Copyright
©The Author(s) 2022.
World J Diabetes. Oct 15, 2022; 13(10): 835-850
Published online Oct 15, 2022. doi: 10.4239/wjd.v13.i10.835
Published online Oct 15, 2022. doi: 10.4239/wjd.v13.i10.835
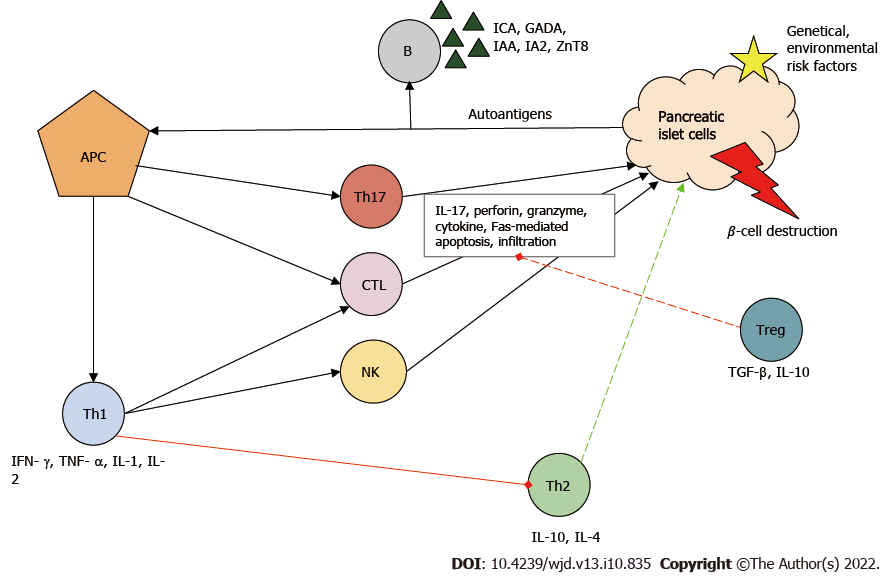
Figure 1 Immunopathogenesis of type 1 diabetes mellitus.
Autoantigens from pancreatic islet β-cells are presented by antigen-presenting cells (APCs), thereby activating T cells including helper T (Th) cells type 1 and type 17 and cytotoxic T lymphocytes (CTLs). Th type 1 cells play a key role in the development of the autoimmune response. They stimulate the activity of inflammatory T cells, macrophages and natural killer (NK) cells by producing proinflammatory cytokines and stimulate B cells (B), which produces autoantibodies and inhibits the protective Th type 2 cell function. Together, these immune cells contribute to the destruction of pancreatic β-cells. Red line: Inhibition; Green line: Stimulation. GADA: Glutamic-acid-decarboxylase antibody; IA2: Islet tyrosine phosphatase 2 antibody; IAA: Insulin autoantibody; ICA: Islet cell antibody; IL: Interleukin; IFN-γ: Interferon γ; TGF-β: Transforming growth factor β; TNF-α: Tumor necrosis factor α; Treg: Regulatory T cell; ZnT8: Zinc transporter 8 antibody.
- Citation: Nagy G, Szekely TE, Somogyi A, Herold M, Herold Z. New therapeutic approaches for type 1 diabetes: Disease-modifying therapies. World J Diabetes 2022; 13(10): 835-850
- URL: https://www.wjgnet.com/1948-9358/full/v13/i10/835.htm
- DOI: https://dx.doi.org/10.4239/wjd.v13.i10.835