Published online Jul 16, 2017. doi: 10.4253/wjge.v9.i7.341
Peer-review started: November 13, 2016
First decision: March 8, 2017
Revised: April 5, 2017
Accepted: April 18, 2017
Article in press: April 19, 2017
Published online: July 16, 2017
We report a case of an infant with Menkes’ disease (MD) presented at the age of five months, with coffee ground vomiting, melaena with a significant drop of haemoglobin. Urgent endoscopic assessment revealed a friable bleeding trans-pyloric multi-lobulated sessile polyp. Due to further significant upper gastrointestinal bleeding, polypectomy occurred. Endoscopic mucosal resection was performed with a grasp-and-snare technique using a dual channel operating gastroscope. Haemostasis was achieved by application of argon plasma coagulation where required. No perforation occurred. Repeated debridement was required 6 wk after which the growth was excised completely with no further blood transfusion required after that procedure. Histological examination confirmed ulcerated and inflamed hyperplastic polyp. We discuss our endoscopic technique and discuss the reported gastrointestinal manifestation of MD in the literature.
Core tip: Infant with Menkes’ disease can present with a potentially life threatening bleeding from hyperplastic gastric polyp. Removing hyperplastic polyp in those infants using grasp and snare technique is feasible and can avoid unnecessary surgical excision in those children.
- Citation: Belsha D, Narula P, Urs A, Thomson M. Management of hyperplastic gastric polyp following upper gastrointestinal bleeding in infant with Menkes’ disease. World J Gastrointest Endosc 2017; 9(7): 341-345
- URL: https://www.wjgnet.com/1948-5190/full/v9/i7/341.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i7.341
Menkes’ disease (MD) is a rare metabolic disease secondary to copper deficiency. It usually presents within the first year of life. Failure to thrive, neurological deficits, and seizures, along with subdural haematomas, connective tissue abnormalities and bony changes are classical features of MD[1]. Gastrointestinal disorder had been reported in MD including gastrointestinal bleeding. Surgical intervention is the only described treatment in the management due to the challenges of endoscopic management in the first year of life.
A Caucasian boy was born of an unrelated couple after an uncomplicated pregnancy. He was vaginally delivered at 39-wk gestation with a birth weight of 2880 g. At birth, no abnormal physical findings were recorded. At one month of age, he was referred because of two cephalohaematoma. Further examination revealed mild dysmorphic features including bilateral adducted thumbs, pectus excavatus, lax skin, moderate hypotonia and bilateral inguinal herniae. In view of mild respiratory distress a chest X-ray was performed and revealed two posterior rib fractures. Following that a skeletal survey was performed and revealed a Wormian bone raising the suspicion of MD. Further physical examination showed bronze and steely hair. The diagnosis of MD was made based on a serum copper level of 0.6 (reference range 5.9-16.3 mg/dL), and confirmed by positive genetic testing for the ATP7A gene. He developed epilepsy which was treated with anti-convulsants. In addition, an echocardiogram revealed aortic stenosis and abdominal US showed bladder diverticuli.
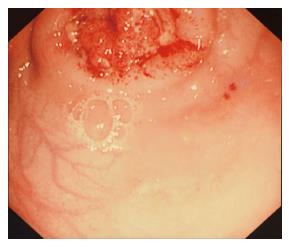
Subcutaneous copper histidinate therapy was introduced at around 8 wk of life. He was nasogastrically fed due to concerns regarding safe swallowing. At the age of five months, he presented with multiple coffee ground vomiting episodes and evidence of aspiration. Initially this was assumed to be secondary to gastro-oesophageal reflux disease (GORD). He was managed conservatively with proton pump inhibitors and nasojejunal feeding. At the age of six months and after a significant drop of haemoglobin from 10 mg/dL to 7.6 mg/dL associated with melaena, urgent endoscopic assessment revealed a friable bleeding trans-pyloric multi-lobulated sessile polyp of around 4 cm in diameter (Figure 1). The lesion was partially obstructing the pylorus but pyloric intubation was easily performed. Histological examination of the biopsied sample was suggestive of hyperplastic polyp.
