Published online Mar 16, 2019. doi: 10.4253/wjge.v11.i3.256
Peer-review started: February 10, 2019
First decision: February19, 2019
Revised: March 7, 2019
Accepted: March 11, 2019
Article in press: March 11, 2019
Published online: March 16, 2019
Endoscopically or fluoroscopically guided dilation is a safe and effective alternative to surgery for patients with benign strictures of the gastric outlet.
We describe two cases where a novel approach with a Spyglass® choledochoscope in assessing the extent of benign duodenal strictures and aiding in placement of duodenal stents for treatment of the strictures. Choledochoscope-guided wire and stent placement was successful in all cases, leading to symptom resolution related to benign duodenal obstruction. No major adverse events were observed.
Choledochoscope-guided assessment and endoscopic therapy is a viable approach in relieving duodenal obstruction, if the conventional combined fluoroscopic and endoscopic methods fail.
Core tip: The choledochoscope has the advantages of a smaller form factor, leading to easier passage of the scope through luminal narrowing or stricture with added benefits of direct visualization. Additional benefits include avoiding looping in the stomach with the passage of the choledochoscope through the therapeutic gastroscope. This study is the first to report this unique technique, with other potential applications in both benign and malignant strictures in the upper gastrointestinal tract if the conventional combined fluoroscopic and endoscopic methods fail.
- Citation: Cho RSE, Magulick J, Madden S, Burdick JS. Choledochoscope with stent placement for treatment of benign duodenal strictures: A case report. World J Gastrointest Endosc 2019; 11(3): 256-261
- URL: https://www.wjgnet.com/1948-5190/full/v11/i3/256.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i3.256
Malignancy remains the commonest cause of gastric outlet obstruction (GOO) but benign etiologies like peptic ulcer disease and caustic ingestion are responsible for significant proportion of such patients[1]. Nonsteroidal anti-inflammatory drugs (NSAID) ingestion is an uncommon cause of GOO[2]. The principal sites of involvement in cases of obstruction are the pyloric channel and the duodenal bulb. Small bowel strictures caused by NSAIDs are short (2-3 mm) web-like and are often labeled as diaphragms[3].
Endoscopically or fluoroscopically guided dilation is a safe and effective alternative to surgery for patients with benign strictures of the gastric outlet. It is considered to be a more rapid treatment and more cost effective than surgery[4-6]. The dilation therapy coupled with anti-secretory therapy and removal of the etiology factors (e.g., Helicobacter pylori) was shown to achieve long-term resolution of symptoms in 85%-100% of patient with peptic ulcer-related GOO[7]. However, the use of self-expandable metallic stents (SEMS) has been rarely reported in benign strictures[3,8,9].
The following cases highlights a novel approach in traversing duodenal strictures using a choledochoscope, combined with use of SEMS in benign duodenal strictures, in previously failed attempts with combined fluoroscopic and endoscopic guidance.
A 65 year-old man presented to the clinic with a complaint of post-prandial fullness and early satiety. The medical history of the patient was significant for peptic ulcer disease, osteoarthritis requiring NSAID, asthma, and depression. At physical exam, the abdomen was tender to palpation in the epigastric region. The vitals were normal. No pertinent laboratory or imaging was pertinent to this case.
A 77 year-old man presented to the clinic with a complaint of postprandial nausea and vomiting. The medical history of the patient was signficant for chronic knee pain requiring NSAID use, congestive heart failure, coronary artery disease, diabetes mellitus, and sleep apnea. At physical exam, the abdomen was tender to palpation in the epigastric region. The vitals were normal. No pertinent laboratory or imaging was available.
