Published online Dec 28, 2020. doi: 10.13105/wjma.v8.i6.472
Peer-review started: October 23, 2020
First decision: November 20, 2020
Revised: November 29, 2020
Accepted: December 10, 2020
Article in press: December 10, 2020
Published online: December 28, 2020
Gastrectomy is the optimal treatment for gastric cancer. Laparoscopic-assisted gastrectomy (LAG) has been extensively employed, while hand-assisted laparoscopic gastrectomy (HALG), which is similar to LAG, remains controversial. Although HALG is popular in China, some surgeons do not accept it as a minimal-access technique.
To assess the safety and practicability of HALG by comparing the short-term outcomes of HALG and LAG.
The electronic databases of EMBASE, PubMed, China National Knowledge Infrastructure, and Cochrane Library were thoroughly searched, and randomized controlled trials (RCTs) comparing HALG and LAG were included. The study results, including surgery time, blood loss, retrieved lymphatic nodes, incision length, time to first flatus, hospitalization duration, and all postsurgical complications, were compared between the two groups.
Five RCTs, which included 302 cases with HALG and 298 cases with LAG, were considered eligible for inclusion. Meta-analysis showed that HALG significantly reduced surgery time (P < 0.01), hospital duration (P < 0.01), and overall postsurgical complications (P < 0.01). Additionally, HALG significantly increased the number of retrieved lymphatic nodes (P = 0.01) and incision length (P < 0.01) compared with LAG. The blood loss and time to first flatus were similar between the two groups (P > 0.05).
Compared with LAG, HALG is a simpler and safer technique. Additionally, HALG should be used as a minimal-access technique, especially in technologically undeveloped areas.
Core Tip: No consensus is available in the literature about which technique is more beneficial to the patients between hand-assisted laparoscopic gastrectomy (HALG) and laparoscopic-assisted gastrectomy (LAG). This is the first systematic review and meta-analysis comparing HALG and LAG. We compared these two techniques in terms of estimated surgery time, blood loss, retrieved lymphatic nodes, incision length, time to first flatus, hospitalization duration, and all postsurgical complications from selected randomized controlled trials. Compared with LAG, HALG is a simpler and safer technique.
- Citation: Gan W, Chen ZY, Liu L, Chen GB, Zhou J, Song YN, Cao YK. Comparison of hand-assisted laparoscopic radical gastrectomy and laparoscopic-assisted radical gastrectomy: A systematic review and meta-analysis. World J Meta-Anal 2020; 8(6): 472-481
- URL: https://www.wjgnet.com/2308-3840/full/v8/i6/472.htm
- DOI: https://dx.doi.org/10.13105/wjma.v8.i6.472
Gastric cancer is associated with high mortality and morbidity rates in China[1-3]. Gastrectomy is the optimal treatment for gastric cancer, but the surgical approach has numerous choices such as traditional open gastrectomy, laparoscopic-assisted gastrectomy (LAG), totally laparoscopic gastrectomy, robot-assisted gastrectomy, and hand-assisted laparoscopic gastrectomy (HALG). Hunter predicted an exciting prospect for hand-assisted laparoscopic surgery (HALS) in gastrectomy[4]. HALS combines the advantages of laparoscopic surgery and laparotomy; thus, it is popular in China[5,6].
Compared with laparoscopic-assisted or totally laparoscopic surgery, HALS retains the tactile sensation of the surgeon’s hand, which can make the operation faster and safer. Besides, it also has advantages of laparoscopy, such as being minimally invasive and having a zooming surgical field. For young surgeons, it also has the advantage of having a short-learning curve[7]. To date, HALG has formed the unique surgical approach called three-step HALG[8-10], which makes gastrectomy more convenient and simpler.
Recently, the number of studies on HALG is increasing. Although certain studies have compared HALG and LAG[11,12], controversy about its useful meaning still exists. Therefore, the present study conducted a systematic review and meta-analysis, with an aim to evaluate the safety and practicability of HALG, and compare the short-term outcomes of HALG and LAG.
EMBASE, PubMed, Cochrane Library, and China National Knowledge Infrastructure were searched for primary studies published up to August 2019. The search terms ‘hand-assisted laparoscopic’ and ‘gastrectomy’ and ‘gastric cancer’ were used in English and Chinese. Additionally, the references cited in retrieved articles were reviewed in order to select studies that better suit our criteria. Studies with only abstracts or unpublished reports were not included.
Two authors (Gan W and Liu LY) independently reviewed the search results. Any studies that met the following criteria were considered: (1) All patients were diagnosed with gastric cancer; (2) The study compared HALG and LAG; (3) It was a randomized controlled trial (RCT); and (4) The endpoints included postsurgical complications. If there were two or more articles by the same authors or research institutions, the one with larger sample size was selected.