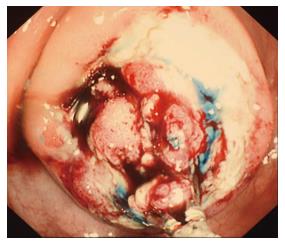
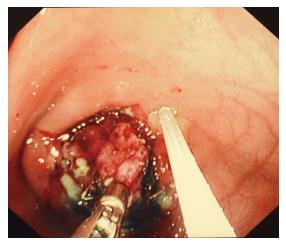
Due to further significant upper gastrointestinal (GI) bleeding polypectomy occurred. Tissue lifting was achieved with plasma expander mixed with adrenaline and methylene blue. Piecemeal polypectomy was the procedure of choice (Figure 2). Due to the difficulty in lifting up such a folded and small area, endoscopic mucosal resection was performed with a grasp-and-snare technique (20 mm eccentric snare and crocodile grasping forceps) using a dual channel operating gastroscope (Erbe Endocut level 1 and 2); the snare was connected to the ERBE and placed down channel one of the dual scope whereas the grasping forceps was down channel two (Figure 3). Table 1 describes the required equipment for the procedure.
| GIF-XQ 260; Olympus Optical Co. , Ltd |
| Dual channel operating scope (2TQ260M), Olympus Optical Co., Ltd |
| Argon plasma coagulator and ERBE electraucatery |
| Argon catheter. 1500 A, 1.5 mm, ERBE electraucautery. |
| Polyloop (2.8 mm channel); Olympus® |
| 25 mm eccentric snare( 1.8 mm channel); Quick Clip® |
| Clip applicators (single use rotatable clip fixing devise), Olympus® Resolution clip, Boston Scientific® |
| Rat toothed grasper, Olympus® |
| Roth net, 2.5 mm, 3 cm, US endoscopy® |
| Injection needle, 2.8 mm, 155 cm, Olympus® |
| 50 mL syringe |
| Succinylated Gelatin, Volplex® |
| Methelionum blue |
| Adrenaline 1 in 10000 |
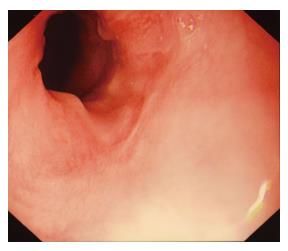
Haemostasis was achieved by application of argon plasma coagulation where required (Figure 4). No perforation occurred. Repeated endoscopic debridement was required 6 wk after which finally excised the growth (Figure 5) with no further blood transfusion required after that procedure. Histological examination of the polyp revealed granulation tissue with fibrosis and neovascularisation of the submucosa with evidence of an ulcerated surface and hence the histological confirmation of ulcerated and inflamed hyperplastic polyp.
Connective tissue abnormalities in MD are caused by decreased lysyl oxidase (LO) activity. LO is the copper dependent enzyme responsible for oxidative deamination of lysine and hydroxylysine as the first step in collagen cross-link formation and is low in this condition[2,3].
It has been hypothesized that the connective tissue weakness caused by LO deficiency creates a predisposition toward mucosal redundancy and hypertrophic polyp formation at the pyloric outlet, a site exposed to chronic localized pressure during gastric peristalsis[4].
Haematemesis in our patient can be explained by the presence of a polyp found in the pyloric region which acted as a ball-valve mechanism, causing intermittent obstruction to the gastric outlet. Exposure of the functional mucosa of this polyp in the alkaline media of the duodenum possibly resulted in continuous gastrin secretion and in turn hypergastrinaemia and erosion of the polyp leading to haematemesis[3].
Review of the literature reveals 4 similar cases of hypertrophic gastric polyps in MD: EMBASE, PubMed, and google scholar databases were searched from 1970 till now using the keywords “Menkes”, “gastrointestinal bleeding”, and or “polyp”.
First case presented at 3 and a half months with coffee ground emesis, upper GI endoscopy revealed an irregular growth around the posterior wall of the gastric antrum there which was managed conservatively as per his parental wishes. At seven months he had massive GI bleeding with melaena leading to hypovolemic shock and death. Post-mortem revealed an ulcerated polypoid mass obstructing the pyloric opening[4].
The second case presented at the age of 10 mo with haematemesis managed conservatively followed by large haematemesis eight months lated. Endoscopy revealed a large solitary ulcerated polypoid mass, again partially obstructing the pylorus. Surgical excision of the mass was performed successfully[4].
The third case was discovered at a post mortem examination of an 11-mo-old infant with MD and revealed an isolated hyperplastic gastric polyp located around the pyloric antrum[5].
The fourth was a Japanese boy with MD who developed multiple gastrointestinal polypoid masses on the palate, the posterior wall of the oropharynx, the gastric body, and pyloric antrum despite normal serum copper levels following copper therapy[6].