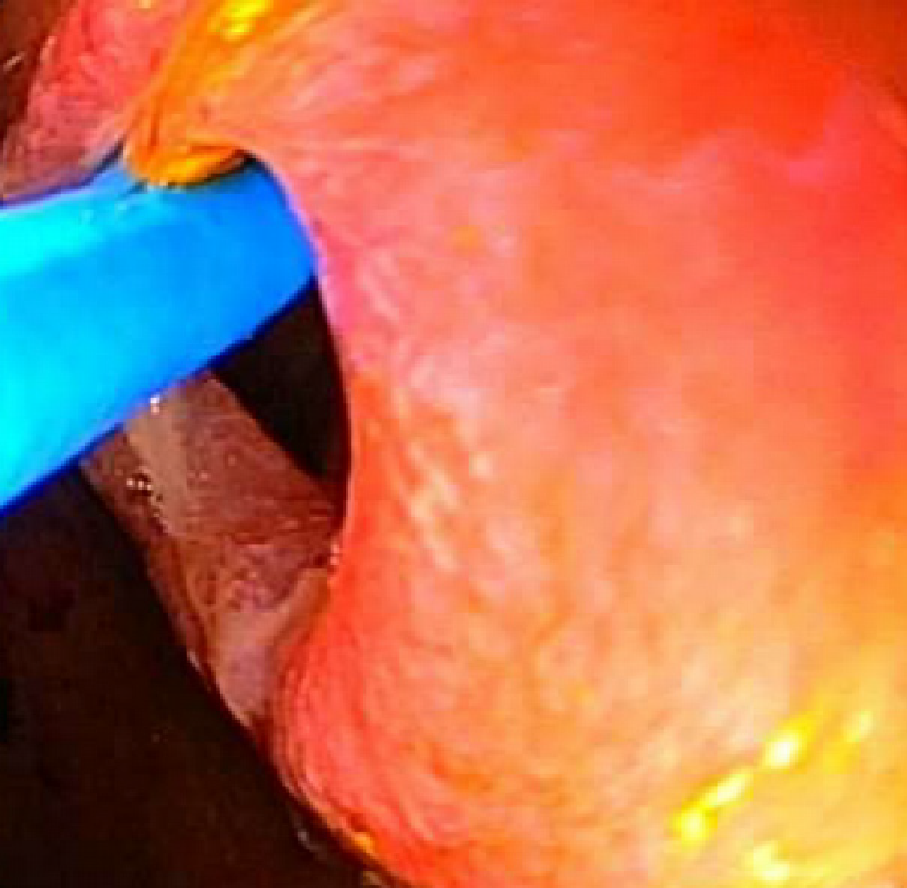
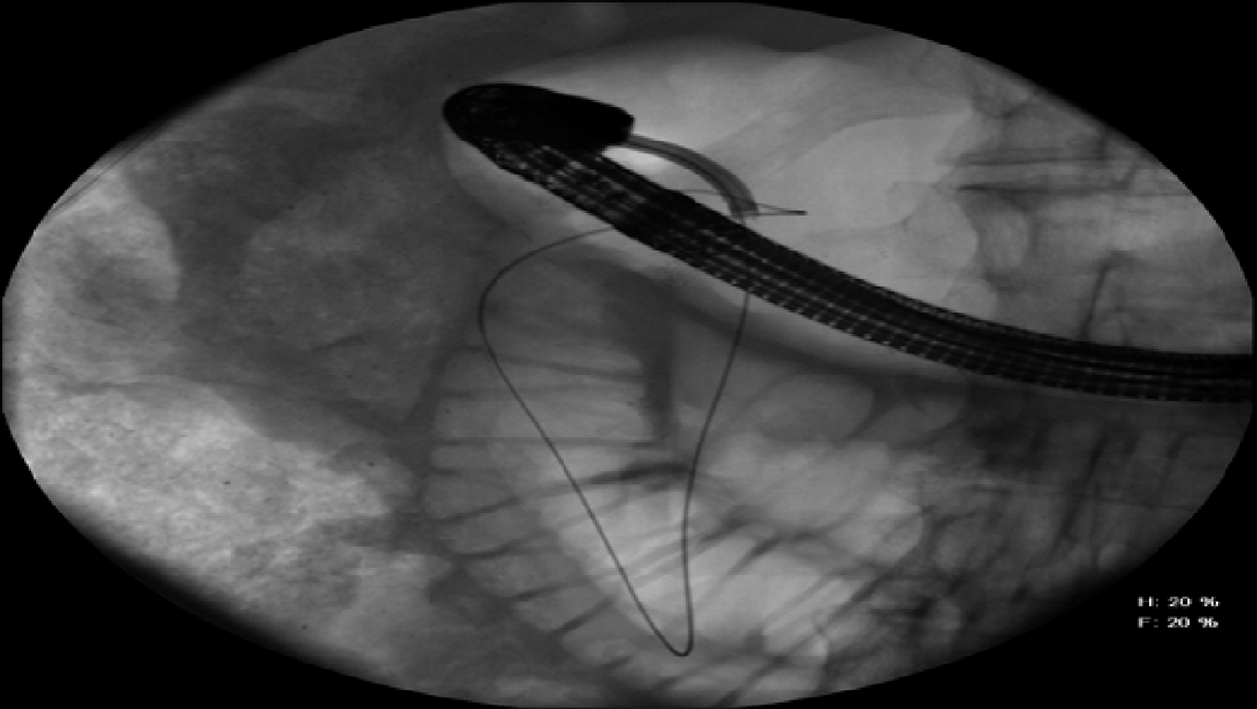
The initial esophagogastroduodenoscopy (EGD) revealed retained food in the stomach and a benign-appearing stricture at the pylorus, traversed post dilation. Another stricture involving was found in the distal bulb noted to be eccentric in location (Figure 1). The mucosa had no mucosal irregularity was smooth in appearance with cicatricle scarring and no intraluminal mass. The overall appearance was consistent with NSAID-induced stricture. No biopsies were performed. Multiple attempts at passing the balloon catheter and guidewire across the area were unsuccessful despite using fluoroscopic guidance (Figure 2).
