Published online Feb 16, 2017. doi: 10.4253/wjge.v9.i2.85
Peer-review started: July 12, 2016
First decision: September 9, 2016
Revised: October 8, 2016
Accepted: November 21, 2016
Article in press: November 22, 2016
Published online: February 16, 2017
Over-the-scope-clips (OTSC®) have been shown to be an effective and safe endoscopic treatment option for the closure of gastrointestinal perforations, leakages and fistulae. Indications for endoscopic OTSC® treatment have grown in number and also include gastro cutaneous fistula (GCF) after percutaneous endoscopic gastrostomy (PEG) tube removal. Non-healing GCF is a rare complication after removal of PEG tubes and may especially develop in immunosuppressed patients with multiple comorbidities. There is growing evidence in the literature that OTSC® closure of GCF after PEG tube removal is emerging as an effective, simple and safe endoscopic treatment option. However current evidence is limited to the geriatric population and short standing GCF, while information on closure of long standing GCF after PEG tube removal in a younger population with significant comorbidities is lacking. In this retrospective single-center case-series we report on five patients undergoing OTSC® closure of chronic GCF after PEG tube removal. Four out of five patients were afflicted with long lasting, symptomatic fistulae. All five patients suffered from chronic disease associated with a catabolic metabolism (cystic fibrosis, chemotherapy for neoplasia, liver cirrhosis). The mean patient age was 43 years. The mean dwell time of PEG tubes in all five patients was 808 d. PEG tube dwell time was shortest in patient 5 (21 d). The mean duration from PEG tube removal to fistula closure in patients 1-4 was 360 d (range 144-850 d). The intervention was well tolerated by all patients and no adverse events occured. Successful immediate and long-term fistula closure was accomplished in all five patients. This single center case series is the first to show successful endoscopic OTSC® closure of long lasting GCF in five consecutive middle-aged patients with significant comorbidities. Endoscopic closure of chronic persistent GCF after PEG tube removal using an OTSC® was achieved in all patients with no immediate or long-term complications. OTSC® is a promising endoscopic treatment option for this condition with a potentially high immediate and long term success rate in patients with multiple comorbidities.
Core tip: Over-the-scope-clips (OTSC®) are effective and safe for closure of gastrointestinal perforations, leakages and fistulae. There is growing evidence that OTSC® can be applied for the closure of gastro-cutaneous fistula after percutaneous endoscopic gastrostomy (PEG) tube removal. In this retrospective single-center case-series we report on five middle-aged patients with multiple comorbidities undergoing OTSC® closure of chronic gastro cutaneous fistula after PEG tube removal. The mean dwell time of PEG tubes was 808 d. Successful immediate and long-term fistula closure was accomplished in all five patients. OTSC® is a promising treatment for this condition with a high immediate and long-term success rate.
- Citation: Heinrich H, Gubler C, Valli PV. Over-the-scope-clip closure of long lasting gastrocutaneous fistula after percutaneous endoscopic gastrostomy tube removal in immunocompromised patients: A single center case series. World J Gastrointest Endosc 2017; 9(2): 85-90
- URL: https://www.wjgnet.com/1948-5190/full/v9/i2/85.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i2.85
The application spectrum of the over-the-scope-clip (OTSC®) has continually evolved from hemostasis to closure of gastrointestinal perforations, leakages and fistulae including anorectal lesions[1-7]. OTSC®s have been proven to be an effective and safe endoscopic treatment option in these conditions[2,8-10]. Emerging indications include fixation of self-expandable metallic stent (SEMS) and diameter reduction of gastrojejunal anastomosis after gastric bypass.
Non-healing gastrocutaneous fistula (GCF) is a rare complication after removal of percutaneous endoscopic gastrostomy (PEG) tubes and can be treated surgically or endoscopically[11]. Clip application, suture, gluing, banding[12] and coagulation techniques have been described as endoscopic therapeutic options[13-17]. Nevertheless, OTSC® application is emerging as a simple and safe endoscopic treatment for persistent GCF.