To limit heterogeneity across the studies, the following exclusion criteria were used: (1) The study included totally laparoscopic or robotic radical gastrectomy; (2) It did not provide sufficient data to calculate the risk ratio (RR) ant its 95% confidence interval (CI) of different procedures for overall postsurgical complications; and (3) The article was an abstract presented at meetings, a case series, a cohort study, a review, or a letter.
Data were extracted independently by two authors, and discrepancies were resolved by consensus. The following details were extracted: Name of the first author, institution, country, study period, publication year, sample size, mean age, gender, tumor stage, surgery time, blood loss, retrieved lymphatic nodes, incision length, time to first flatus, hospitalization duration, and all postsurgical complications.
All statistical analyses were performed using RevMan 5.3 software (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). For the meta-analysis, the results were presented as RR for dichotomous variables and weighted mean difference (WMD) for continuous variables. If the I2 value was ≤ 50%, a fixed effects model was employed, and if the value was > 50%, a random effects model was selected. Two-sided P < 0.05 was considered to indicate a statistically significant difference. χ2 test was used to evaluate statistical heterogeneity, and I2 statistic was calculated to evaluate the extent of variability attributable to statistical heterogeneity between trials. To assess the publication bias, a funnel plot was applied.
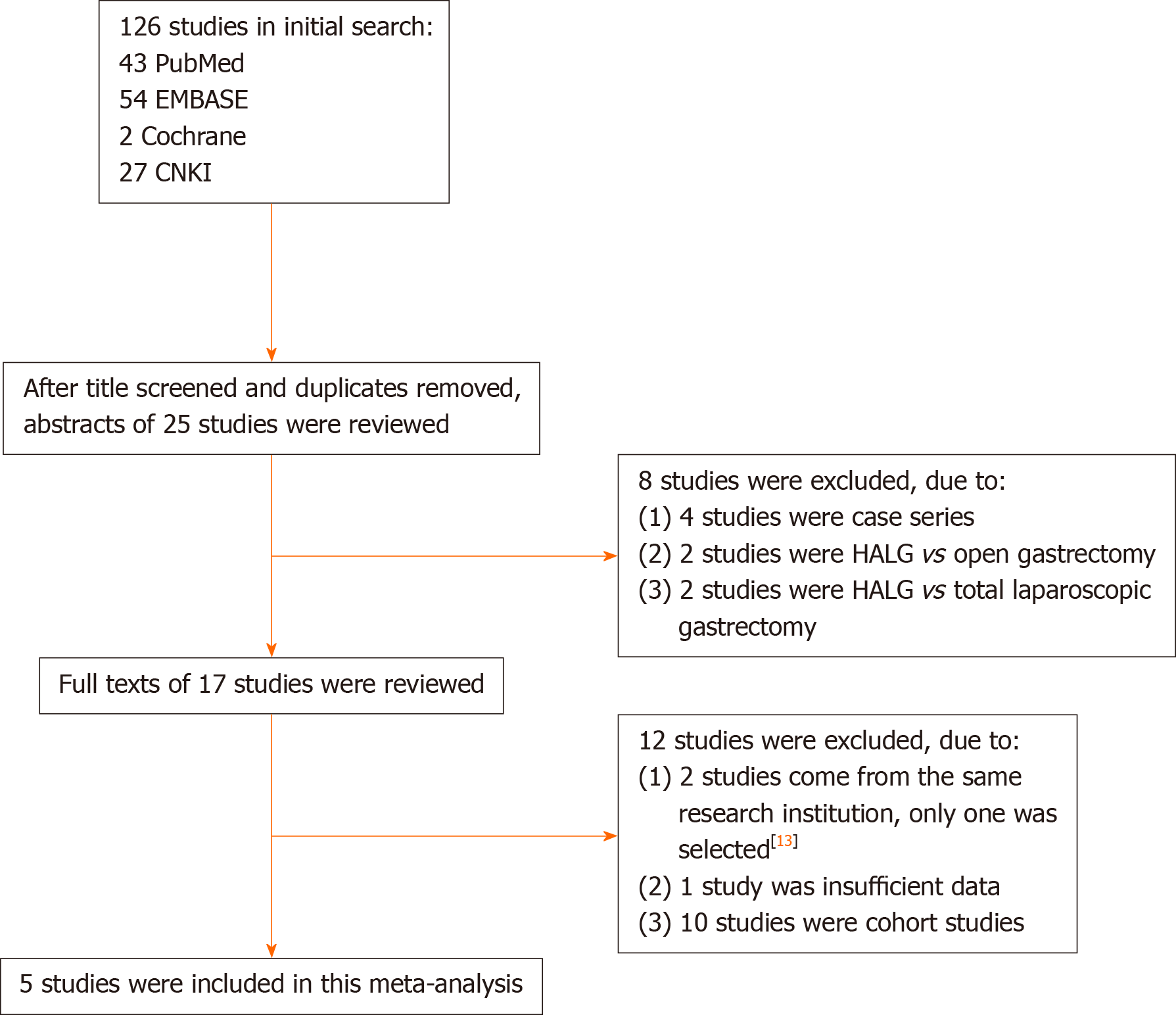
During the initial search, 126 publications were obtained from electronic databases. A total of 17 articles were reviewed in detail. Two studies derived from the same research institution[13,14]; thus, the biggest sample size study was selected[13]. Finally, five RCT studies were selected for the meta-analysis[13,15-18]. The details of the search strategy are shown in Figure 1.
The basic characteristics of the included studies are shown in Table 1. Five RCTs were included. A total of 302 patients were included in the HALG group, and 298 patients were included in the LAG group. Five studies were reported from different regions of China.
| Ref. | Year | Nation | Geographical region | Study period | Sample size | Age, mean (yr) | Gender (M/F) | Tumor stage | Types of operation | |||||||||
| HALG | LAG | HALG | LAG | HALG | LAG | HALG | LAG | HALG | LAG | |||||||||
| I/II/III/IV | I/II/III/IV | TG | DG | PG | TG | DG | PG | |||||||||||
| Gong et al[13] | 2014 | China | Southwest | 2008-2013 | 120 | 113 | 58.94 | 59.29 | 75/45 | 82/31 | 15/19/46/40 | 9/15/52/37 | 46 | 61 | 13 | 31 | 59 | 23 |
| Wang[16] | 2015 | China | North | 2010-2013 | 61 | 65 | NA | NA | NA | NA | NA | NA | 0 | 61 | 0 | 0 | 60 | 0 |
| Yang et al[18] | 2016 | China | Southwest | 2013-2015 | 42 | 42 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Xue et al[17] | 2018 | China | Central | 2015-2016 | 28 | 28 | 52.68 | 52.74 | 21/7 | 20/8 | 3/7/18/0 | 2/5/21/0 | 0 | 28 | 0 | 0 | 28 | 0 |
| Gao et al[15] | 2019 | China | East | 2013-2014 | 51 | 50 | 57.6 | 58.2 | 32/19 | 36/14 | 10/12/29/0 | 13/15/22/0 | 12 | 39 | 0 | 17 | 33 | 0 |
The Jadad scoring system was used to assess the quality of the selected RCT studies. Due to being open-label RCTs, those studies only scored 2 or 3 points (Table 2). It was known that operation was impossible to blind patients and surgeons. Thus, studies with a score ≥ 2 were classified as methodologically sound studies.