Hyperplastic polyps in infancy of such a large size with extensive involvement of the antrum and pylorus of the stomach are extremely rare[7]. Two previous report in non MD has been described in infancy period and required surgical resection secondary to hematemesis and obstructive symptoms[7,8]. Gastric polyps have been described in children receiving long term proton pump inhibitor (PPI) therapy as in our patient[9]; however, the majority of PPI-associated polyps are small (2-8 mm), with a partly translucent surface and usually located in the fundus or proximal in the gastric corpus. In most cases, these polyps appear to be fundic gland polyps, although in a minority hyperplastic and inflammatory polyps occur[10,11].
In Western countries, adults hyperplastic polyps constitute 20% of all gastric polyps and are sessile or pedunculated polyps of usually less than 2 cm in diameter. They can occur as single polyps usually in the antrum or as multiple polyps throughout the stomach[12]. Hyperplastic polyps of the gastric antrum are a rare but significant cause of gastrointestinal blood loss in older patients. Removal of the polyps using endoscopic or surgical methods may be required for resolution of the blood loss along with iron supplementation[13].
Though bleeding from hyperplastic gastric polyps is not well documented in adult series, a review by Al-Hadad et al[14] of all gastric polyps encountered in their centre revealed 1.4% to be hyperplastic polyps in the gastric antrum, of whom 35% presented with melaena and significant iron deficiency anaemia.
The British Society of Gastroenterology (BSG) recommends the removal of hyperplastic polyps > 1 cm whenever possible whilst multiple, or smaller ones can be biopsied and monitored annually. Biopsies should be taken of the intervening or surrounding mucosa and Helicobacter pylori eradicated when present[15].
To the best of our knowledge our case is the first reported in a child with MD to undergo endoscopic treatment of such a hyperplastic gastric polyp. In addition, and allowed by recent advances in endotherapeutic techniques, this is the first reported case of an infant of a weight of less than 6 kg that has undergone extended endoscopic submucosal dissection (ESD) using the grasp-and-snare technique.
In an adult series of 11 patients: The grasp-and-snare technique was used to perform EMR with good outcomes where sub-mucosal lifting and accessibility were problematic[16]. Complication rates are known to be higher after EMR and ESD relative to other basic endoscopic interventions[17]. In an adult series gastric lesions treated with EMR and ESD demonstrated complete resection in 73.9% and a combined complication rate of 1.9% (1.4% bleeding, 0.5% perforation)[18].
Of note our case also had significant GORD, which is noted to be more frequent in MD and in one case during open Nissen fundoplication, loose connective tissues were noted around the GOJ, especially the crura of the diaphragm[19]. GOR is probably one of the connective tissue manifestations od MD and may reflect a failure in elastin and collagen crosslinking caused by a decrease in the functional activity of copper-dependent LO. Defective elastic fibres within the internal elastic lamina, tunica media, and intimal layers of arteries and arterioles result in vascular tortuosity and ectasia with greater predisposition to mucosal haemorrhage[20].
This case identifies an unusual gastrointestinal complication of MD and for the first time shows the possibility of successful and uncomplicated EEMR even in very small infants.
Upper gastrointestinal bleeding in infants with Menkes’ disease (MD).
Hyperplastic gastric polyp.
Upper gastrointestinal endoscopy ruled out other diagnosis of gastrointestinal bleeding like gastric/ duodenal ulcers /erosive oesophagitis/erosive gastritis.
Low serum Copper level was documented. Patient had recurrent low haemoglobin level after bleeding episodes necessitating blood transfusions. The diagnosis was confirmed with upper gastroesophageal endoscopy.
Bleeding from ulcerated hyperplastic gastric polyp in the gastric antrum was the diagnosis as per endoscopic finding and the histological examinations.
The patient was treated endoscopically. Piecemeal polypectomy was the procedure of choice. Due to the difficulty in lifting up such a folded and small area, endoscopic mucosal resection was performed with a grasp-and-snare technique. Repeated debridement was required 6 wk after which the growth was excised completely with no further blood transfusion required after that procedure. Histological examination confirmed ulcerated and inflamed hyperplastic polyp.
Four similar cases of hypertrophic pyloric gastric polyps in MD were all presented in infancy period, two patients had fatal extensive bleeding and two managed with surgical excision of the pylorus.
Infants with MD can present with a potentially life threatening bleeding from hyperplastic gastric polyp. Endoscopic removal of the polyp infants using grasp and snare technique is feasible and can avoid unnecessary surgical excision in those children.