Even though various risk factors for the development of GCF such as stomal infection, delayed gastric emptying, acid hypersecretion, malnutrition, catabolic metabolism, tumors, immunosuppression and consecutive impaired wound healing have been discussed, the only evidence-based risk factor is a duration of gastrostomy > 6 mo leading to epithelialization and persistence of the gastrostomy channel[18,19]. Existing case series on OTSC® application for GCF closure generally focus on closure of short standing GCFs in the setting of infection in geriatric populations[2,8]. We here report on our experience with OTSC® closure of long standing GCF in middle-aged patients with significant comorbidities.
We report five cases of patients who were treated in one tertiary care center and underwent closure of persisting GCF after PEG tube removal. Since the OTSC® has been implemented into daily routine, five patients were referred to our clinic for endoscopic closure of persistent GCF after PEG tube removal. After thorough evaluation of each case and written informed consent by each patient, procedures were performed with flexible Olympus® endoscopes using carbon dioxide insufflation instead of ambient air.
The deployment of OTSC® has been published before[20]. A “bearclaw” like OTSC® clamped on a plastic cap is mounted onto the tip of the endoscope. The targeted lesion is then pulled into the plastic cap by suction. If the surrounding tissue is fibrotic and scarred a three-hook anchoring device (anchor® OVESCO Endoscopy AG, Tübingen) is used. The OTSC® is then deployed over the targeted lesion.
Primarily, the smallest, atraumatic (a) OTSC® (size 11 mm) was chosen in order to easily pass the upper esophageal sphincter and to minimize lacerations within the esophagus. In one patient, the largest OTSC® (size 14 mm) was necessary to achieve tight GCF closure after a size 12 OTSC® failed to do so. The small-sized OTSC® was removed with a standard rat-tooth forceps. No overtube was necessary to introduce the OTSC® mounted endoscope. Immediate evaluation of closure success was either proven endoscopically or utilizing contrast medium and inspection of the fistula orifice at skin level. Lasting closure success and subsequent complications were assessed clinically in the follow-up.
Between June 23rd 2009 and June 18th 2015, a total of 1373 PEG tubes were inserted at our clinic. We removed 231 of these PEG tubes in the follow-up. A total of 4 patients (0.29%) developed chronic GCF and were then referred to our unit for endoscopic closure (Table 1). Immediate OTSC® closure of the gastrostomy was performed upon PEG tube removal in a fifth patient due to ascitic fluid leakage. All 5 patients suffered from chronic disease associated with a catabolic metabolism (cystic fibrosis, chemotherapy for neoplasia, liver cirrhosis). Patients 2 and 3 had cystic fibrosis and required additional feeding through a PEG tube due to malnutrition. Patient 1, patient 4 and patient 5 suffered from tongue or oropharyngeal carcinoma, respectively and needed PEG-feeding during radio-chemotherapy. Patient 5 additionally suffered from refractory ascites due to decompensated liver cirrhosis. The mean age of the patients was 43 years. The mean duration of prior PEG treatment was 808 d (d) in all 5 patients while the time period was shortest in patient 5 (21 d).