The initial EGD revealed a two serial stricture around the C-sweep of the duodenum, which could not be traversed with a diagnostic gastroscope or ultrathin endoscope. The mucosa had no mucosal irregularity was smooth in appearance with cicatricle scarring and no intraluminal mass. The overall appearance was consistent with NSAID-induced stricture. No biopsies were performed. A guidewire was advanced across the first stricture but could not be advance pass the second stricture. Balloon dilation was attempted using a controlled radial expansion (CRE) balloon but given the short distance between the two strictures, the balloon was inadequately positioned across the stricture.
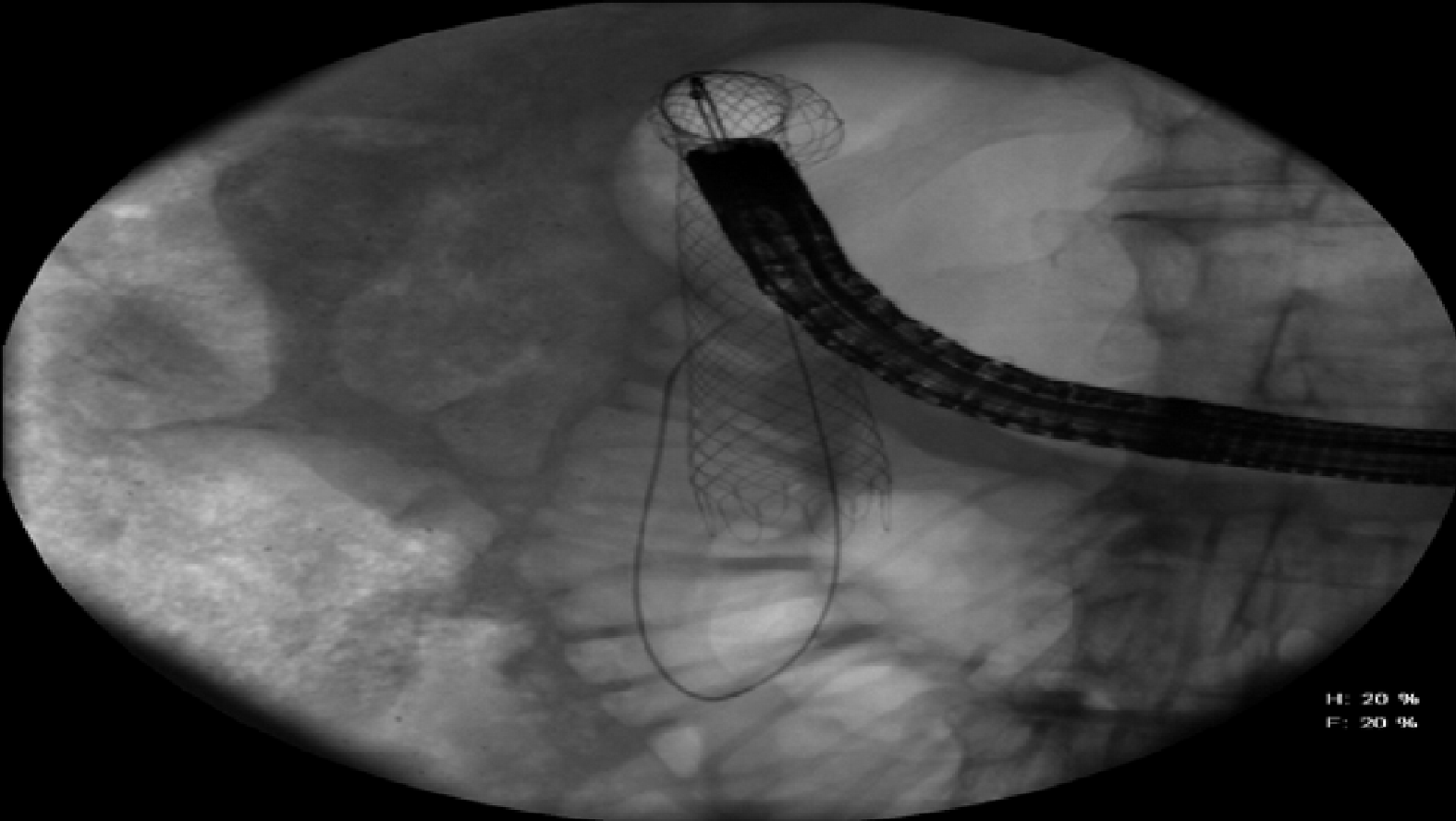
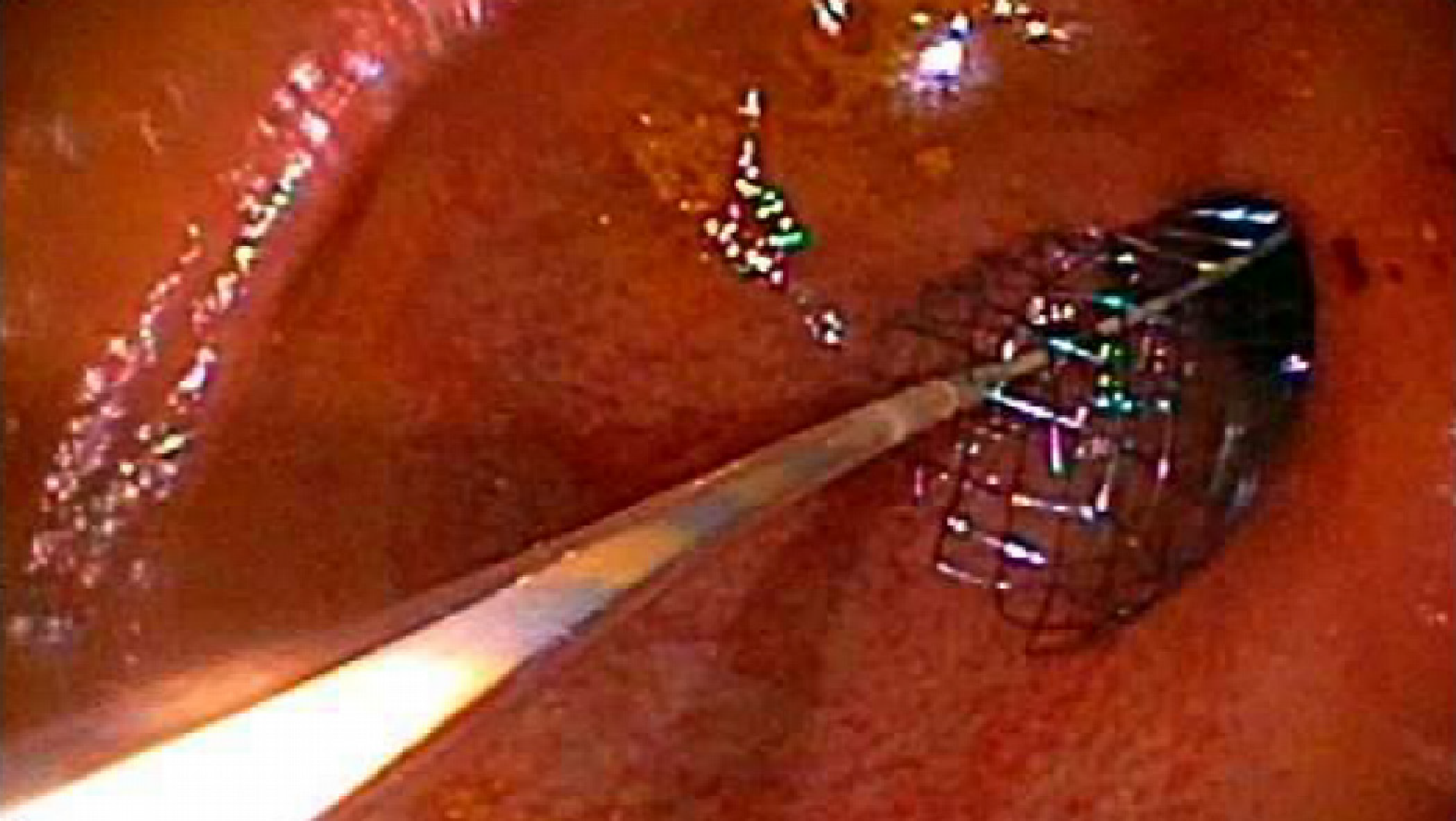
