Published online Mar 16, 2019. doi: 10.4253/wjge.v11.i3.239
Peer-review started: August 17, 2018
First decision: August 31, 2018
Revised: January 28, 2019
Accepted: February 19, 2019
Article in press: February 20, 2019
Published online: March 16, 2019
The progression of Barrett’s esophagus (BE) to early esophageal carcinoma occurs sequentially; the metaplastic epithelium develops from a low-grade dysplasia to a high-grade dysplasia (HGD), resulting in early esophageal carcinoma and, eventually, invasive carcinoma. Endoscopic approaches including resection and ablation can be used in the treatment of this condition.
To compare the effectiveness of radiofrequency ablation (RFA) vs endoscopic mucosal resection (EMR) + RFA in the endoscopic treatment of HGD and intramucosal carcinoma.
In accordance with PRISMA guidelines, this systematic review included studies comparing the two endoscopic techniques (EMR + RFA and RFA alone) in the treatment of HGD and intramucosal carcinoma in patients with BE. Our analysis included studies involving adult patients of any age with BE with HGD or intramucosal carcinoma. The studies compared RFA and EMR + RFA methods were included regardless of randomization status.
The seven studies included in this review represent a total of 1950 patients, with 742 in the EMR + RFA group and 1208 in the RFA alone group. The use of EMR + RFA was significantly more effective in the treatment of HGD [RD 0.35 (0.15, 0.56)] than was the use of RFA alone. The evaluated complications (stenosis, bleeding, and thoracic pain) were not significantly different between the two groups.
Endoscopic resection in combination with RFA is a safe and effective method in the treatment of HGD and intramucosal carcinoma, with higher rates of remission and no significant differences in complication rates when compared to the use of RFA alone.
Core tip: This study is important for providing a framework for an endoscopic intervention that can prevent the progression of Barrett's esophagus (BE) into early esophageal carcinoma. This meta-analysis aims to compare two endoscopic techniques, namely, radiofrequency ablation by the HALO system (RFA) alone and RFA in combination with an endoscopic resection (EMR+RFA), in the treatment of high-grade dysplasia and intramucosal carcinoma in patients with BE. It also aims to evaluate the efficiency of each treatment and the prevalence of adverse events.
- Citation: de Matos MV, da Ponte-Neto AM, de Moura DTH, Maahs ED, Chaves DM, Baba ER, Ide E, Sallum R, Bernardo WM, de Moura EGH. Treatment of high-grade dysplasia and intramucosal carcinoma using radiofrequency ablation or endoscopic mucosal resection + radiofrequency ablation: Meta-analysis and systematic review. World J Gastrointest Endosc 2019; 11(3): 239-248
- URL: https://www.wjgnet.com/1948-5190/full/v11/i3/239.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i3.239
The progression of Barrett’s esophagus (BE) to early esophageal carcinoma occurs sequentially; the metaplastic epithelium develops from a low-grade dysplasia (LGD) to a high-grade dysplasia (HGD), resulting in early esophageal carcinoma and, eventually, invasive carcinoma[1,2]. According to several randomized studies, endoscopic interventions can prevent the progression of the disease[2,3].
Esophagectomy has been the treatment for BE that is associated with HGD or early esophageal carcinoma, and it has been recommended prior to endoscopic ablation; however, the procedure is associated with high rates of morbidity and mortality. In an attempt to avoid the complications associated with an esophagectomy, endoscopic therapies have been developed to treat early lesions[4].
BE may be treated endoscopically by using resection techniques (such as endoscopic mucosal resections and endoscopic submucosal resections) and ablative techniques (such as radiofrequency ablations, photodynamic therapies, and argonium plasma coagulations). The most common resection techniques use CAP (Olympus) and the Duette Kit (W. Cook). An endoscopic resection is considered to be a method with a high diagnostic accuracy and therapeutic efficacy[5], with the advantage that it also enables the histopathological study of the resected mucosa. Either localized or circumferential resections can be performed, though circumferential resections have greater morbidities.
Radiofrequency ablation, the most widely used technique in recent years, uses the HALO 360 system for circumferential ablations and the HALO 90 system for focal ablations (BARXX Medical, Sunnyvale, California). The first major study on RFA was conducted from 2003 to 2005 in eight centers in the USA by Sharma et al[6]. In this study, only patients with BE without dysplasia were included, and Sharma et al[6] reported a 70% success rate in eradicating intestinal metaplasia. Subsequent studies included patients with LGD, with remissions reported in 100% of the cases[6]. Later studies, which included patients with HGD and intramucosal carcinoma, also reported favorable success rates[7].
The combination of resection techniques with ablative techniques is now a form of treatment in cases where there are visible macroscopic lesions, since it is believed that these regions contain more advanced stages of the disease. The resection of the macroscopic lesions enables histopathological studies that more precisely define the degree of mucosal invasion.
The aim of this meta-analysis is to compare radiofrequency ablation (RFA) and endoscopic mucosal resection (EMR) + RFA in the treatment of HGD and intramucosal carcinoma in patients with BE; specifically, the meta-analysis compared the efficacy and the prevalence of adverse events in each treatment.
The current study was registered in PROSPERO (CRD42016049780) and was designed by using PRISMA guidelines[8]. Our analysis included studies involving adult patients of any age with BE and HGD or intramucosal carcinoma. These were comparative studies involving RFA using the Halo technique (BARXX Medical, Sunnyvale, California), either with or without the use of an endoscopic resection, in patients with BE. Studies were included regardless of randomization status. We included papers without language restrictions and that used full-text versions of the articles.
Electronic databases, such as MEDLINE, Scopus, and LILACS, were searched, along with a search of the gray literature. The following search strategies were used in MEDLINE: (1) (BARRETT ESOPHAGUS OR BARRETT’S ESOPHAGUS) AND (CATHETER ABLATION OR RADIOFREQUENCY) and (2) (esophagus neoplasm OR esophageal neoplasm OR esophagus cancer) AND (catheter ablation OR radiofrequency). In the other databases, the strategies used were (BARRETT ESOPHAGUS OR BARRETT’S ESOPHAGUS) AND (CATHETER ABLATION OR RADIOFREQUENCY).
Two independent reviewers selected the studies for the meta-analysis and, in cases of disagreement; the issues were addressed by utilizing a scientific methodology discussion group until a consensus was reached.
The arms of the study included a mucosal resection, followed by RFA (intervention), and RFA alone (control). The expected outcomes included the complete remission of the HGD and intramucosal carcinoma, as determined by endoscopic and histological evaluations. Complications, such as bleeding, perforations, thoracic pain, and stenosis resulting from the procedures, were also noted.
Since the included studies were observational studies, the NewcastleOttawa scale was used. This scale evaluates the quality of the studies by analyzing the following factors: selection of the exposed and unexposed cohorts, the exposure method, the demonstration that the outcome of interest was not present before the start of the study, the comparability between the cases vs the controls, the assessment of the outcome, the demonstration that the follow-up was long enough to evaluate the outcome, and the adequacy of the follow-up. Studies with a score of ≥ 6 were included[9]. Studies that presented losses of > 20% were excluded.
The RevMan5 software (Review Manager Version 5.3.5 - Cochrane Collaboration, Copyright © 2014) was used for the meta-analysis of the outcomes. Heterogeneity was modified by up to 50%, with an analysis of sensitivity where it was possible and necessary. In addition, the difference between the samples was calculated as the risk difference for the dichotomous variables with a Cochran–Mantel–Haenszel test, with a confidence interval of 95%.
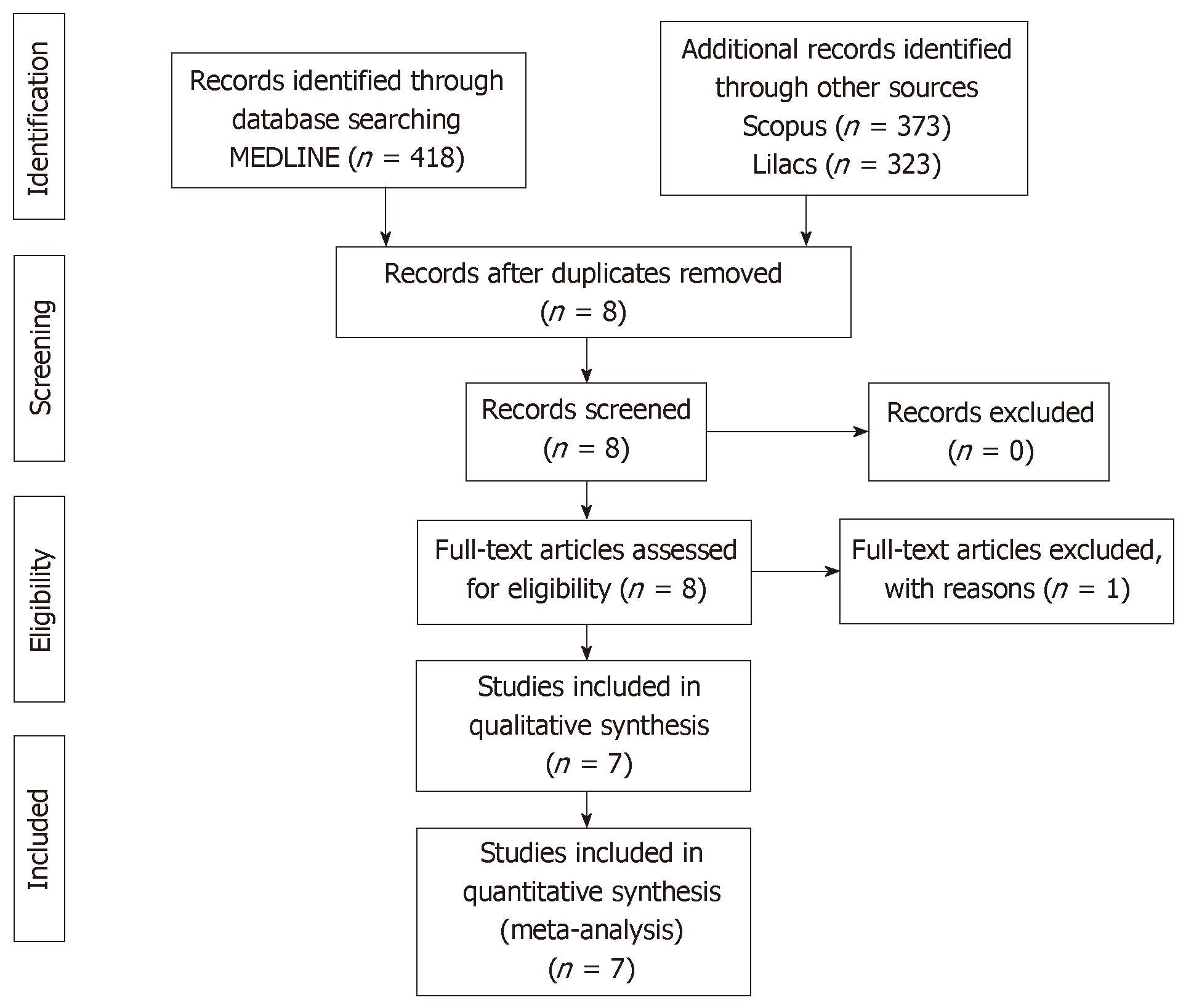
The search strategy used in the MEDLINE database led to the retrieval of 418 articles by using the first search technique and 368 by using the second technique. Another 373 articles were retrieved from the Scopus database, and 323 were retrieved from the LILACS database, but all of these articles were included in the MEDLINE search.
Initially, eight papers[10-17] were selected that compared RFA alone to RFA with an endoscopic resection for the treatment of HGD and intramucosal carcinoma, thus leading to an initial total of 2016 patients (Table 1). One study by Phoa et al[13] had to be excluded because the data could not be extracted for the meta-analysis. The seven papers that were included represented a total of 1950 patients, with 742 in the ablation with endoscopic resection group, and 1208 in the RFA alone group (Figure 1).
| Ref. | Country | Centers | Type of study | Subjects (EMR + RFA/RFA alone | Outcomes |
| Li et al[10], 2015 | USA | 148 | Observational retrospective | 1263 (406/857) | Efficacy and safety |
| Strauss et al[11], 2014 | USA | 2 | Observational retrospective | 36 (31/5) | Efficacy and safety |
| Haidry et al[12], 2013 | England | 19 | Observational retrospective | 335 (164/171) | Efficacy and safety |
| Kim et al[14], 2012 | USA | 1 | Observational retrospective | 169 (65/104) | Efficacy and safety |
| Caillol et al[15], 2012 | France | 1 | Observational retrospective | 34 (16/18) | Efficacy and safety |
| Okoro et al[16], 2012 | USA | 1 | Observational retrospective | 100 (44/46) | Efficacy and safety |
| Pouw et al[17], 2008 | The Netherlands | 1 | Observational retrospective | 44 (31/13) | Efficacy and safety |
Eradication: All seven selected studies evaluated the eradication of HGD and intramucosal carcinoma, and it was possible to submit all of the data for a meta-analysis, on the basis of the absolute numbers. Efficacy was evaluated at ≥ 12 months after the start of treatment. The follow-up times varied among the studies (9-32 mo), and there were differences in the follow-up times between the study arms in several studies.
According to the analysis, there was a significant difference between the two groups [RD 0.35(0.15, 0.56)], with better results observed in the patients who underwent endoscopic resections and RFA (EMR + RFA). The heterogeneity was high (I 2: 95%) and was not related to publication bias. The random model was used (Figure 2).
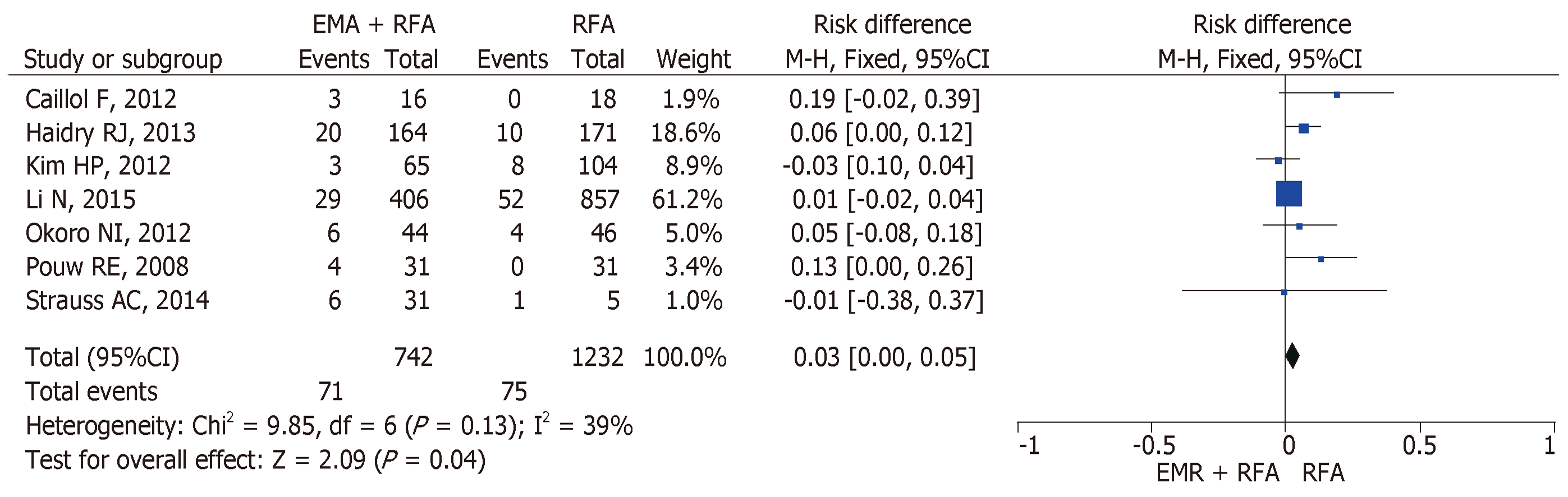
Stenosis: It was possible to analyze the data for all seven studies[10-17]. The cases of stenosis that occurred at any time during the treatment were included. According to the analyses, there was no significant difference between the two groups [RD 0.03 (0.00, 0.05)]. The heterogeneity was moderate (I 2: 39%) and was not related to publication bias. The fixed model was used (Figure 3).
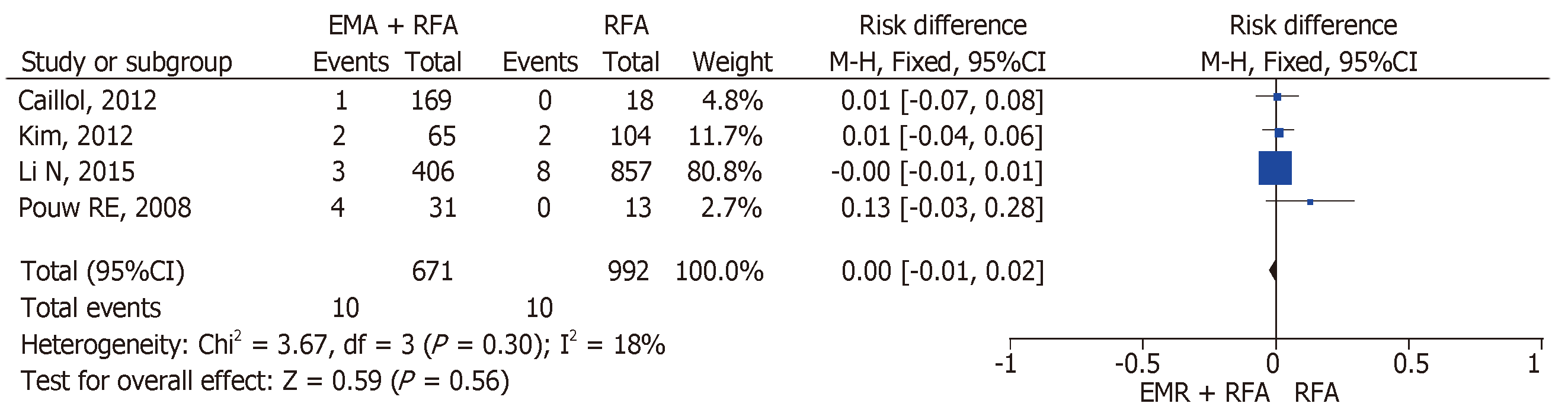
Bleeding: Only four studies provided information for the meta-analysis on bleeding: Li et al[10], Kim et al[14], Calloil et al[15], and Pouw et al[17]. According to the data, there was no significant difference between the two groups [SD 0.0 (−0.01, 0.02)], with low heterogeneity (I 2: 18%). The fixed model was used (Figure 4).
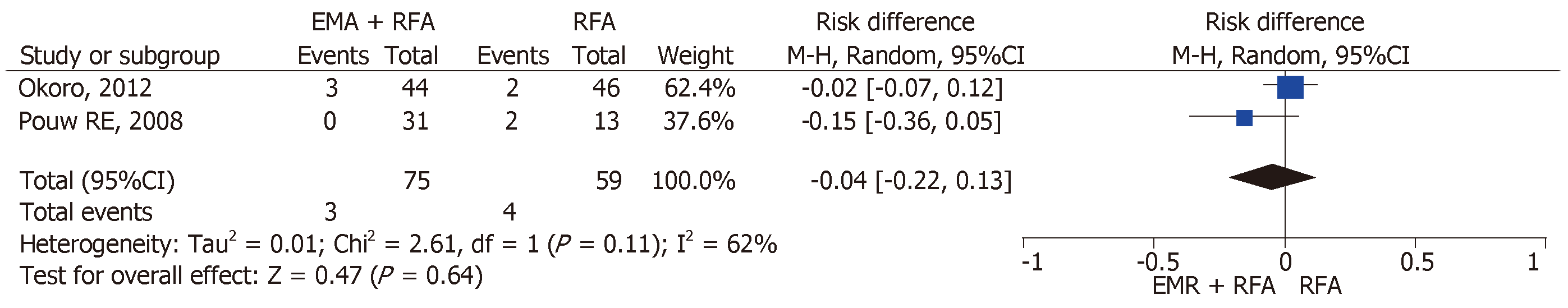
Thoracic pain: Only two studies provided data on the outcome of thoracic pain: Okoro et al[16] and Pouw et al[17]. According to the analysis, there was no significant difference between the two groups [SD -0.04 (-0.22, 0.13)]. The heterogeneity was high (I 2: 62%) and was not related to publication bias. The random model was used (Figure 5).
In all of the studies that were used in this meta-analysis, resections were performed if there were visible lesions or mucosal irregularities in the esophagogastric junction. In some cases, rescue EMRs were necessary during the follow-ups.
When regarding the eradication of HGD and intramucosal carcinoma, the use of resection with RFA was significantly more effective than RFA alone. In five cases, the combination of the techniques had an efficacy of > 90% (90%-100%)[10-12,15,17]. It was necessary to maintain high heterogeneity across the studies in the meta-analysis (95%) because many of the studies were lost to analysis when the sensitivity tests were performed.
Although the vast majority of the individual studies report that there is no difference between the groups of patients[11,12,15,16], some of the studies discuss the fact that the patients who were submitted to resection before ablation were more frequently diagnosed with intramucosal carcinoma than with HGD (66% vs 43%)[11], i.e., the patients were at a more advanced stage of the disease; therefore, they had a greater chance of incomplete resection or recurrence.
In 2016, Qumseya et al[18] published a systematic review comparing the complication rates of RFA and RFA associated with EMR. An overall complication rate of 8.8% was observed, with a 4.4% (P = 0.015) higher rate in the group that underwent RFA + EMR. The complications included: 5.6% who had strictures, 1% who had bleeding, and 0.6% who had perforations. These data are similar to those observed in the present study.
Another systematic review performed by Qumseya et al[19] in 2017, which included 2746 patients and evaluated the progression of LGD in patients with BE who underwent radiofrequency ablation and with surveillance only, showed a risk reduction of 10.9% in favor of the group submitted to RFA.
Regarding the eradication of metaplasia, the studies of Kim et al[14] and Caillol et al[15] demonstrated higher rates of incomplete treatment (remission of metaplasia) in patients who were submitted to ablation by radiofrequency alone. The rates of incomplete treatment ranged from 12% to 44% in the group submitted to resection, compared to 22% to 56% in the groups submitted to RFA alone. Although there was no significant difference between the two groups in relation to the incomplete remission of metaplasia (64% for both), Li et al[10] reported that 3.6% of patients who underwent RFA alone eventually progressed to having invasive adenocarcinoma, compared with 1.5% in the EMR + RFA group.
In relation to complications, four types of complications were reported in the studies: stenosis, bleeding, perforations, and thoracic pain. However, only three of these types could be analyzed because only one study cited numerical data on perforations[17], with one case occurring after the endoscopic resection. Other studies have reported that perforations did not occur in either of the two groups[10,12,16].
Our meta-analysis did not show any significant difference in the prevalence of stenosis, bleeding, or thoracic pain between the two groups. Only the study conducted by Kim et al[12] showed a higher number of stenosis cases in the RFA alone group, compared to the EMR + RFA group (7.7% vs 4.6%).
The strong points of this work are as follows: there are no systematic reviews comparing EMR + RFA vs RFA alone; although the studies used were observational studies, all of the studies had a score > 5 on the Newcastle-Ottawa Scale, i.e., good methodological quality; and the review had a large sample size, with 1971 patients in total (Table 2).
| Ref. | Selection | Comparability | Outcome | Points | |||||
| Representativeness of the exposed cohort | Selection of the unexposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at the start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow-up of cohort | ||
| Li et al[10], 2015 | × | × | × | × | × | × | × | 7 Points | |
| Strauss et al[11], 2014 | × | × | × | × | × | × | × | × | 8 Points |
| Haidry et al[12], 2013 | × | × | × | × | × | × | × | 7 Points | |
| Kim et al[14], 2012 | × | × | × | × | × | × | 6 Points | ||
| Caillol et al[15], 2012 | × | × | × | × | × | × | 6 Points | ||
| Okoro et al[16], 2012 | × | × | × | × | × | × | × | 7 Points | |
| Pouw et al[17], 2008 | × | × | × | × | ×× | × | × | 8 Points | |
In all of the studies included in this systematic review, the pathological samples were evaluated by at least two pathologists to confirm the presence of HGD and intramucosal carcinoma, with the exception of Li et al[10], wherein only one pathologist reviewed the samples.
One limitation of this systematic review is the heterogeneity of the techniques used to perform the endoscopic resections. The majority of the studies only cite the techniques without quantifying them, as shown in Table 3 There is also a lack of information about the techniques used to diagnose residual BE, which is also shown in Table 3.
| Ref. | Endoscopic resection method | Residual BE diagnosis method |
| Li et al[10], 2015 | Not mentioned | Not mentioned |
| Strauss et al[11], 2014 | Duette device | Not mentioned |
| Haidry et al[12], 2013 | Duette device | Not mentioned |
| Kim et al[14], 2012 | ER-cap technique (Olympus) (55%); Duette device (45%) | NBI assisted |
| Caillol et al[15], 2012 | Duette device or double channel technique | Staining with acetic acid or high definition endoscopy |
| Okoro et al[16], 2012 | ER-cap technique (Olympus) and Duette device* | Not mentioned |
| Pouw et al[17], 2008 | ER-cap technique (Olympus) and Duette device* | Lugol’s staining (2%) or narrow-band imaging1 |
The presence of buried glands after RFA is an obscure topic in the literature, likely due to the difficulty of diagnosing this condition. Sharma et al[6] evaluated 3007 neosquamous biopsies after RFA, and no buried glands were reported. In a systematic review conducted by Gray et al[20], buried metaplasia was found in 9 patients out of 1004 (0.9%). The other studies included in this systematic review did not report on the diagnosis of buried glands.
The weak points relate to the fact that few studies have compared the two groups and that the studies included nonconsecutive patients. There were no randomized studies that compared endoscopic resections and RFA with RFA alone because the patients who presented visible changes during endoscopies (nodularities or other lesions) were submitted for resections and could not be treated exclusively by ablative methods. Moreover, only three studies presented optimal follow-up periods (> 24 mo) to evaluate the eradication of the disease.
In conclusion, endoscopic resection, in combination with RFA, is a safe and effective method in the treatment of HGD and intramucosal carcinoma, with higher rates of remission and no significant difference in complication rates when compared to RFA alone.
Barrett’s esophagus (BE) remains a challenging disease. BE associated with dysplasia is a difficult diagnosis for pathologists. Additionally, the adequate treatment and close follow-up of these patients is required. With the advent of new therapies, more studies have been done to unveil the best way to treat patients with this disease. One of the most promising techniques in the management of this condition is radiofrequency ablation (RFA). This approach can also be performed combined with resection methods, such as endoscopic mucosal resection (EMR). This systematic review and meta-analysis aimed to evaluate RFA alone or combined EMR (RFA + EMR) in the treatment of high-grade dysplasia (HGD) and intramucosal carcinoma in BE.
Radiofrequency ablation has been recognized with the method of choice for the treatment of BE with dysplasia. However, there is a question in the literature about the need to associate resection techniques such as EMR and endoscopic submucosal dissection in the treatment of these patients. Our study aims to assess whether the association of EMR adds benefit in the treatment of BE with HGD and intramucosal carcinoma.
The objective of our study is to evaluate the effectiveness of RFA and RFA+EMR in patients with BE with HGD and intramucosal carcinoma. This systematic review and meta-analysis can help colleagues in decision making regarding the treatment of this condition, as well as serve as a basis for future studies related to this subject.
This systematic review was conducted according to the PRISMA. The search was performed in electronic databases including Medline (via PubMed), LILACS and Cochrane. Studies comparing RFA and EMR + RFA in the treatment of HGD and intramural carcinoma were included. The Newcastle-Ottawa tool was used to evaluate the risk of bias and the applicability of primary diagnostic accuracy studies. The meta-analysis was performed using the RevMan5 software.
Seven studies were included with a total of 1950 patients, with 742 in the RFA + EMR group, and 1208 in the RFA isolate group. A higher eradication rate was observed in patients submitted to RFA + EMR compared to patients submitted to RFA isolated [RD 0.35 (0.15, 0.56)]. However, no statistical differences were observed regard to the bleeding rate, [SD 0.0 (-0.01, 0.02)], stenosis rate [RD 0.03 (0.00, 0.05)], and chest pain rate [SD -0.04 (-0.22, 0.13)].
This meta-analysis corroborates the idea of performing EMR+RFA in patients with BE with HGD or intramucosal carcinoma, without increasing the number of complications associated with the combination of RFA + EMR when compared to RFA alone. We believe that the association of these techniques allows a deeper elimination of BE with HGD or intramucosal carcinoma, without increasing the risk of the procedure for the patient, validating the association of these techniques in the treatment of this disease.
This systematic review and meta-analysis can help colleagues in decision making regarding the treatment of HGD or intramucosal carcinoma in BE, as well as serve as a basis for future studies related to this subject.
PRISMA 2009 Checklist: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Unsolicited Manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen YX, Jha AK, Friedel D S- Editor: Dou Y L- Editor: A E- Editor: Wu YXJ
| 1. | Phillips WA, Lord RV, Nancarrow DJ, Watson DI, Whiteman DC. Barrett's esophagus. J Gastroenterol Hepatol. 2011;26:639-648. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Lenglinger J, Riegler M, Cosentini E, Asari R, Mesteri I, Wrba F, Schoppmann SF. Review on the annual cancer risk of Barrett's esophagus in persons with symptoms of gastroesophageal reflux disease. Anticancer Res. 2012;32:5465-5473. [PubMed] [Cited in This Article: ] |
| 3. | Phoa KN, van Vilsteren FG, Weusten BL, Bisschops R, Schoon EJ, Ragunath K, Fullarton G, Di Pietro M, Ravi N, Visser M, Offerhaus GJ, Seldenrijk CA, Meijer SL, ten Kate FJ, Tijssen JG, Bergman JJ. Radiofrequency ablation vs endoscopic surveillance for patients with Barrett esophagus and low-grade dysplasia: a randomized clinical trial. JAMA. 2014;311:1209-1217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 445] [Cited by in F6Publishing: 407] [Article Influence: 40.7] [Reference Citation Analysis (0)] |
| 4. | Chadwick G, Groene O, Markar SR, Hoare J, Cromwell D, Hanna GB. Systematic review comparing radiofrequency ablation and complete endoscopic resection in treating dysplastic Barrett's esophagus: a critical assessment of histologic outcomes and adverse events. Gastrointest Endosc. 2014;79:718-731.e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Terheggen G, Horn EM, Vieth M, Gabbert H, Enderle M, Neugebauer A, Schumacher B, Neuhaus H. A randomised trial of endoscopic submucosal dissection versus endoscopic mucosal resection for early Barrett's neoplasia. Gut. 2017;66:783-793. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 137] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 6. | Sharma VK, Wang KK, Overholt BF, Lightdale CJ, Fennerty MB, Dean PJ, Pleskow DK, Chuttani R, Reymunde A, Santiago N, Chang KJ, Kimmey MB, Fleischer DE. Balloon-based, circumferential, endoscopic radiofrequency ablation of Barrett's esophagus: 1-year follow-up of 100 patients. Gastrointest Endosc. 2007;65:185-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 219] [Cited by in F6Publishing: 233] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 7. | Sharma VK, Kim HJ, Das A, Dean P, DePetris G, Fleischer DE. A prospective pilot trial of ablation of Barrett's esophagus with low-grade dysplasia using stepwise circumferential and focal ablation (HALO system). Endoscopy. 2008;40:380-387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6253] [Cited by in F6Publishing: 7039] [Article Influence: 469.3] [Reference Citation Analysis (0)] |
| 9. | Wells GA, Shea B, O’connell D, Peterson JE, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Cited in This Article: ] |
| 10. | Li N, Pasricha S, Bulsiewicz WJ, Pruitt RE, Komanduri S, Wolfsen HC, Chmielewski GW, Corbett FS, Chang KJ, Shaheen NJ. Effects of preceding endoscopic mucosal resection on the efficacy and safety of radiofrequency ablation for treatment of Barrett's esophagus: results from the United States Radiofrequency Ablation Registry. Dis Esophagus. 2016;29:537-543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Strauss AC, Agoston AT, Dulai PS, Srivastava A, Rothstein RI. Radiofrequency ablation for Barrett's-associated intramucosal carcinoma: a multi-center follow-up study. Surg Endosc. 2014;28:3366-3372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Haidry RJ, Dunn JM, Butt MA, Burnell MG, Gupta A, Green S, Miah H, Smart HL, Bhandari P, Smith LA, Willert R, Fullarton G, Morris J, Di Pietro M, Gordon C, Penman I, Barr H, Patel P, Boger P, Kapoor N, Mahon B, Hoare J, Narayanasamy R, O'Toole D, Cheong E, Direkze NC, Ang Y, Novelli M, Banks MR, Lovat LB. Radiofrequency ablation and endoscopic mucosal resection for dysplastic barrett's esophagus and early esophageal adenocarcinoma: outcomes of the UK National Halo RFA Registry. Gastroenterology. 2013;145:87-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 160] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 13. | Phoa KN, Pouw RE, van Vilsteren FGI, Sondermeijer CMT, Ten Kate FJW, Visser M, Meijer SL, van Berge Henegouwen MI, Weusten BLAM, Schoon EJ, Mallant-Hent RC, Bergman JJGHM. Remission of Barrett's esophagus with early neoplasia 5 years after radiofrequency ablation with endoscopic resection: a Netherlands cohort study. Gastroenterology. 2013;145:96-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 171] [Cited by in F6Publishing: 183] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 14. | Kim HP, Bulsiewicz WJ, Cotton CC, Dellon ES, Spacek MB, Chen X, Madanick RD, Pasricha S, Shaheen NJ. Focal endoscopic mucosal resection before radiofrequency ablation is equally effective and safe compared with radiofrequency ablation alone for the eradication of Barrett's esophagus with advanced neoplasia. Gastrointest Endosc. 2012;76:733-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Caillol F, Bories E, Pesenti C, Poizat F, Monges G, Guiramand J, Esterni B, Giovannini M. Radiofrequency ablation associated to mucosal resection in the oesophagus: experience in a single centre. Clin Res Hepatol Gastroenterol. 2012;36:371-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Okoro NI, Tomizawa Y, Dunagan KT, Lutzke LS, Wang KK, Prasad GA. Safety of prior endoscopic mucosal resection in patients receiving radiofrequency ablation of Barrett's esophagus. Clin Gastroenterol Hepatol. 2012;10:150-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 17. | Pouw RE, Gondrie JJ, Sondermeijer CM, ten Kate FJ, van Gulik TM, Krishnadath KK, Fockens P, Weusten BL, Bergman JJ. Eradication of Barrett esophagus with early neoplasia by radiofrequency ablation, with or without endoscopic resection. J Gastrointest Surg. 2008;12:1627-36; discussion 1636-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 91] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 18. | Qumseya BJ, Wani S, Desai M, Qumseya A, Bain P, Sharma P, Wolfsen H. Adverse Events After Radiofrequency Ablation in Patients With Barrett's Esophagus: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2016;14:1086-1095.e6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 106] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 19. | Qumseya BJ, Wani S, Gendy S, Harnke B, Bergman JJ, Wolfsen H. Disease Progression in Barrett's Low-Grade Dysplasia With Radiofrequency Ablation Compared With Surveillance: Systematic Review and Meta-Analysis. Am J Gastroenterol. 2017;112:849-865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 20. | Gray NA, Odze RD, Spechler SJ. Buried metaplasia after endoscopic ablation of Barrett's esophagus: a systematic review. Am J Gastroenterol. 2011;106:1899-908; quiz 1909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 124] [Article Influence: 9.5] [Reference Citation Analysis (0)] |