Copyright
©The Author(s) 2021.
World J Clin Cases. Nov 26, 2021; 9(33): 10300-10307
Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10300
Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10300
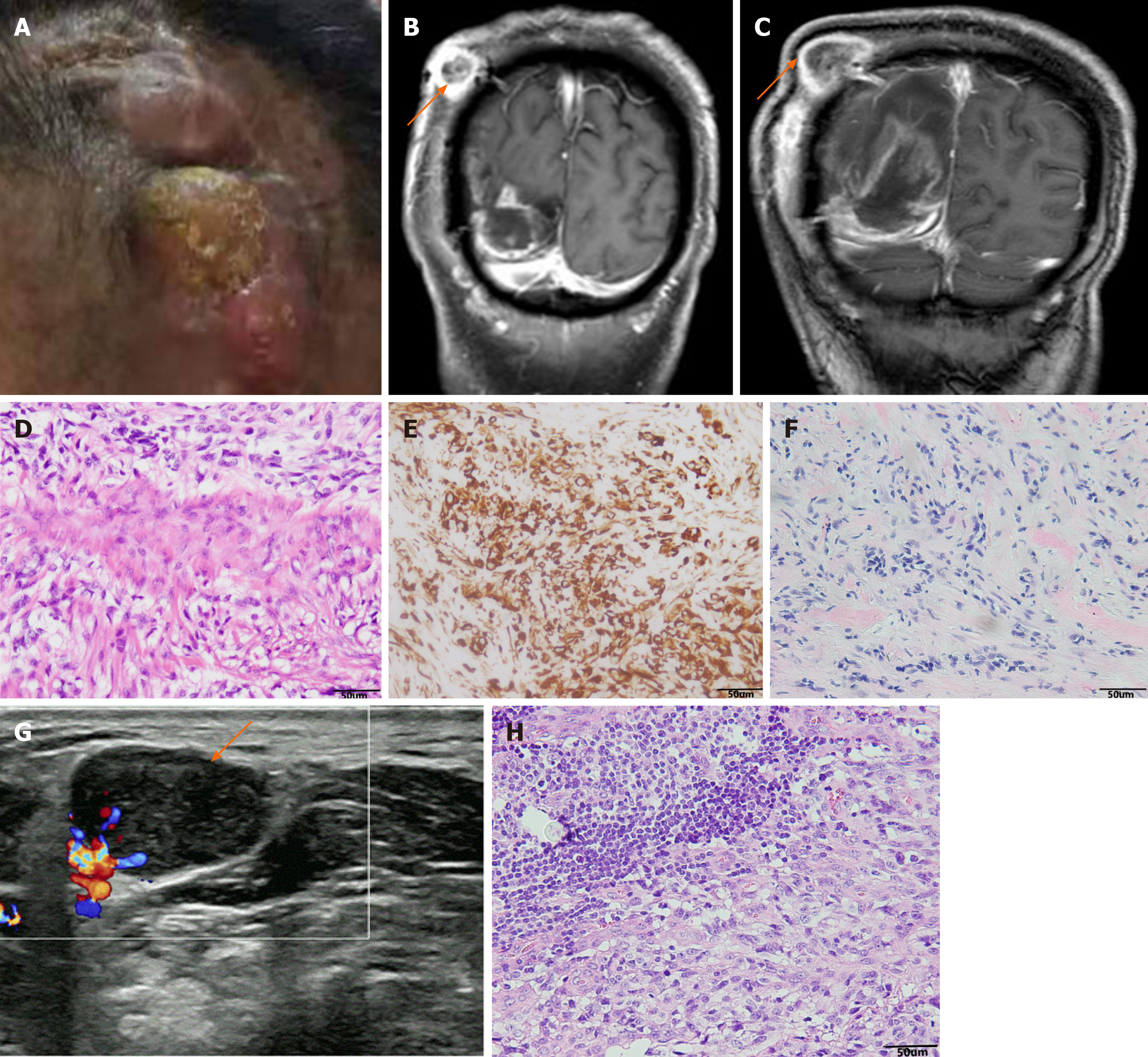
Figure 2 Imaging and pathology before and after the second operation.
A: The patient has a lump on the scalp at the first surgical incision in the right temple; B: 6 mo after first surgery, brain contrast-enhanced magnetic resonance imaging (MRI): intracranial recurrence and scalp transfer; C: Brain contrast-enhanced MRI was re-examined 9 mo after first surgery: both the intracranial recurrent tumors and the scalp metastases have grown up; D: Hematoxylin-eosin staining suggested fibrous tissue proliferation and necrosis, and scattered abnormal cells, which was considered as intracranial GBM metastasis (magnification, × 200); E: GFAP (+) (magnification, × 200); F: Vim (+) (magnification, × 200); G: Ultrasonography revealed enlarged lymph nodes in the right neck (2.1 cm × 1.5 cm); H: Pathological examination of enlarged lymph nodes in the right neck was diagnosed as glioblastoma, hematoxylin-eosin staining (magnification, × 200).
- Citation: Luan XZ, Wang HR, Xiang W, Li SJ, He H, Chen LG, Wang JM, Zhou J. Extracranial multiorgan metastasis from primary glioblastoma: A case report. World J Clin Cases 2021; 9(33): 10300-10307
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10300.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10300