The repeat procedure was performed using a therapeutic gastroscope, allowing the passage of a Spyglass® choledochoscope (10 Fr outer diameter, 230 cm in length) with direct visualization of the lumen of the stricture (Figure 3 and 4). Then a guidewire was advanced through the choledochoscope (Figure 5), with subsequent stenting of the stricture (Figure 6 and 7) using an uncovered SEMS (WallFlex™ Duodenal Stent 22 mm by 90 mm), which was removed in 10 d. The stricture extension involvement was post bulbar which raised the issue of ampullary obstruction with covered stenting. Self-expanding stents utilized for the procedure were thus uncovered to avoid ampullary obstruction. Serial dilation was performed, using wire-guided CRE balloon over three sessions every 2 wk, with the final dilation performed to 20 mm.
The repeat procedure was performed using a therapeutic gastroscope, allowing the passage of a Spyglass® choledochoscope with direct visualization of the lumen of the two strictures. A guidewire was advanced through the choledochoscope, followed by dilation (12 mm) and subsequent stent placement (WallFlex™ Duodenal Stent 22 mm by 90 mm) crossing both strictures, which was removed in 10 d.
The patients were both appropriately counseled on avoidance of NSAID and continued to adhere to the recommendation throughout the treatment. Following the initial stent placement, both patients progressed from liquid to soft diet. They progressed to solid diet following the conclusion of the aforementioned procedures, without complications. Both patients progressed from liquid to soft diet without complications.
In this study we described a novel approach for traversing duodenal stricture using a choledochoscope. Both cases of duodenal strictures initially could not be traversed using the conventional combined fluoroscopic and endoscopic methods. Direct visualization of the stricture with a passage of the choledochoscope aided in traversing the narrowed lumen and subsequent intervention using a SEMS for the treatment of the duodenal obstruction.
Endoscopically or fluoroscopically guided dilation has proven to be an effective alternative to surgery for patients with benign duodenal strictures. The use of SEMS is an established palliative treatment to relieve the obstructive symptoms of inoperable gastrointestinal tract malignancy with stenotic change. The SEMS application in benign duodenal obstruction however has been rarely reported. All the previous studies have small sample size and it was concluded that stenting for benign duodenal obstruction is an effective treatment modality[8,9]. It is postulated that better symptom management could be obtained by gradual and continuous dilatation with SEMS in the stenotic segment. The results show that there are low rates of recurrences after stenting and it reduces the need for further invasive procedures. The most common complications of the stent placement included stent migration and stent ingrowth. Neither complications were seen in our cases.
The choledochoscope has the advantages of a smaller form factor, leading to easier passage of the scope through the stenosis with added benefits of direct visualization. Additional benefits include avoiding looping in the stomach (e.g., ultrathin gastroscope) with the passage of the scope through the therapeutic gastroscope. This study is the first to report this unique technique, with other potential applications in both benign and malignant strictures in the upper gastrointestinal tract if the conventional combined fluoroscopic and endoscopic methods fail.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sugimoto M S- Editor: Dou Y L- Editor: A E- Editor: Wu YXJ
| 1. | Shone DN, Nikoomanesh P, Smith-Meek MM, Bender JS. Malignancy is the most common cause of gastric outlet obstruction in the era of H2 blockers. Am J Gastroenterol. 1995;90:1769-1770. [PubMed] [Cited in This Article: ] |
| 2. | Weaver GA, Harper RL, Storey JA, Jenkins PL, Merrell NB. Nonsteroidal antiinflammatory drugs are associated with gastric outlet obstruction. J Clin Gastroenterol. 1995;20:196-198. [PubMed] [Cited in This Article: ] |
| 3. | Higuchi K, Umegaki E, Watanabe T, Yoda Y, Morita E, Murano M, Tokioka S, Arakawa T. Present status and strategy of NSAIDs-induced small bowel injury. J Gastroenterol. 2009;44:879-888. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 176] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 4. | Kim JH, Shin JH, Song HY. Benign strictures of the esophagus and gastric outlet: interventional management. Korean J Radiol. 2010;11:497-506. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Noor MT, Dixit P, Kochhar R, Nagi B, Dutta U, Singh K, Poornachandra KS. NSAIDs-Related Pyloroduodenal Obstruction and Its Endoscopic Management. Diagn Ther Endosc. 2011;2011:967957. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Kochhar R, Kochhar S. Endoscopic balloon dilation for benign gastric outlet obstruction in adults. World J Gastrointest Endosc. 2010;2:29-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 53] [Cited by in F6Publishing: 51] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 7. | Cherian PT, Cherian S, Singh P. Long-term follow-up of patients with gastric outlet obstruction related to peptic ulcer disease treated with endoscopic balloon dilatation and drug therapy. Gastrointest Endosc. 2007;66:491-497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Choi WJ, Park JJ, Park J, Lim EH, Joo MK, Yun JW, Noh H, Kim SH, Choi WS, Lee BJ, Kim JH, Yeon JE, Kim JS, Byun KS, Bak YT. Effects of the temporary placement of a self-expandable metallic stent in benign pyloric stenosis. Gut Liver. 2013;7:417-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Dormann AJ, Deppe H, Wigginghaus B. Self-expanding metallic stents for continuous dilatation of benign stenoses in gastrointestinal tract - first results of long-term follow-up in interim stent application in pyloric and colonic obstructions. Z Gastroenterol. 2001;39:957-960. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |