 15, 2023. doi: 10.4239/wjd.v14.i1.26
Published online Jan 15, 2023. doi: 10.4239/wjd.v14.i1.26
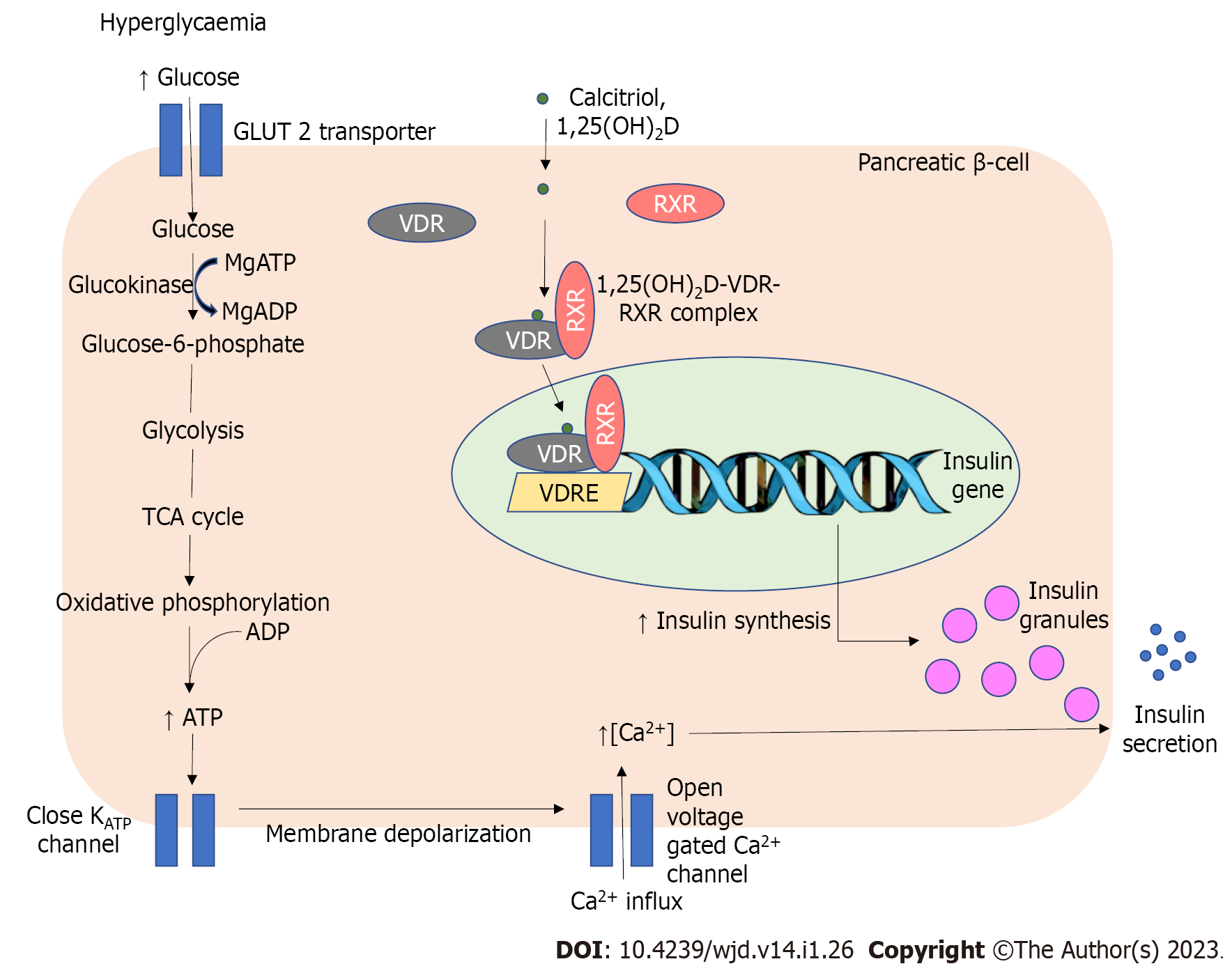
Figure 1 Interrelation of vitamin D and magnesium in the regulation of insulin synthesis and release from pancreatic β-cells.
Calcitriol, an activated form of vitamin D, enters pancreatic β-cells and binds to vitamin D receptors (VDR) to form a heterodimer complex with retinoid X receptor (RXR). The calcitriol-VDR-RXR complex later binds to the vitamin D response element which is located in the promoter region of the insulin gene in the nucleus. This is followed by increased insulin gene transcription to enhance its synthesis. Magnesium in the form of magnesium adenosine triphosphate and magnesium adenosine diphosphate plays vital roles in regulating glucokinase, an enzyme that converts glucose to glucose-6-phosphate. Adequacy of intracellular magnesium level is paramount to allow optimal glucokinase activity. The subsequent process in glycolytic pathway, tricarboxylic acid cycle, and oxidative phosphorylation yields adenosine triphosphate (ATP). The rise in ATP results in the closure of potassium-ATP-channel which increases intracellular potassium level. The resulting membrane depolarization causes the opening of voltage-gated calcium channel that triggers insulin degranulation and secretion. GLUT 2: Glucose transporter type 2; RXR: Retinoid X receptor; VDRE: Vitamin D response element; MgATP: Magnesium adenosine triphosphate; MgADP: Magnesium adenosine diphosphate; ATP: Adenosine triphosphate; Ca2+: Calcium; TCA: Tricarboxylic acid; ADP: Adenosine diphosphate; KATP: Potassium-ATP-channel; VDR: Vitamin D receptors; 1,25(OH)2 D: 1,25-dihydroxy vitamin D.
- Citation: Wan Nik WNFH, Zulkeflee HA, Ab Rahim SN, Tuan Ismail TS. Association of vitamin D and magnesium with insulin sensitivity and their influence on glycemic control. World J Diabetes 2023; 14(1): 26-34
- URL: https://www.wjgnet.com/1948-9358/full/v14/i1/26.htm
- DOI: https://dx.doi.org/10.4239/wjd.v14.i1.26