| Age | Gender | Underlying condition | No. of previous PEG's | Date of first PEG | Date of PEG removal | Duration of PEG treatment | PEG complication | Age of GC fistula (d) | Previous antibiotics | OTSC type | Date of OTSC placement | Method | Successful immediate closure | Long term resolution of leak | Follow-up (d) | Complications | |
| Case 1 | 67 | F | Cerebral ischemia, tongue carcinoma | 3 | 23/07/09 | 20/01/11 | 546 | Chronic, recurrent infections with gastrocutaneus fistula | 203 | Yes | 11/3a | 11/08/11 | Suction and anchor | Yes | Yes | 1875 | No |
| Case 2 | 23 | F | Cystic fibrosis | 1 | 31/12/11 | 01/06/15 | 1248 | Persisting gastrocutaneus fistula | 241 | No | 11/6a | 28/01/16 | Suction | Yes | Yes | 244 | No |
| Case 3 | 23 | M | Cystic fibrosis | 1 | 30/07/12 | 18/06/15 | 1053 | Persisting gastrocutaneus fistula | 144 | No | 11/6a | 09/11/15 | Suction | Yes | Yes | 324 | No |
| Case 4 | 52 | F | Oropharyngeal carcinoma | 1 | 30/12/11 | 18/01/13 | 385 | Persisting gastrocutaneus fistula | 850 | No | 11/6a | 18/05/15 | Suction | Yes | Yes | 499 | No |
| Case 5 | 52 | M | Tongue carcinoma liver cirrhosis | 1 | 23/08/12 | 13/09/12 | 21 | Leaking gastrostomy due to ascites | NA | No | 14/6a | 13/09/12 | Suction | Yes | Yes | 1476 | No |
| Mean | 43 | 808 | 360 | 884 |
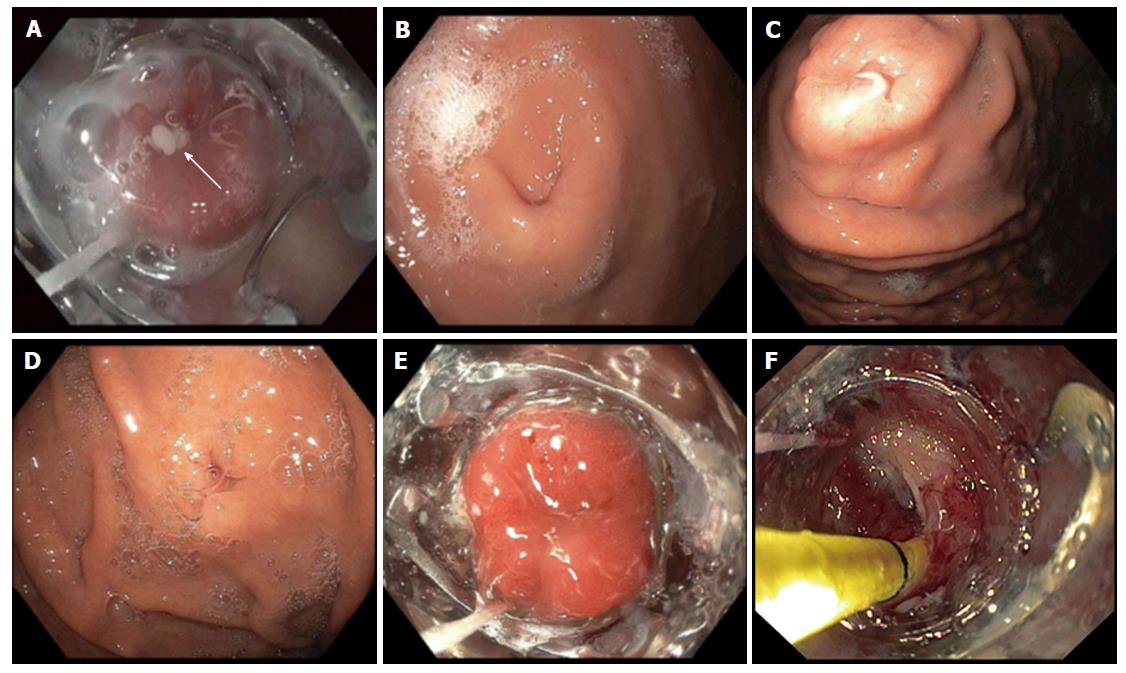
Patient 1 suffered from chronically infected PEG sites necessitating antibiotic treatment applying various different regimes and following two changings of the PEG site. Upon suction during OTSC® placement, pus drained through the fistula towards the endoscope (Figure 1). Three patients (patients 2-4) suffered from a chronically draining and persisting GCF after PEG tube removal. Patient 5 suffered from refractory ascites due to decompensated liver cirrhosis complicated by bacterial peritonitis following PEG insertion. Therefore, immediate and tight OTSC® closure of the gastrostomy was performed immediately after PEG tube removal.
The mean duration from PEG tube removal to fistula closure in patients 1-4 was 360 d (range 144-850 d).
A small sized OTSC® (size 11 mm) was sufficient in patients 1-4 to achieve successful and tight fistula closure. In patient 5, a size 12 mm OTSC® was chosen for the first closure attempt. After deployment, leakage of ascites into the stomach was noticed suggesting incomplete closure. Therefore, the 12 mm OTSC® was removed using a standard rat-tooth forceps. In a second attempt during the same procedure ascites-tight closure of the GCF was accomplished. In patient 1, we used suction and the anchoring device for appropriate clip deployment. Suction through the working channel of the endoscope alone was then sufficient for adequate clip placement in all the four cases that followed.
Successful immediate GCF closure was accomplished in all 5 patients. After a mean follow-up time of 746 d (range 186-1737 d), all five leaks showed persistent long-term fistula closure. All clips remained in place with some overgrowing granulation tissue, but patients were asymptomatic; no abdominal discomfort or pain was reported. No OTSC®-associated complications occurred and none of the clips had to be removed. On a skin level, scaring and retraction at the PEG site were minimal.
We present the first single-center case series showing successful endoscopic GCF closure using the OTSC® device in middle-aged patients suffering from severe comorbidities. Since the introduction of the PEG in 1980 by Gauderer et al[21] surgery has been the treatment of choice for persisting GCF. Before the introduction of the OTSC®, the endoscopic armamentarium for GCF closure comprised mainly clip application, suture, gluing and coagulation techniques[13-17]. Alongside with the evolution of interventional endoscopy, the OTSC® device has gained significant importance as a sophisticated closure tool for various gastrointestinal conditions. The classical indications for OTSC® treatment are gastrointestinal perforations[3], leakages[4], fistulae[5] and uncontrolled bleedings[22]. These classical indications have lately been broadened to include SEMS fixation[23], closure of Peroral Endoscopic Myotomy access[24] within the esophagus as well as diameter reduction of gastrojejunal anastomosis after gastric bypass[25]. As recently shown by our group in a large cohort[26], traumatic or inflammatory fistulae are the most challenging conditions in regards to closure success rate. OTSC® closure of persisting GCF after PEG tube removal is a specific subgroup within this fistula group and is thus not comparable to classic chronic GCF in other conditions in regards to closure efficacy. We argue, based on our results, that due to the removal of the inserted foreign body (PEG tube) and the absence of chronic inflammation, OTSC® closure in GCF is far more promising in regards to successful closure compared to self-developing inflammatory fistulae. Long-term immunosuppressive therapy is a known risk factor for impaired wound healing and might therefore promote persistence of GCF after PEG removal. Catabolic metabolism in chronically ill patients seems to have the same effect. Geriatric patients are prone to suffer from persisting GCF suggesting that age itself is a risk factor for impaired natural closure of the PEG tunnel. Our mean patient age (43 ± 24 years) was significantly lower compared to the only existing comparable case series by Singhal et al[2] (mean age 84.4 ± 8.75 years). Yet, all of our patients suffered from chronic disease associated with a catabolic metabolism. We therefore suggest, that the patients’ tissue regeneration was compromised allowing the PEG tunnel to persist after tube removal. Once a chronic GCF is triggered by an immunocompromised state of any origin, the GCF still differs much from conventional inflammatory fistulae in the gastrointestinal tract. This fact might be due to the integrity of the tissue surrounding the fistula orifice in GCF compared to the damaged surrounding tissue in inflammatory fistulae. Therefore, effective clip placement and persistent attachment is far more challenging in inflammatory fistulae. In addition to the immunocompromised state, four out five patients underwent a long-term PEG treatment (> 6 mo) as the main risk factor for developing persistent GCF after PEG tube removal[18,19].
Portal hypertension with tense ascites is known to hinder closure of abdominal wall fistulae[27,28]. We therefore decided to immediately close the GCF in patient 5 after PEG tube removal. Whether or not previous gastropexies play a role in this particular setting is unknown. Since we so far only treated one patient with ascites for closure after PEG tube removal, a general recommendation cannot be given yet. Until there will be more data available in the future, individual solutions will need to be sought for.
Even though the number of patients in our case series is relatively small, our high closure success rate (100%) is in accordance with the success rate presented by Singhal et al[2] (90%). These results stand in clear contrast to the low long-term success rate of 30% published by our group for inflammatory fistulae[26]. Compared to Singhal et al[2], our follow-up period was clearly longer and shows that there is a low rate of long term failures after endoscopic fistula closure. Although the OTSC® is a foreign body with a drop-off rate of 0% in our case series, the clips did not induce any symptoms and no need for removal arose.
No major complications connected to the OTSC® treatment were recorded in our study. In one case, a too small-sized OTSC® was chosen initially and failed to achieve tight GCF closure. The clip was easily removed with a standard forceps and did not interfere with a second deployment of a larger sized OTSC®. In case of strong clip adherence or any other indication for clip removal, OVESCO Endoscopy AG (Tübingen) has introduced an OTSC® clip cutter system. In our large OTSC® cohort published previously, only a few minor complications occurred (in 6 out of 233 cases)[26]. These included accidental deployment of the OTSC® on the patients’ tongue in the very first cases and superficial mucosal laceration of the esophagus due to a too large-sized OTSC®.
In this case series, we adapted the clip size to the particular features of the GCF, the patient and the clinical setting. We used one size 14 clip, which can cause difficulties in passing the upper esophageal sphincter due to its large diameter. Compared to the study of Singhal et al[2] and Sulz et al[8], we included patients suffering from substantially more long standing GCF (mean fistula age = 360 d). Wright et al[29] performed electrocautery of the GCF before clip closure. Unfortunately, the authors did not discuss the reason for this step before OTSC® closure in their publication. One could hypothesize that the granulation tissue caused by electrocautery would promote GCF healing. Even though we did not perform this step, we were able to show that even epithelialized, long-lasting PEG fistulas should not be excluded from an endoscopic closure attempt using the OTSC® device.
In conclusion, endoscopic closure of persistent GCF after PEG tube removal using an OTSC® is a promising indication with a potentially high immediate and long term closure rate and with limited complications to be feared.
Five middle-aged patients with severe comorbidities developed gastro cutaneous fistula (GCF) after percutaneous endoscopic gastrostomy (PEG) tube removal. Four patients had long-standing symptomatic fistulas (mean PEG dwell time 808 d), while one patient developed a leaking gastrostomy due to ascites.
Over-the-scope-clips (OTSC®) application in the gastrointestinal tract is safe and effective in large variety of indications. There is evidence in the literature that OTSC application is safe and effective for endoscopic closure for GCF after PEG tube removal. However this evidence is mostly limited to a geriatric population with short standing GCFs.
This case series is the first to our knowledge to show safe and effective closure of GCF after PEG tube removal in a middle-aged patient population with severe comorbidities and long standing GCF.
OTSC application for GCF closure after PEG Tube removal.
The manuscript provides anecdotal support for the application of OTSC for long standing GCFs after PEG removal.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Switzerland
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Aly EH, Gonzalez-Ojeda A, Papavramidis TS, Rabago L, Wall J S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Kirschniak A, Subotova N, Zieker D, Königsrainer A, Kratt T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25:2901-2905. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Singhal S, Changela K, Culliford A, Duddempudi S, Krishnaiah M, Anand S. Endoscopic closure of persistent gastrocutaneous fistulae, after percutaneous endoscopic gastrostomy (PEG) tube placement, using the over-the-scope-clip system. Therap Adv Gastroenterol. 2015;8:182-188. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of gastrointestinal fistulae--a meta-analysis. Minim Invasive Ther Allied Technol. 2012;21:249-258. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Mennigen R, Colombo-Benkmann M, Senninger N, Laukoetter M. Endoscopic closure of postoperative gastrointestinal leakages and fistulas with the Over-the-Scope Clip (OTSC). J Gastrointest Surg. 2013;17:1058-1065. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Mercky P, Gonzalez JM, Aimore Bonin E, Emungania O, Brunet J, Grimaud JC, Barthet M. Usefulness of over-the-scope clipping system for closing digestive fistulas. Dig Endosc. 2015;27:18-24. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Prosst RL, Joos AK, Ehni W, Bussen D, Herold A. Prospective pilot study of anorectal fistula closure with the OTSC Proctology. Colorectal Dis. 2015;17:81-86. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Manta R, Manno M, Bertani H, Barbera C, Pigò F, Mirante V, Longinotti E, Bassotti G, Conigliaro R. Endoscopic treatment of gastrointestinal fistulas using an over-the-scope clip (OTSC) device: case series from a tertiary referral center. Endoscopy. 2011;43:545-548. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Sulz MC, Bertolini R, Frei R, Semadeni GM, Borovicka J, Meyenberger C. Multipurpose use of the over-the-scope-clip system (“Bear claw”) in the gastrointestinal tract: Swiss experience in a tertiary center. World J Gastroenterol. 2014;20:16287-16292. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc. 2014;80:610-622. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Mönkemüller K, Peter S, Toshniwal J, Popa D, Zabielski M, Stahl RD, Ramesh J, Wilcox CM. Multipurpose use of the ‘bear claw’ (over-the-scope-clip system) to treat endoluminal gastrointestinal disorders. Dig Endosc. 2014;26:350-357. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Schurr MO, Arezzo A, Ho CN, Anhoeck G, Buess G, Di Lorenzo N. The OTSC clip for endoscopic organ closure in NOTES: device and technique. Minim Invasive Ther Allied Technol. 2008;17:262-266. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Deen OJ, Parisian KR, Harris C, Kirby DF. A novel procedure for gastrocutaneous fistula closure. J Clin Gastroenterol. 2013;47:608-611. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Kumar N, Thompson CC. Endoscopic therapy for postoperative leaks and fistulae. Gastrointest Endosc Clin N Am. 2013;23:123-136. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Duddempudi S, Ghevariya V, Singh M, Krishnaiah M, Anand S. Treatment of persistently leaking post PEG tube gastrocutaneous fistula in elderly patients with combined electrochemical cautery and endoscopic clip placement. South Med J. 2009;102:585-588. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Farra J, Zhuge Y, Neville HL, Thompson WR, Sola JE. Submucosal fibrin glue injection for closure of recurrent tracheoesophageal fistula. Pediatr Surg Int. 2010;26:237-240. [PubMed] [Cited in This Article: ] |
| 16. | Willingham FF, Buscaglia JM. Endoscopic Management of Gastrointestinal Leaks and Fistulae. Clin Gastroenterol Hepatol. 2015;13:1714-1721. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Papavramidis TS, Mantzoukis K, Michalopoulos N. Confronting gastrocutaneous fistulas. Ann Gastroenterol. 2011;24:16-19. [PubMed] [Cited in This Article: ] |
| 18. | Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20:7739-7751. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Shellito PC, Malt RA. Tube gastrostomy. Techniques and complications. Ann Surg. 1985;201:180-185. [PubMed] [Cited in This Article: ] |
| 20. | Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-167. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Gauderer MW, Ponsky JL, Izant RJ. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872-875. [PubMed] [Cited in This Article: ] |
| 22. | Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162-3164. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Toshniwal J, Zabielski M, Fry LC, Mönkemüller K. Combination of the “bear claw” (over-the-scope-clip system) and fully covered stent for the treatment of post-operative anastomotic leak. Endoscopy. 2012;44 Suppl 2 UCTN:E288-E289. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Saxena P, Chavez YH, Kord Valeshabad A, Kalloo AN, Khashab MA. An alternative method for mucosal flap closure during peroral endoscopic myotomy using an over-the-scope clipping device. Endoscopy. 2013;45:579-581. [PubMed] [DOI] [Cited in This Article: ] |
| 25. | Heylen AM, Jacobs A, Lybeer M, Prosst RL. The OTSC®-clip in revisional endoscopy against weight gain after bariatric gastric bypass surgery. Obes Surg. 2011;21:1629-1633. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | Honegger C, Valli P, Wiegand N, Bauerfeind P, Gubler C. Establishment of Over-The-Scope-Clips (OTSC) in daily endoscopic routine. Unit Europ Gastroenterol J. 2016; Epub ahead of print. [DOI] [Cited in This Article: ] |
| 27. | Baltz JG, Argo CK, Al-Osaimi AM, Northup PG. Mortality after percutaneous endoscopic gastrostomy in patients with cirrhosis: a case series. Gastrointest Endosc. 2010;72:1072-1075. [PubMed] [DOI] [Cited in This Article: ] |
| 28. | Schrag SP, Sharma R, Jaik NP, Seamon MJ, Lukaszczyk JJ, Martin ND, Hoey BA, Stawicki SP. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16:407-418. [PubMed] [Cited in This Article: ] |
| 29. | Wright R, Abrajano C, Koppolu R, Stevens M, Nyznyk S, Chao S, Bruzoni M, Wall J. Initial results of endoscopic gastrocutaneous fistula closure in children using an over-the-scope clip. J Laparoendosc Adv Surg Tech A. 2015;25:69-72. [PubMed] [DOI] [Cited in This Article: ] |