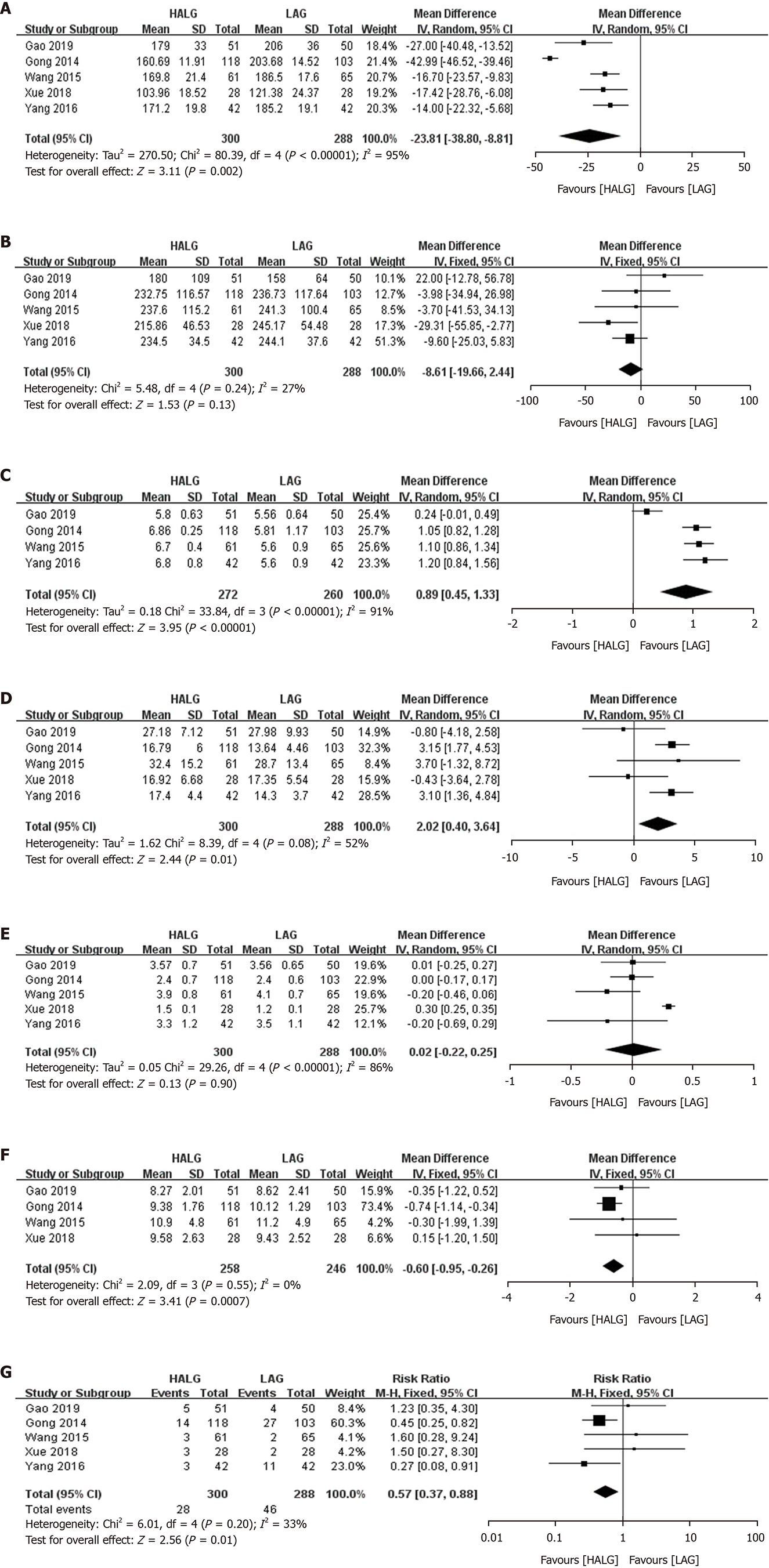
The surgery time, blood loss, incision length, and retrieved lymphatic nodes were evaluated. The HALG group had a shorter surgery time compared with the LAG group (WMD, -23.81 min; 95%CI, -38.80 to -8.81; P = 0.002; Figure 2A). There was no significant difference in blood loss between the two groups (WMD, -8.61 mL; 95%CI, -19.66 to 2.44; P = 0.13; Figure 2B). Only four studies reported the incision length, and the value was longer in the HALG group than in the LAG group (WMD, 0.89 cm; 95%CI, 0.45 to 1.33; P < 0.01; Figure 2C). The HALG group had a greater number of retrieved lymphatic nodes compared with the LAG group (WMD, 2.02; 95%CI, 0.40 to 3.64; P = 0.01; Figure 2D).
The time to first flatus and the duration of postsurgical hospitalization were evaluated in the postoperative recovery. There was no significant difference in the time to first flatus between the two groups (WMD, 0.02 d; 95%CI, -0.22 to 0.25; P = 0.90; Figure 2E). The HALG group had shorter hospital duration, compared with the LAG group (WMD, -0.60 d; 95%CI, -0.95 to -0.26; P < 0.01; Figure 2F).
The overall postsurgical complications were evaluated in all the included studies. The pooled result showed that the HALG group had a lower risk of overall postsurgical complications than the LAG group (RR, 0.57; 95%CI, 0.37 to 0.88; P < 0.01; Figure 2G).
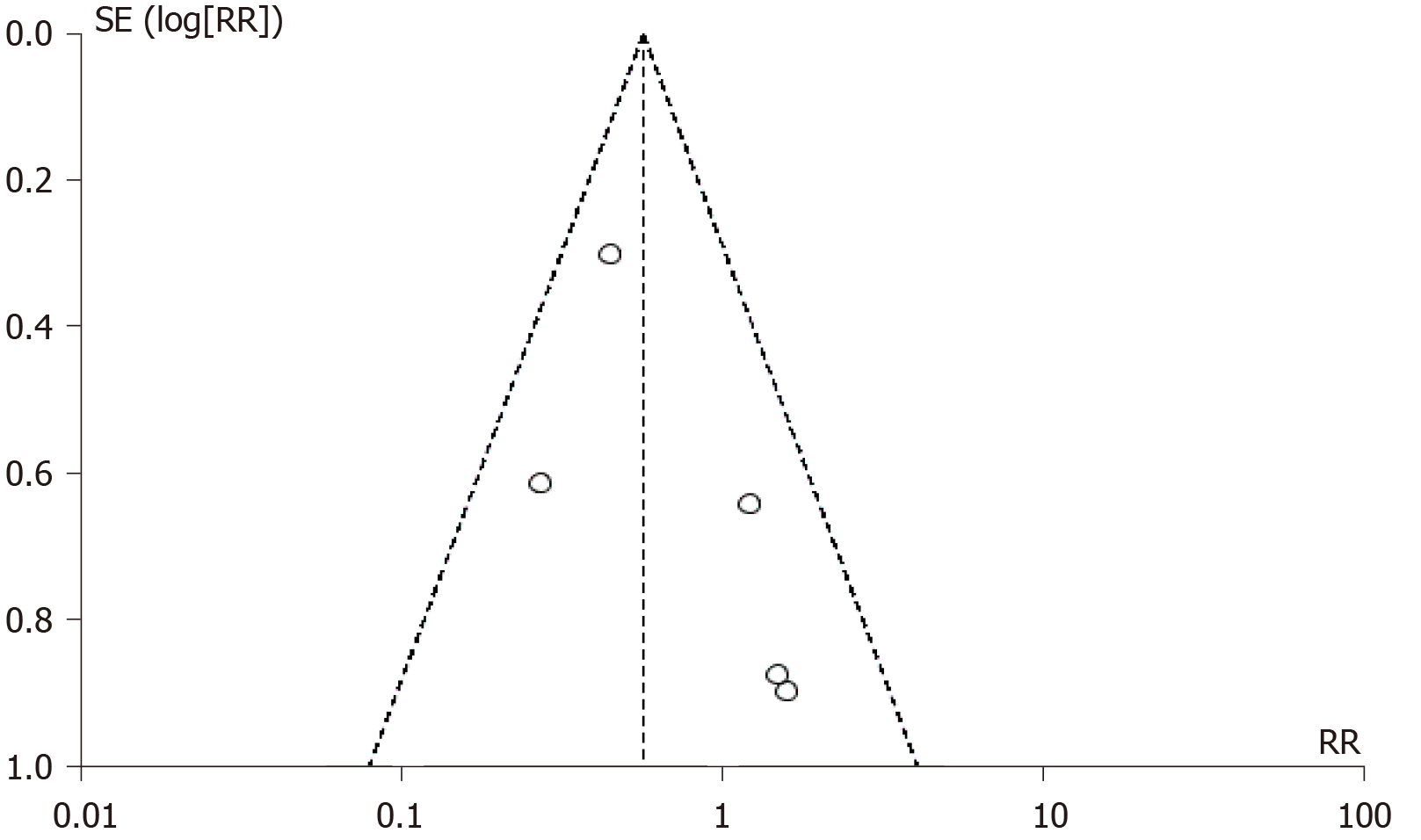
The funnel plot of overall postsurgical complications was used to examine the potential publication bias. Based on the approximate symmetry, there was no evidence of publication bias in this meta-analysis (Figure 3).
The therapeutic effect of LAG has been confirmed for gastric cancer in previous studies[19-21]. Likewise, several studies confirmed the therapeutic effect of HALS on gastrointestinal tumors[22-24]. There are numerous similarities between HALG and LAG, such as the use of laparoscopy, a small incision, and digestive reconstruction. However, they also differ in various aspects such as the surgical procedure and the function of incision. ‘Three-step HALG’ has become the standardized procedure in our hospital[8,25]. The application of HALG has been gradually increasing, especially in China. Nevertheless, due to the lack of consistency across different studies, controversy exists on the therapeutic effects and advantages of HALG. In this meta-analysis, in order to improve the reliability, we only included RCTs on HALG and LAG.
RCTs are the gold standard in study design; however, randomized controlled surgical trials, especially blinding, remain controversial, since the surgeon cannot be blinded to the procedure, and there are practical and ethical barriers to blind patients[26]. Due to the absence of blinding, five studies automatically scored poorly on the Jadad score in this meta-analysis. Although the poor-quality RCTs may be biased due to their inherent design limitations, there is no satisfactory program to resolve this issue. In addition, two of the studies did not report the exact value of the groups’ baseline[16,18], although they clearly reported that the groups were similar at the baseline in the article.
Previously, HALG has been considered the transitional bridge from traditional open surgery to laparoscopic surgery[27-29]. Currently, HALG is universally used for gastrointestinal tumors in China. However, most surgeons may prejudice HALG’s minimal invasiveness because of one hand into the abdominal cavity. In fact, several studies have shown that the important prognostic indicators of HALG, with the exception of incision length, are more advantageous than those of LAG[9,27,30-32]. Additionally, HALG should not be denied as being minimally invasive just because of slightly longer incision (WMD, 0.89 cm; 95%CI, 0.45 to 1.33). There are several possible reasons for this. First, HALG is simpler for isolating the omentum, and groups 5, 6, and 12 lymph nodes under direct vision through the upper abdomen incision, so that it can greatly reduce the laparoscopic operation time. Second, the surgeon’s left hand is more agile than that of the LAG’s assistant. Third, the initial learning-curve of HALG is shorter; thus, surgeons can better acquire the skill to decrease the operation time. Fourth, the incision length is appropriate for digestive reconstruction.
Severe postsurgical complications could increase the hospitalization duration and affect the prognosis. In this meta-analysis, the rates of all postsurgical complications of HALG were lower than those of LAG, which could be attributed to the following reasons: First, HALG have a clearer operative field to isolate groups 5, 6, and 12 lymph nodes, and to complete the digestive reconstruction by the comfortable incision. Second, due to the direct hand assistance, the important structures, particularly the splenic lymph node, could more intuitively be revealed via the laparoscope. Third, HALG has a lower requirement for pneumoperitoneum pressure, so that it favorably maintains the stability of the internal environment. However, those studies did not evaluate the long-term outcomes. Thus, it is important to evaluate the long-term survival of HALG in the future.
To date, surgeons have multiple options to complete gastrectomy, especially the novel totally laparoscopic gastrectomy and robotic gastrectomy. However, the reconstruction process of totally laparoscopic gastrectomy or robotic gastrectomy is difficult[33-35]. Compared with HALG, it also has a longer-learning curve to complete operation[7]. The robotic gastrectomy is similar to minimal need for experienced assistance with HALG. However, the robotic approach is not widely used because of its high price[36,37]. Compared with the cheap equipment of HALG, many hospitals cannot pay for initial purchasing costs and maintenance costs of robotic procedures, especially in undeveloped areas. Additionally, the high hospitalization costs of robotic gastrectomy also affect the choice of patients. Collectively, we still recommend this ordinary HALG to the undeveloped areas in this analysis.
Nevertheless, this study has certain limitations. First, all the included studies were conducted in China, which limited the universal application of the results. Second, all the studies are RCTs, but there are no uniform criteria and no uniform training of surgeons. Due to the poor-quality RCTs, there is an indeterminate risk of bias. Third, although the present study included all the relevant publications from our search, the sample size is still not sufficient. Fourth, three types of gastrectomy were included in this meta-analysis, and the difference between these types is ignored, which may lead to high heterogeneity.
In conclusion, our meta-analysis suggests that HALG is a simpler and safer technique than LAG. HALG should be used as a minimal-access technique, particularly in technologically undeveloped areas. However, further high-quality RCTs with larger sample size should be conducted in order to evaluate this issue.
Hand-assisted laparoscopic gastrectomy (HALG) is a popular operation in China, but some surgeons do not accept it as a minimal-access technique.
If the safety and practicability of HALG can be confirmed by comparing with laparoscopic-assisted gastrectomy (LAG), HALG should be used as a minimal-access technique.
This research aimed to assess the safety and practicability of HALG by comparing the short-term outcomes of HALG and LAG.
The electronic databases of EMBASE, PubMed, China National Knowledge Infrastructure, and Cochrane Library were thoroughly searched, and only randomized controlled trials (RCTs) comparing HALG and LAG were included.
This meta-analysis included five RCTs with 600 cases. Compared with LAG, HALG reduced surgery time, hospital duration, and overall postsurgical complications, and increased the number of retrieved lymphatic nodes and incision length.
HALG is simpler and safer technique than LAG. HALG should be used as a minimal-access technique, especially in technologically undeveloped areas.
It is important to evaluate the long-term survival of hand-assisted laparoscopic gastrectomy in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hori T S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Li JH
| 1. | Zeng L, Wang GP. Status of Cancer Epidemiology and Prevention Research in China. Shijie Zuixin Yixue Xinxi Wenzhai. 2016;16:36-37. [DOI] [Cited in This Article: ] |
| 2. | Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol Biomarkers Prev. 2016;25:16-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2004] [Cited by in F6Publishing: 2263] [Article Influence: 251.4] [Reference Citation Analysis (0)] |
| 3. | Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18694] [Cited by in F6Publishing: 20838] [Article Influence: 2315.3] [Reference Citation Analysis (2)] |
| 4. | Hunter JG. Hand-assisted laparoscopic gastrectomy for cancer: the next last frontier. J Am Coll Surg. 2004;199:436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Cao YK. Challenge and progress of hand-assisted laparoscopic radical gastrectomy. Zhonghua Puwai Kexue Wenxian. 2016;10:334-339. [DOI] [Cited in This Article: ] |
| 6. | Liu Y. Current application and prospects of hand assisted laparoscopic surgery in gastrointestinal tumors. Shijie Huaren Xiaohua Zazhi. 2016;24:3841-3845. [DOI] [Cited in This Article: ] |
| 7. | Gong JQ, Cao YK, Wang YH, Zhang GH, Wang PH, Luo GD. Learning curve for hand-assisted laparoscopic D2 radical gastrectomy. World J Gastroenterol. 2015;21:1606-1613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Gong JQ, Cao YK, Wang YH, Zhang GH, Wang PH, Luo GD. Three-step hand-assisted laparoscopic surgery for radical distal gastrectomy: an effective surgical approach. Int J Clin Exp Med. 2014;7:2156-2164. [PubMed] [Cited in This Article: ] |
| 9. | Gong J, Cao Y, Wang Y, Zhang G, Wang P, Luo G. Three-step hand-assisted laparoscopic d2 radical gastrectomy for chinese obese patients: a highly efficient and feasible surgical approach. J Cancer. 2015;6:120-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Cao YK, Liu LY, Gong JQ, Wang YH, Luo GD, Zhou J, Gan W, Huang L. [Analysis of lymph node dissection patterns in D2 radical gastrectomy by hand-assisted laparoscopic technique]. Zhonghua Wei Chang Wai Ke Za Zhi. 2013;16:970-973. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 11. | Yang K, Zhang WH, Chen XL, Chen XZ, Guo DJ, Zhang B, Chen ZX, Zhou ZG, Hu JK. Comparison of hand-assisted laparoscopic gastrectomy vs. laparoscopy assisted gastrectomy for gastric cancer. Hepatogastroenterology. 2014;61:2411-2415. [PubMed] [Cited in This Article: ] |
| 12. | Akahoshi T, Uehara H, Tomikawa M, Kawanaka H, Hashizume M, Maehara Y. Comparison of open, laparoscopic, and hand-assisted laparoscopic devascularization of the upper stomach and splenectomy for treatment of esophageal and gastric varices: a single-center experience. Asian J Endosc Surg. 2014;7:138-144. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Gong J, Cao Y, Li Y, Zhang G, Wang P, Luo G. Hand-assisted laparoscopic versus laparoscopy-assisted D2 radical gastrectomy: a prospective study. Surg Endosc. 2014;28:2998-3006. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Luo G, Cao Y, Li Y, Gong J, Tang S, Li Y. Hand-assisted laparoscopic vs laparoscopic-assisted radical gastrectomy for advanced gastric cancer: a prospective randomized study. Int J Clin Exp Med. 2017;10:1917-1926. [Cited in This Article: ] |
| 15. | Gao P, Jie Z, Li Z, Cao Y, Xiong J, Wei X, Zhen W, Yi L. Hand-assisted laparoscopic vs laparoscopy-assisted radical gastrectomy: A randomized controlled clinical study. Shiyong Yixue Zazhi. 2019;35:1292-1295. [DOI] [Cited in This Article: ] |
| 16. | Wang C. The short-term effect of Hand-assisted laparoscopic D2 radical gastrectomy for advanced distal gastric cancer. Shandong Yiyao. 2015;55:71-72. [DOI] [Cited in This Article: ] |
| 17. | Xue F, Shi Y, Zhao S. Comparison of laparoscopic assisted vs hand-assisted laparoscopic radical gastrectomy. Anhui Yixue. 2018;39:99-102. [DOI] [Cited in This Article: ] |
| 18. | Yang K, Dan Z, Zhou Q. Evaluation on effect of clinical intervention in D2 Lymphadenectomy for gastric cancer combined with hand-assisted laparoscope. Yunnan Yiyao. 2016;37:609-612. [Cited in This Article: ] |
| 19. | Ahn SH, Kang SH, Lee Y, Min SH, Park YS, Park DJ, Kim HH. Long-term Survival Outcomes of Laparoscopic Gastrectomy for Advanced Gastric Cancer: Five-year Results of a Phase II Prospective Clinical Trial. J Gastric Cancer. 2019;19:102-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, Ryu SW, Cho GS, Song KY, Ryu SY. Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched Korean multicenter study. J Clin Oncol. 2014;32:627-633. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 241] [Cited by in F6Publishing: 258] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 21. | Hu Y, Huang C, Sun Y, Su X, Cao H, Hu J, Xue Y, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Chen P, Liu H, Zheng C, Liu F, Yu J, Li Z, Zhao G, Chen X, Wang K, Li P, Xing J, Li G. Morbidity and Mortality of Laparoscopic Versus Open D2 Distal Gastrectomy for Advanced Gastric Cancer: A Randomized Controlled Trial. J Clin Oncol. 2016;34:1350-1357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 428] [Cited by in F6Publishing: 470] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 22. | Chen G, Xu X, Gong J, Zhang G, Cao Y, Zhang L. [Safety and efficacy of hand-assisted laparoscopic versus open distal gastrectomy for gastric cancer: A systematic review and meta-analysis]. Zhonghua Wei Chang Wai Ke Za Zhi. 2017;20:320-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 23. | Wang G, Zhou J, Sheng W, Dong M. Hand-assisted laparoscopic surgery vs laparoscopic-assisted surgery for colorectal cancer: a Meta-analysis. Zhonghua Putong Waike Zazhi. 2016;25:497-509. [Cited in This Article: ] |
| 24. | Fan X, Dong S, Duan J, Song J. Hand-assisted laparoscopic vs open surgery radical resection of colorectal cancer: a Meta analysis. Zhongguo Zhongliu Waike Zazhi. 2014;6:4-8. [DOI] [Cited in This Article: ] |
| 25. | Cao Y, Zhou J, Liu L, Wang Y, Gong J, Zhang G, Zhang L, Pei hong W, Guo de L. Clinical Control Study of Hand Assisted Laparoscopic D2 Radical Gastrectomy Versus Laparoscopic Assisted D2 Radical Gastrectomy for Gastric Cancer. Zhongguo Puwai Jichu Yu Linchuang Zazhi. 2012;19:1208-1212. [Cited in This Article: ] |
| 26. | Campbell AJ, Bagley A, Van Heest A, James MA. Challenges of randomized controlled surgical trials. Orthop Clin North Am. 2010;41:145-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Kim YW, Bae JM, Lee JH, Ryu KW, Choi IJ, Kim CG, Lee JS, Rho JY. The role of hand-assisted laparoscopic distal gastrectomy for distal gastric cancer. Surg Endosc. 2005;19:29-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Wong SK, Tsui DK, Li MK. Laparoscopic distal gastrectomy for gastric cancer: initial experience on hand-assisted technique and totally laparoscopic technique. Surg Laparosc Endosc Percutan Tech. 2009;19:298-304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Ohki J, Nagai H, Hyodo M, Nagashima T. Hand-assisted laparoscopic distal gastrectomy with abdominal wall-lift method. Surg Endosc. 1999;13:1148-1150. [PubMed] [Cited in This Article: ] |
| 30. | Zhang P, Zhang X, Xue H. Long-term results of hand-assisted laparoscopic gastrectomy for advanced Siewert type II and type III esophagogastric junction adenocarcinoma. Int J Surg. 2018;53:201-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | Zhang GT, Song YC, Zhang XD. Hand-assisted laparoscopic total gastrectomy with regional lymph node dissection for advanced gastric cancer. Surg Laparosc Endosc Percutan Tech. 2014;24:e78-e84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Usui S, Inoue H, Yoshida T, Fukami N, Kudo SE, Iwai T. Hand-assisted laparoscopic total gastrectomy for early gastric cancer. Surg Laparosc Endosc Percutan Tech. 2003;13:304-307. [PubMed] [Cited in This Article: ] |
| 33. | Zhao S, Zheng K, Zheng JC, Hou TT, Wang ZN, Xu HM, Jiang CG. Comparison of totally laparoscopic total gastrectomy and laparoscopic-assisted total gastrectomy: A systematic review and meta-analysis. Int J Surg. 2019;68:1-10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Guerrini GP, Esposito G, Magistri P, Serra V, Guidetti C, Olivieri T, Catellani B, Assirati G, Ballarin R, Di Sandro S, Di Benedetto F. Robotic versus laparoscopic gastrectomy for gastric cancer: The largest meta-analysis. Int J Surg. 2020;82:210-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 35. | Wang S, Su ML, Liu Y, Huang ZP, Guo N, Chen TJ, Zou ZH. Efficacy of totally laparoscopic compared with laparoscopic-assisted total gastrectomy for gastric cancer: A meta-analysis. World J Clin Cases. 2020;8:900-911. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 36. | Qiu H, Ai JH, Shi J, Shan RF, Yu DJ. Effectiveness and safety of robotic versus traditional laparoscopic gastrectomy for gastric cancer: An updated systematic review and meta-analysis. J Cancer Res Ther. 2019;15:1450-1463. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Ahmed HO. An invited commentary on "Robotic versus laparoscopic gastrectomy for gastric cancer: The largest meta-analysis". Int J Surg. 2020;83:159-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |