Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.162
Peer-review started: August 23, 2014
First decision: November 18, 2014
Revised: December 10, 2014
Accepted: December 18, 2014
Article in press: December 19, 2014
Published online: March 16, 2015
Processing time: 209 Days and 15.7 Hours
The intentional ingestion of foreign objects (IIFO) is described more commonly in prison populations than in the general population, with an estimated annual incidence of 1 in 1900 inmates in our state correctional facilities. Incidents often involve ingestion of small metal objects (e.g., paperclips, razor blades) or other commonly available items like pens or eating utensils. Despite ingestion of relatively sharp objects, most episodes can be clinically managed with either observation or endoscopy. Surgery should be reserved for those with signs or symptoms of gastrointestinal perforation or obstruction. For those with a history of IIFO, efforts should focus on prevention of recurrence as subsequent episodes are associated with higher morbidity, significant healthcare and security costs. The pattern of IIFO is often repetitive, with escalation both in frequency of ingestions and in number of items ingested. Little is known about successful prevention strategies, but efforts to monitor patients and provide psychiatric care are potential best-practice strategies. This article aims to provide state-of-the art review on the topic, followed by a set of basic recommendations.
Core tip: Intentional ingestion of foreign objects typically involves ingestion of small objects (e.g., paperclips, razor blades, pens, eating utensils). Most episodes can be managed with either observation or endoscopy. Surgery should be reserved for those with signs or symptoms of gastrointestinal perforation or obstruction. Due to the documented pattern of escalation, efforts should focus on prevention of recurrence as subsequent episodes are associated with higher morbidity, and significant healthcare and security costs. There are no proven prevention strategies, but efforts to closely monitor patients and provide early psychiatric intervention are among recommended best-practice strategies.
- Citation: Evans DC, Wojda TR, Jones CD, Otey AJ, Stawicki SP. Intentional ingestions of foreign objects among prisoners: A review. World J Gastrointest Endosc 2015; 7(3): 162-168
- URL: https://www.wjgnet.com/1948-5190/full/v7/i3/162.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i3.162
Intentional ingestion of foreign objects (IIFO) is a serious problem that chronically affects the United States prison population. Although other non-prisoner patients, specifically those with severe psychiatric conditions, have been reported to have the propensity toward IIFO, the prison population seems unique in that the magnitude of the problem is especially high[1-3]. It has been estimated that up to 1500 deaths may be attributable to IIFO annually in the United States alone[4]. IIFO is a seemingly preventable phenomenon that is associated with high costs of care as well as security costs for transporting and guarding inmates while hospitalized[5]. Health care costs associated with IIFO accounted for $6.5 billion of the $36.8 billion spent to manage the correctional system budgets of 44 states[6]. In a recent study, IIFO episodes were associated with healthcare-related median charges between $4683 and $7698 for those evaluated in the emergency department and admitted[5]. Male sex, incarceration, and psychiatric disease are the predominant factors associated with IIFO[7].
The management of IIFO was revolutionized by the widespread adoption of endoscopic techniques that can be used for retrieval of accessible ingested objects[8]. The prisoner population presents unique challenges due to the multifactorial interaction of psychiatric disease, the (less likely) potential for secondary gain, and the escalating nature of recurrent IIFO. Inmates treated for IIFO often return after variable time intervals having ingested larger, more dangerous, or more toxic objects[2]. These extenuating factors should prompt careful consideration of treatment options as overly aggressive treatment can often lead to disastrous complications.
An exhaustive literature search was performed using the terms “foreign body ingestion”, “foreign object ingestion”, “intentional ingestion”, “swallowed object”, and “ingestion”. We utilized the United States National Library of Medicine NIH PubMed service, as well as Google™ Scholar to identify as many pertinent English literature sources as possible. After narrowing down the publication list to case reports, case series, reviews, retrospective and prospective studies, the search was further focused on epidemiology, diagnosis, management, and prevention as additional search terms. Results were tabulated, with all major studies on the topic published to date and compiled into a comprehensive, definitive list (Table 1).
The epidemiology of intentional foreign object ingestions continues to be poorly understood. Most literature focusing on foreign object ingestions is in the pediatric literature, where the size of the gastrointestinal (GI) tract is smaller and many objects become lodged in the pharynx or esophagus posing an aspiration, toxicity, or erosion risk[9-11]. Psychiatric and prison populations account for the majority of adults presenting with foreign object ingestions, the vast majority of which were non-accidental[2]. Due to the unique characteristics of these populations, relatively few of these patients tend to present to community hospitals. In the United States these patients are typically cared for in “safety net” hospitals, making IIFO a relatively high-frequency occurrence in select hospitals. While a general IIFO incidence in the community is not known, the annual incidence of IIFO requiring evaluation in the emergency room or hospital from 2006-2010 in the prison population in the State of Ohio was 0.0528% or approximately 1 in 1900 inmates, making the disease quite rare in this high risk population (see Table 1). Unfortunately in the prison population, recurrent ingestions are also relatively more common[2,5]. The epidemiology of recurrent IIFO is less well understood. Grimes et al[7] found no evidence that conscious sedation, esophageal pathology, or age had any statistical significance as a significant predictor of recurrent ingestion. Repeat ingestors are more likely to ingest foreign objects and less likely to experience food impaction[7]. Impulsivity, secondary gain, or an undiagnosed psychiatric disorder are possible explanations for ingestions in the prison population[7].
Several case series and observational studies of IIFO in adults have been published[1-4,7,8,13-20]. Many of these studies included prisoners, but some included a mix of general psychiatric patients as well. Table 2 summarizes the world published literature on adult IIFO. While children commonly ingest toys, coins, and loose household items, inmates and psychiatric patients are much more likely to ingest sharp and relatively dangerous objects such as blades, improvised shanks, and metal hardware and instruments. Table 3 reviews the types of objects frequently ingested in the published literature.
| Ref. | Year | Patients (n) | Not undergoing intervention | With psych dx | Surgery | Endoscopy | Objects ingested (n) |
| O’Sullivan et al[1] | 1996 | 36 (20 prisoners) | 31 (86) | 6 (16) | 2 (6) | 4 (11) | 308 |
| 1Dalal et al[2] | 2013 | 30 (141 episodes) | 33 (23) | 27 (19) | 11 (7) | 97 (68) | 649 |
| 1Weiland et al[3] | 2002 | 22 (256 episodes) | 23 (9) | 10 (4) | 64 (25) | 256 | |
| Barros et al[4] | 1991 | 167 (39 prisoners) | 14 (8) | 6 (3) | 51 (30) | 117 (70) | 167 |
| Selivanov et al[8] | 1984 | 100 | 42 (42) | 4 (6) | 12 (12) | 42 (42) | 101 |
| Blaho et al[13] | 1998 | 8 | 8 (100) | 6 (75) | 14 | ||
| Velitchkov et al[14] | 1996 | 542 (379 prisoners) | 410 (75) | 124 (23) | 26 (5) | 19 (3) | 1203 |
| Karp et al[15] | 1991 | 19 | 18 (95) | ||||
| 1Lee et al[17] | 2007 | 33 (52 episodes) | 0 | 6 (12) | 46 (88) | 104 | |
| Bisharat et al[18] | 2008 | 11 | 7 (63) | 3 (27) | 2 (18) | ||
| Huang et al[19] | 2010 | 33 | 4 (12) | 27 (81) | 2 (6) | 299 | 305 |
| Ribas et al[20] | 2014 | 82 | 142 | 62 (75) | 5 (6) | 15 (18) | 162 |
| Grimes et al[7] | 2013 | 159 (23 prisoners) | 34 (21) | 5 (3) | 231 | 254 | |
| Total | 2613 | 1014 (39) | 317 (12) | 190 (7) | 1129 (43) | 3153 |
| O’Sullivan et al[1] | Batteries, sharp metal objects (nails, razor blades, pins) |
| Dalal et al[2] | Pens, razor blades, spoons, sporks1, toothbrush, screws, bolts |
| Weiland et al[3] | Metal bezoars |
| Barros et al[4] | Wires, needles, balloons (filled with narcotics) |
| Selivanov et al[8] | Coins, bones, food, razor blades, safety pins |
| Blaho et al[13] | Razor blades |
| Velitchkov et al[14] | Screws, pins, spoons |
| Huang et al[19] | Pens, batteries, knives |
| Karp et al[15] | Razors, glass, toothbrush |
| Lee et al[17] | Metal wires, pens, toothbrush, needles |
| Bisharat et al[18] | Razors, batteries |
| Ribas et al[20] | Razor blades, cylindrical batteries, mattress springs |
| Grimes et al[7] | Toothbrush, pencil |
The costs of IIFO in the inmate population are high, especially when compared to the non-incarcerated population[21]. It has been estimated that the overall cumulative annual costs of IIFO in the majority (44 out of 50) United States states exceed $6 billion[6]. The majority of IIFO care costs can be broken down into nursing care (56%), endoscopy services (14%), emergency department care (10%), and surgical services (6%)[19]. Considering the above, IIFO episodes were associated with healthcare-related median charges between $4683 and $7698 for both emergency department evaluations and hospital admissions[5]. In the subset of patients who required hospital admission, median per-episode charges exceeded $14000[5]. Moreover, when repeated episodes of IIFO are factored in, estimated cumulative “lifetime” charges for patients studied in the same cohort were nearly $50000[5]. In addition there are the costs of security and transportation to the prison system because these patients have to be transported in a secure fashion, typically with multiple guards. While hospitalized, a guard must remain at the patient bedside. Hospitals also cover the cost of around-the-clock security for non-prisoner psychiatric patients. The estimated cost not reimbursed by third party payers for security was $278806 in Rhode Island over an eight year span[19].
Most ingestions are either self-reported by the inmate or witnessed by security staff. Patients presenting typically receive a plain X-ray to localize the object. Patients with normal vital signs and normal physical exam typically do not require additional imaging, even in the setting of sharp or other seemingly more dangerous objects.
Plain abdominal X-ray demonstrating free air is considered diagnostic for perforation. However, free air under the diaphragm is rarely seen because perforations are most commonly caused by impactions that have slowly eroded through the intestinal wall. These erosions are covered by fibrin, omentum, or adjacent loops of bowel limiting the passage of free air into the peritoneal cavity[22].
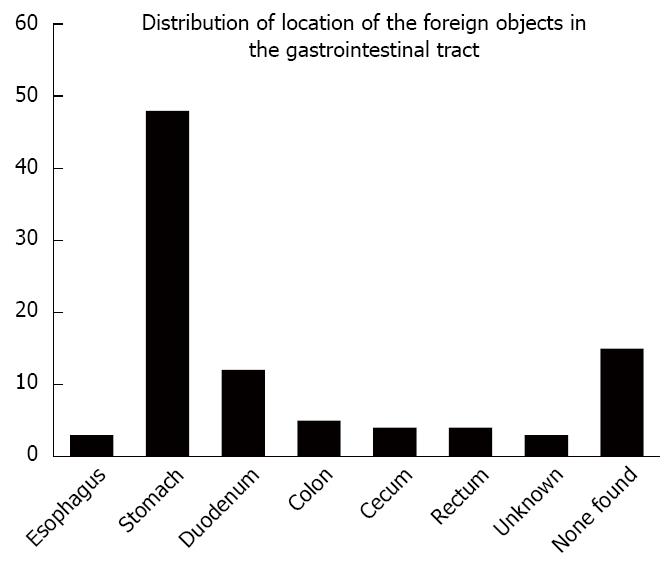
Patients with abdominal pain, fever, gastrointestinal bleeding, or other symptoms typically require CT scanning to evaluate for the presence of bowel perforation or other pathology. It has been shown that prisoners sometimes choose objects that will be visible on radiographs, wrap them in plastic or other materials to reduce the risk of injury, and then feign gastrointestinal symptoms[20]. Most objects are located in the stomach at the time of initial presentation (Figure 1). After initial X-ray, no additional workup is typically performed for radiolucent objects unless mandated by abnormal physical exam findings or vital signs.
Claimed or fictitious ingestions have been reported[13]. Although speculative, there are three possible explanations for this observed pattern: (1) some form of secondary gain may be present when an ingestion is claimed; (2) an actual ingestion may have occurred but the object ingested is not readily detectable or has already passed through the gastrointestinal system; or (3) the patient may be contemplating ingestion, but has not yet committed to this self-destructive behavioral pattern. It is important to note that healthcare-related median charges associated with verified (i.e., proven) ingestions are higher ($5860) than charges associated with claimed (i.e., fictitious) ingestions ($3997)[5].
Like any surgical emergency, initial management is typically based on physical examination and patient physiology. Patients with peritonitis typically require immediate surgical exploration[2]. Selective endoscopy is appropriate for many intragastric objects and can prevent progressive peristalsis of the object (with its associated dangers)[2,4,8]. In inmate and psychiatric populations surgical exploration should be avoided when possible as the benefits of operative removal often do not outweigh the risks of surgery. Drug and contraband smuggling, known as “body packing,” is another event that should be recognized. Ribas et al[20] reported on 36 patients attempting to smuggle cocaine by ingesting packets containing the drug. These “body packers” usually do not undergo endoscopy for fear of rupture and surgery is usually only performed if the patient develops symptoms. The operative course itself may be difficult due to the adhesions of previous laparotomies, often due to prior such incidents, and patients with the associated psychiatric comorbidities may have a difficult postoperative course.
In our practice there is a high rate of wound complications, self-inflicted wound mutilation (including self-inflicted evisceration of the midline laparotomy site), and non-compliance with physician orders (such as violation of nothing-by-mouth orders resulting in aspiration of gastric contents). Prisoners who develop complications of surgery for IIFO are at risk for the development of intestinal fistula and we have observed generally poor outcomes of both operative and non-operative management of fistulas in this population, with high rates of readmission, parenteral nutrition-associated line infections, abdominal wall infections, and non-healing wounds. In our previous work we reported the various management strategies employed for 141 episodes of IIFO in inmates (Table 4)[2].
| No intervention | 16% |
| Hospital admission | 10% |
| Surgery alone | 5% |
| Endoscopy + surgery | 3% |
| Endoscopy alone | 12% |
| Endoscopy (successful) | 54% |
In the vast majority of cases (approximately 67%-80%) expectant management will suffice, including watchful waiting and serial physical exams, with or without concurrent radiographic assessments[1,8,14]. Most of the foreign bodies that clear the stomach will spontaneously pass through the gastrointestinal system, frequently within a week[3,8]. Fortunately, many of the IIFO episodes end up being self-limited, and do not require formal hospital admission[22]. The need for admission is present in 7%-33% of patients[1,13]. In one series of 141 ingestions, the risk of hospital admission was independently associated with elevated white blood cell count [odds ratio (OR) 1.4] and increasing number of items ingested (OR 1.3)[2].
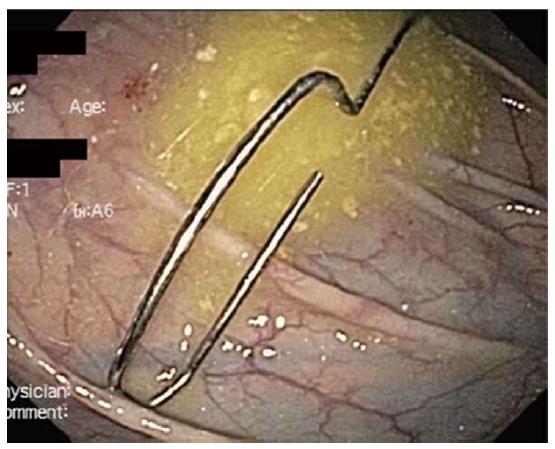
Endoscopy has revolutionized the management of IIFO. In fact, the forward-viewing flexible endoscope is the first option for retrieval of foreign objects in the stomach and duodenum[23]. Most ingested objects can be retrieved endoscopically, as long as they have not progressed beyond the ligament of Treitz. Successful endoscopic retrieval of IIFO has been reported in 19.5%-53.9% of cases[2,14]. Some of the more common objects retrieved by endoscopy are coins, bones, and impacted food[8]. In one study, the successful performance of endoscopy with retrieval of the IIFO has been found to reduce the risk of surgery by over 85%[2]. Having said that, endoscopy has also been associated with high failure rates and complications by others, thus warranting careful consideration when implementing this therapeutic option[3]. Grimes et al[7] found first time ingestors were more likely to have a food impaction compared to recurrent ingestors who were more likely to have ingested metal objects; however, recurrent ingestors experienced food impactions as well, commonly due to esophageal stricture[7]. In the same study one patient was found to be responsible for 67 ingestions (22%) of the ingestions. On average there were 9.2 episodes per patient. They also found that endoscopy was more successful in single ingestion patients, supporting the idea that the more times a patient ingests an object the more complex the ingestion becomes. Most objects that pass the ligament of Treitz are likely to pass through the entire GI tract. Rarely, small objects can become impacted in the colon. Endoscopy is frequently successful in removing those small objects such as the paperclip that was removed by the author (D.C.E.) depicted in Figure 2. While some sharp objects such as small razor blades can be removed endoscopically, particularly with the use of hoods, available endoscopic equipment and local practices may vary and we cannot draw any conclusions regarding recommendations for specific strategies for objects of various shapes, sizes, or sharpness.
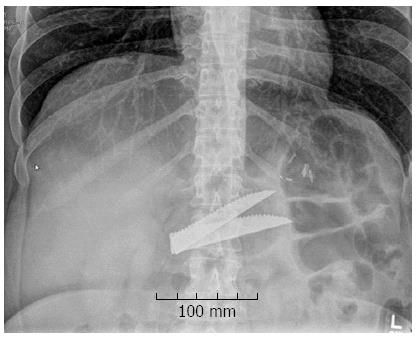
Operative intervention is required in up to 30% of IIFO cases[1,2,4,8,14], although more recent series report lower rates (i.e., < 15%) of operative intervention in this population[1,2]. In one large retrospective study, factors independently associated with risk of surgery in the setting of IIFO included elevated white blood cell count (OR 1.6) and increasing number of ingested items (OR 1.1 per item)[2]. Not surprisingly, failure of endoscopy has been associated with the need for subsequent operative intervention[4]. It has been noted that thinner, sharper foreign objects mandate a higher index of clinical suspicion due to higher perforation risk[14]. Also, surgery may be more likely in cases of proximally located IIFO, especially when the object is > 6-7 cm in largest dimension[14]. Previous surgery, obstruction, and narrowing all predispose to impaction of an object and increase the possible need for surgical intervention[22]. Long objects, such as the intragastric steak knife blades shown on abdominal X-ray (Figure 3), frequently require laparotomy. The author (D.C.E.) retrieved one blade endoscopically but the other became impacted at the esophageal hiatus and required laparotomy with gastrotomy for removal.
IIFO impaction is also possible, particularly in the ileo-cecal area[14]. The ileocecal region is particularly prone to obstruction by objects less than 6 cm that are able to maneuver through the duodenum[22]. Velitchkov et al[14] advocate an appendicostomy approach to retrieval of IIFO impacted in this location, however, most surgeons would prefer a simple enterotomy with foreign object retrieval, followed by repair of the enterotomy[14]. Figure 4 depicts small plastic-wrapped balls of narcotics removed from the terminal ileum by the author (D.C.E.) in a prisoner who was smuggling drugs by body packing. The patient developed an acute complete small bowel obstruction requiring emergent laparotomy. We performed a simple enterotomy in the ileum that was closed with interrupted silk sutures.
When it comes to IIFO-related gastrointestinal tract perforations, certain generalizations can be borrowed from the cumulative experience with non-intentional foreign object ingestions. In that setting, perforations of the stomach, duodenum, and large intestine tend to present with slow onset of non-specific clinical signs while perforations of the ileum and jejunum typically are severe and acute[22]. This is likely due to foregut and hindgut perforations occurring in retroperitoneal spaces where perforations are often contained. In contrast, midgut perforations are more likely to result in free spillage of enteric contents into the abdomen.
Recently published data reinforce the critical importance of prevention in the setting of IIFO, especially when repeated episodes of ingestion are present[2,5]. It has been difficult to prevent psychologically ill patients from ingesting foreign bodies and psychiatric medication has proven ineffective. Prisoners typically receive mental health care in their institution and do not require admission to the hospital for psychiatric care. Many of these patients are not suicidal and their psychiatric illness is not acute in nature, so psychiatric hospital admission is typically of little value[19]. Prevention strategies suggested include decreasing access to objects in the environment, increasing psychotherapy, changing diet for those with a history of food impaction, and dilating the esophagus for those with stricture[7].
The impetus for prevention primarily stems from the association between escalating psychiatric illness and repeated ingestion episodes. The fact that patients with recurrent ingestion episodes tend to have more severe psychiatric illness (as evident by the increasing number of formal psychiatric diagnoses) supports the contention that early and aggressive psychiatric intervention may help curtail the escalation of this self-damaging behavioral pattern. Gitlin et al[24] present a fascinating discussion of the psychiatric aspects of IIFO and found that most IIFO cases in the general population are associated with malingering, psychosis, pica, or personality disorders[24]. Treatment should be tailored to the patient’s specific psychiatric diagnosis[25]. Prisons may employ closely monitored units in combination with psychiatric care in an attempt to reduce this type of behavior.
Another impetus for aggressive prevention is that finding that the financial burden of IIFO also tends to escalate as this repetitive self-destructive behavior continues to recur[5]. As the complexity of care and frequency of surgical intervention increases in patients with a history of prior ingestions, so does the cost of care.
IIFO is a rare but complex and expensive disease in prisoners. Observation and endoscopy are common appropriate management strategies and surgery should be avoided when possible. For those patients who present with their first episode of IIFO, an intensive monitoring and prevention plan should be developed to reduce the risk of recurrent episodes. While more data on the types of prevention interventions and their effectiveness is needed, the pattern of escalation among the IIFO population certainly warrants organized, proactive approaches.
Our research on this topic was approved by the Institutional Review Board of The Ohio State University.
P- Reviewer: Alsolaiman M, Chai J, Gurkan A, Kim GH, Mazeh H, Pauli EM, Seow-Choen F S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | O’Sullivan ST, Reardon CM, McGreal GT, Hehir DJ, Kirwan WO, Brady MP. Deliberate ingestion of foreign bodies by institutionalised psychiatric hospital patients and prison inmates. Ir J Med Sci. 1996;165:294-296. |
| 2. | Dalal PP, Otey AJ, McGonagle EA, Whitmill ML, Levine EJ, McKimmie RL, Thomas AC, Cook CH, Papadimos TJ, Reilley TE. Intentional foreign object ingestions: need for endoscopy and surgery. J Surg Res. 2013;184:145-149. |
| 3. | Weiland ST, Schurr MJ. Conservative management of ingested foreign bodies. J Gastrointest Surg. 2002;6:496-500. |
| 4. | Barros JL, Caballero A, Rueda JC, Monturiol JM. Foreign body ingestion: management of 167 cases. World J Surg. 1991;15:783-788. |
| 5. | Otey JA, Houser JS, Jones C, Evans DC, Dalal PP, Whitmill ML, Levine EJ, McKimmie RL, Papadimos Steinberg SM, Bergese SD. Examination of financial charges associated with intentional foreign body ingestions by prisoners: A pattern of escalation. OPUS 12 Scientist. 2014;8: 6-8 Available from: http://journal.opus12.org/o12-ojs/ojs-2.1.1/index.php/o12sci/article/viewFile/286/123. |
| 6. | The Pew Charitable Trusts Managing Prison Health Care Spending. May 15, 2014. Available from: http://www.pewtrusts.org/en/research-and-analysis/reports/2014/05/15/managing-prison-health-care-spending. |
| 7. | Grimes IC, Spier BJ, Swize LR, Lindstrom MJ, Pfau PR. Predictors of recurrent ingestion of gastrointestinal foreign bodies. Can J Gastroenterol. 2013;27:e1-e4. |
| 8. | Selivanov V, Sheldon GF, Cello JP, Crass RA. Management of foreign body ingestion. Ann Surg. 1984;199:187-191. |
| 9. | Burton DM, Stith JA. Extraluminal esophageal coin erosion in children. Case report and review. Int J Pediatr Otorhinolaryngol. 1992;23:187-194. |
| 10. | Bennett DR, Baird CJ, Chan KM, Crookes PF, Bremner CG, Gottlieb MM, Naritoku WY. Zinc toxicity following massive coin ingestion. Am J Forensic Med Pathol. 1997;18:148-153. |
| 11. | Reilly J, Thompson J, MacArthur C, Pransky S, Beste D, Smith M, Gray S, Manning S, Walter M, Derkay C. Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope. 1997;107:17-20. |
| 12. | Ohio Department of Rehabilitation and Correction DRC Annual Reports. Accessed 8/6/2014 2006-2013. Available from: http://www.drc.ohio.gov/web/reports/reports2.asp. |
| 13. | Blaho KE, Merigian KS, Winbery SL, Park LJ, Cockrell M. Foreign body ingestions in the Emergency Department: case reports and review of treatment. J Emerg Med. 1998;16:21-26. |
| 14. | Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg. 1996;20:1001-1005. |
| 15. | Karp JG, Whitman L, Convit A. Intentional ingestion of foreign objects by male prison inmates. Hosp Community Psychiatry. 1991;42:533-535. |
| 16. | Karp JG, Whitman L, Convit A. Ingestion of sharp foreign objects. Am J Psychiatry. 1991;148:271-272. |
| 17. | Lee TH, Kang YW, Kim HJ, Kim SM, Im EH, Huh KC, Choi YW, Kim TH, Lee OJ, Jung UT. Foreign objects in Korean prisoners. Korean J Intern Med. 2007;22:275-278. |
| 18. | Bisharat M, O’Donnell ME, Gibson N, Mitchell M, Refsum SR, Carey PD, Spence RA, Lee J. Foreign body ingestion in prisoners - the Belfast experience. Ulster Med J. 2008;77:110-114. |
| 19. | Huang BL, Rich HG, Simundson SE, Dhingana MK, Harrington C, Moss SF. Intentional swallowing of foreign bodies is a recurrent and costly problem that rarely causes endoscopy complications. Clin Gastroenterol Hepatol. 2010;8:941-946. |
| 20. | Ribas Y, Ruiz-Luna D, Garrido M, Bargalló J, Campillo F. Ingested foreign bodies: do we need a specific approach when treating inmates? Am Surg. 2014;80:131-137. |
| 21. | Palese C, Al-Kawas FH. Repeat intentional foreign body ingestion: the importance of a multidisciplinary approach. Gastroenterol Hepatol (N Y). 2012;8:485-486. |
| 22. | Goh BK, Chow PK, Quah HM, Ong HS, Eu KW, Ooi LL, Wong WK. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg. 2006;30:372-377. |
| 23. | Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41:39-51. |
| 24. | Gitlin DF, Caplan JP, Rogers MP, Avni-Barron O, Braun I, Barsky AJ. Foreign-body ingestion in patients with personality disorders. Psychosomatics. 2007;48:162-166. |
| 25. | Klein CA. Intentional ingestion and insertion of foreign objects: a forensic perspective. J Am Acad Psychiatry Law. 2012;40:119-126. |