Nice case. Good literature review.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen MJ, Freeman HJ S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Bacopoulou F, Henderson L, Philip SG. Menkes disease mimicking non-accidental injury. Arch Dis Child. 2006;91:919. [PubMed] [Cited in This Article: ] |
| 2. | Siegel RC. Lysyl oxidase. Int Rev Connective Tiss Res. 1979;8:73-118. [DOI] [Cited in This Article: ] [Cited by in Crossref: 198] [Cited by in F6Publishing: 212] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Alper M, Akcan Y, Belenli O. Large pedinculated antral hyperplastic gastric polyp traversed the bulbus causing outlet obstruction and iron deficiency anemia: endoscopic removal. World J Gastroenterol. 2003;9:633-634. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 9] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Kaler SG, Westman JA, Bernes SM, Elsayed AM, Bowe CM, Freeman KL, Wu CD, Wallach MT. Gastrointestinal hemorrhage associated with gastric polyps in Menkes disease. J Pediatr. 1993;122:93-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Wheeler EM, Roberts PF. Menkes’s steely hair syndrome. Arch Dis Child. 1976;51:269-274. [PubMed] [Cited in This Article: ] |
| 6. | Sasaki G, Ishii T, Sato S, Hoshino K, Morikawa Y, Kodama H, Matsuo N, Takahashi T, Hasegawa T. Multiple polypoid masses in the gastrointestinal tract in patient with Menkes disease on copper-histidinate therapy. Eur J Pediatr. 2004;163:745-746. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Too SC, Sarji S A, Yik Y I, Sithasanan N, Singaravel S. Infantile Hyperplastic gastric polyps: a rare entity. Internet J of Paediatrics and Neonatology. 2009;In press. [Cited in This Article: ] |
| 8. | Brooks GS, Frost ES, Wesselhoeft C. Prolapsed hyperplastic gastric polyp causing gastric outlet obstruction, hypergastrinemia, and hematemesis in an infant. J Pediatr Surg. 1992;27:1537-1538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Pashankar DS, Israel DM. Gastric polyps and nodules in children receiving long-term omeprazole therapy. J Pediatr Gastroenterol Nutr. 2002;35:658-662. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Stolte M, Bethke B, Seifert E, Armbrecht U, Lütke A, Goldbrunner P, Rabast U. Observation of gastric glandular cysts in the corpus mucosa of the stomach under omeprazole treatment. Z Gastroenterol. 1995;33:146-149. [PubMed] [Cited in This Article: ] |
| 11. | el-Zimaity HM, Jackson FW, Graham DY. Fundic gland polyps developing during omeprazole therapy. Am J Gastroenterol. 1997;92:1858-1860. [PubMed] [Cited in This Article: ] |
| 12. | Carmack SW, Genta RM, Schuler CM, Saboorian MH. The current spectrum of gastric polyps: a 1-year national study of over 120,000 patients. Am J Gastroenterol. 2009;104:1524-1532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 189] [Cited by in F6Publishing: 205] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 13. | Stolte M, Sticht T, Eidt S, Ebert D, Finkenzeller G. Frequency, location, and age and sex distribution of various types of gastric polyp. Endoscopy. 1994;26:659-665. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 166] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | Al-Haddad M, Ward EM, Bouras EP, Raimondo M. Hyperplastic polyps of the gastric antrum in patients with gastrointestinal blood loss. Dig Dis Sci. 2007;52:105-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B; British Society of Gastroenterology. The management of gastric polyps. Gut. 2010;59:1270-1276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 192] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 16. | de Melo SW, Cleveland P, Raimondo M, Wallace MB, Woodward T. Endoscopic mucosal resection with the grasp-and-snare technique through a double-channel endoscope in humans. Gastrointest Endosc. 2011;73:349-352. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | ASGE Technology Committee, Kantsevoy SV, Adler DG, Conway JD, Diehl DL, Farraye FA, Kwon R, Mamula P, Rodriguez S, Shah RJ, Wong Kee Song LM, Tierney WM. Endoscopic mucosal resection and endoscopic submucosal dissection. Gastrointest Endosc. 2008;68:11-18. [PubMed] [Cited in This Article: ] |
| 18. | Kojima T, Parra-Blanco A, Takahashi H, Fujita R. Outcome of endoscopic mucosal resection for early gastric cancer: review of the Japanese literature. Gastrointest Endosc. 1998;48:550-554. [PubMed] [Cited in This Article: ] |
| 19. | Okada T, Sasaki F, Honda S, Miyagi H, Kubota M, Todo S. Menkes disease with gastroesophageal reflux disease and successful surgical treatment: a case report and literature review. Turk J Pediatr. 2010;52:333-335. [PubMed] [Cited in This Article: ] |
| 20. | Mandelstam SA, Fisher R. Menkes disease: a rare cause of bilateral inguinal hernias. Australas Radiol. 2005;49:192-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |