Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10198
Peer-review started: July 9, 2021
First decision: August 8, 2021
Revised: August 9, 2021
Accepted: September 10, 2021
Article in press: September 10, 2021
Published online: November 26, 2021
Neuropathy is a common chronic complication in type 2 diabetes mellitus (T2DM). Statin and metformin are commonly used medications in T2DM patients, and some studies showed statin- or metformin-induced neuropathy.
To evaluate the incidence of neuropathy among patients with T2DM associated with statin and metformin therapies.
Korean Health Insurance Review and Assessment national patient sample data from 2016 and 2017 were used. Patients with T2DM and no complications were divided into statin/metformin/statin + metformin users and non-users. Neuropathy incidence was defined by International Statistical Classification of Diseases and Related Health Problems, 10th revision codes and concomitant prescriptions for anticonvulsants or antidepressants. Logistic regression analyses were conducted to examine the associations between statin/metformin/statin + metformin therapies and the incidence of neuropathy. Propensity score (PS) matching was performed on the basis of age, sex and comorbidities.
Overall, 34964 and 35887 patients with T2DM and no complications were included in the Korean Health Insurance Review and Assessment national patient sample datasets from 2016 and 2017, respectively. Statin therapy was associated with increased risks of neuropathy in 2016 and 2017 [PS-matched odds ratio (OR) = 1.22, 95% confidence interval (CI): 1.08-1.38; PS-matched OR = 1.17, 95%CI: 1.03-1.33, respectively]. Metformin therapy was associated with reduced risks of neuropathy in 2016 and 2017 (PS-matched OR = 0.30, 95%CI: 0.21-0.42; PS-matched OR = 0.44, 95%CI: 0.32-0.60, respectively). Combined statin + metformin therapy was not significantly associated with neuropathy in 2016 or 2017 (PS-matched OR = 0.85, 95%CI: 0.61-1.19; PS-matched OR = 0.95, 95%CI: 0.66-1.38, respectively).
Statin therapy was associated with enhanced risk of new-onset neuropathy in patients with T2DM, but metformin therapy showed the opposite association.
Core Tip: Diabetic neuropathy is one of the most common chronic complications in patients with type 2 diabetes mellitus. Statin is a commonly used lipid lowering agent in patients with type 2 diabetes mellitus, and metformin is background medication for type 2 diabetes mellitus. In some observational studies, statin and metformin were associated with an increased risk of neuropathy. In the present study using Korean Health Insurance Review and Assessment national patient sample data, the use of statin was associated with increased risk of diabetic neuropathy occurrence, whereas metformin use showed a negative association with diabetic neuropathy.
- Citation: Min HK, Kim SH, Choi JH, Choi K, Kim HR, Lee SH. Impacts of statin and metformin on neuropathy in patients with type 2 diabetes mellitus: Korean Health Insurance data. World J Clin Cases 2021; 9(33): 10198-10207
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10198.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10198
The prevalence of type 2 diabetes mellitus (T2DM) and dyslipidemia are increasing with increased population aging worldwide[1,2]. These two diseases are related to cardiovascular disease (CVD), such that they result in higher incidences of CVD-related morbidities and mortalities. Therefore, the proper management of T2DM and dyslipidemia is important for preventing CVD[3,4]. Furthermore, the treatment targets for dyslipidemia differ among comorbidities, and patients with very high risks of CVD are recommended to have low-density lipoprotein-cholesterol levels below 70 mg/dL[3]. Several major risk factors for CVD are known, including dysglycemia (e.g., T2DM)[3]. In practice, statins (i.e. hydroxymethylglutaryl-CoA reductase inhibitors) are used as first-line therapy for dyslipidemia[3]. Despite their broad usage, some studies have shown that statins may induce neuropathy[5,6].
Metformin, a biguanide, is a first-line oral medication for patients with T2DM that can reduce hepatic glucose production and intestinal glucose absorption, but it also enhances insulin sensitivity[4]. In addition to its primary therapeutic effects, metformin has demonstrated anti-inflammatory effects through the modulation of the AMPK/mTOR pathway[7]. Furthermore, metformin does not induce hypoglycemia, which is a critical side effect of other anti-diabetic drugs. Although metformin is commonly used as a background medication in patients with T2DM[4,8], a potential risk for metformin-induced neuropathy has recently been proposed. Patients with T2DM and neuropathy reportedly have lower vitamin B12 levels, and a higher metformin dose is associated with lower vitamin B12 levels[9]. However, the association between metformin and diabetic neuropathy remains controversial[10].
Dyslipidemia in patients with T2DM is more severe in terms of inducing atherosclerosis, high triglyceride levels, reduced high-density lipoprotein-cholesterol levels and elevated low-density lipoprotein-cholesterol levels[11]. Furthermore, there are shared risk factors (e.g., old age and obesity) between T2DM and dyslipidemia[12,13]. Therefore, the use of anti-diabetic medications and statins in both groups of patients are common situations in clinical practice. In addition, neuropathy is a chronic microvascular complication in patients with T2DM that depends on the duration and severity of T2DM. Therefore, primary prevention via proper glycemic control is important[12]. In addition, the avoidance of additional risk of neuropathy is an important consideration. However, little is known regarding the impact of commonly used medications, i.e. statins and metformin, on neuropathy development in patients with T2DM.
The Korean health insurance system covers the entire population of residents in Korea. All health care facilities provide medical services to patients, then submit insurance benefit claims to the national health insurance service. These insurance claims are collected in the Health Insurance Review and Assessment (HIRA) database, which is used annually to produce representative sample data comprising approximately 3% of all insurance claims, the HIRA national patient sample (NPS). HIRA-NPS data are useful for analyzing various medical insurance-related data including treatments, procedures, prescriptions, patient demographics and health care provider information. Furthermore, these data can be used to analyze the incidences of specific disorders based on operational definitions.
In the present study, we evaluated the influence of statin, metformin and statin + metformin therapies on the incidence of neuropathy in patients with T2DM using Korean HIRA-NPS data from 2016 and 2017.
Korean HIRA-NPS data are produced annually, and this study included HIRA-NPS data from 2016 and 2017. Korea has a unique government-funded insurance system, in which claims data are generated when healthcare facilities file insurance benefit claims with HIRA. These claims data include diverse information such as patient demo
This study was conducted in accordance with the tenets of the Declaration of Helsinki (1964). Written informed consent for enrollment was waived because the data were provided by HIRA. This study was approved by the Institutional Review Board of Konkuk University Medical Center (Approval number: 2020-12-057).
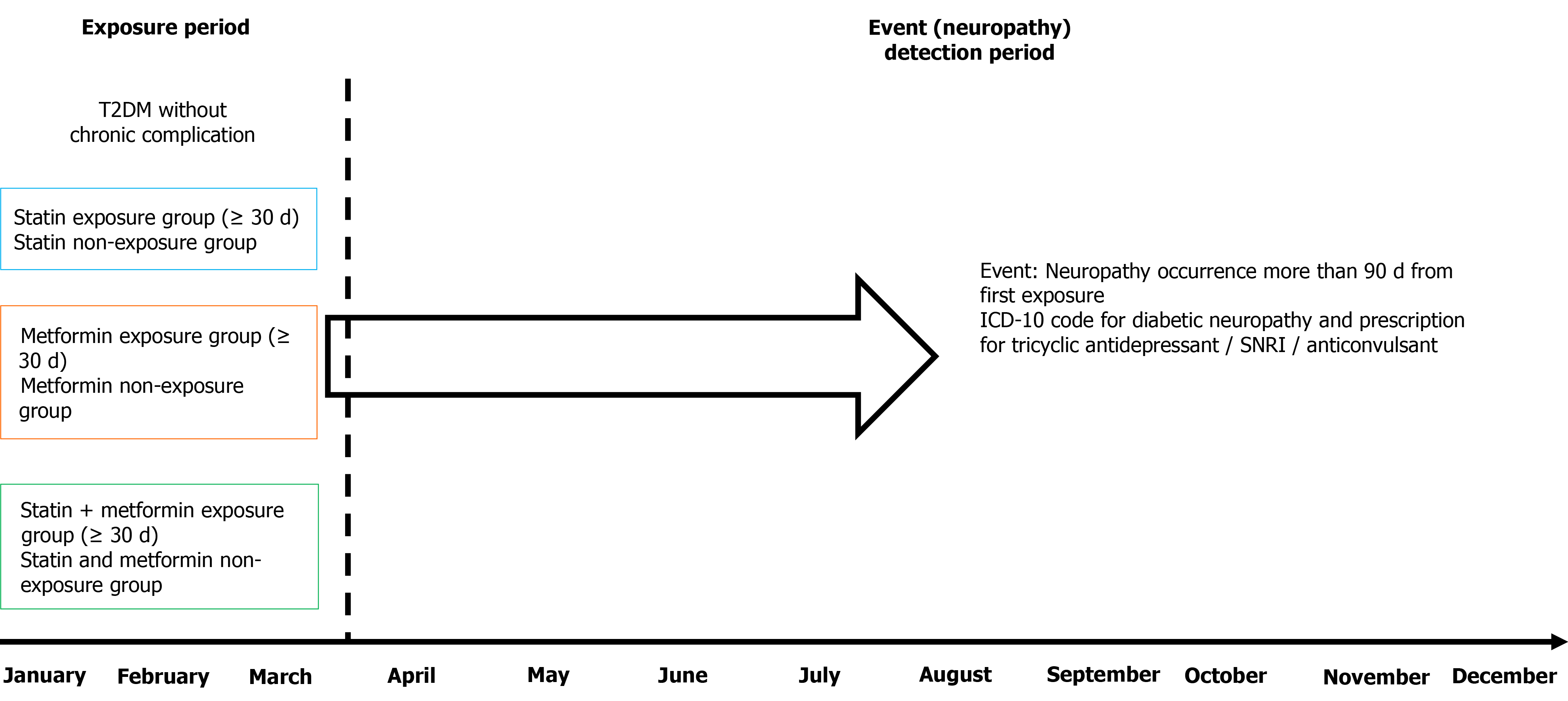
Considering the characteristics of HIRA-NPS data, operational definitions of T2DM and new-onset neuropathy were used in this study. Patients were selected based on the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10). At baseline, ICD-10 codes for T2DM without chronic complications were selected by searching for the following ICD-10 codes: E110, E111, E119, E120, E121, E129, E130, E131, E139, E140, E141 and E149. In addition, participants were included if they had anatomic therapeutic chemical codes for prescriptions of the anti-diabetic medications A10A and A10B for more than 30 d within the first 3 mo. Patients were excluded if they were prescribed antidepressants (N06A) or anticonvulsants (N03AX12 and N03AX16) within the first 3 mo because these could be used for diabetic neuropathy[14]. Considering the etiology of T2DM, patients older than 30 years of age were included in the study. To exclude other causes of neuropathy, patients with connective tissue diseases (ICD-10 codes: M05, M06, M30, M31, M32, M33, M34, M35 and M45), renal failure (ICD-10 codes: I120, I131, I132, N17, N18 and N19) and malignancy (ICD-10 codes: C00–C97) were excluded at baseline. The first 3 mo were selected as the duration of exposure to statin/metformin/statin + metformin, and exposure to each medication was defined as a prescription for more than 30 d of treatment. Patients who had never been prescribed these medications were defined as the non-exposure group. The statin + metformin non-exposure group was defined as patients who had not been exposed to statins or metformin. Anatomic therapeutic chemical codes were used to identify prescriptions for statins (C10AA01–C10AA08) and metformin (A10BA02). Patients with combination medications, such as statins with other dyslipidemia or antihypertensive medications or metformin with other anti-diabetic medications, were excluded from the assessment of medication exposure to specifically evaluate the influence of statins or metformin on neuropathy incidence. The incidence of new-onset neuropathy was investigated within the final 9 mo of the index year. The combined disease codes for diabetic neuropathy (ICD-10 codes: E114, E124, E134, E144, G590 and G632) and prescriptions of either tricyclic antidepressants, serotonin–norepinephrine reuptake inhibitors or anticonvulsants recommended by the American Diabetes Association[14] [anatomic therapeutic chemical codes: N03AX12 (gabapentin), N03AX16 (pregabalin), N06AA01 (desipramine), N06AA02–N06AA03 (imipramine), N06AA09 (amitriptyline), N06AA10 (nortriptyline), N06AX16 (venlafaxine) and N06AX21 (duloxetine)] for more than 30 d were used to identify patients with new-onset neuropathy. The ICD-10 codes for diabetic neuropathy were selected because the use of anticonvulsants or serotonin–norepinephrine reuptake inhibitors is covered by national health insurance for patients with diabetic neuropathy but not for patients with nonspecific neuropathy. Therefore, in Korea, neuropathy medications (i.e. anticonvulsants or antidepressants) are usually prescribed after the submission of the ICD-10 codes for diabetic neuropathy in patients with T2DM. In this study, we identified drug-induced neuropathy by only including patients with ICD-10 codes for diabetic neuropathy and combined prescriptions of antidepressants or anticonvulsants after at least 90 d of exposure to statin/ metformin/statin + metformin therapies. The schematic diagram of the research protocol is presented in Figure 1. The patients were divided into the following 10-year age-group intervals: 30–39, 40–49, 50–59, 60–69 and > 70 years.
Baseline demographic characteristics are summarized as numbers and percentages and compared using the χ2 test or Fisher’s exact test. Propensity score (PS)-matching was performed by 1:1 matching according to age, sex and comorbidities included in the Charlson Comorbidity Index[15]. Logistic regression analyses were performed to calculated crude and PS-matched odds ratios (ORs) for new-onset neuropathy. Values of P < 0.05 were considered to indicate statistical significance. All tests were performed using R software (R for Windows 3.3.2; The R Foundation for Statistical Computing, Vienna, Austria).
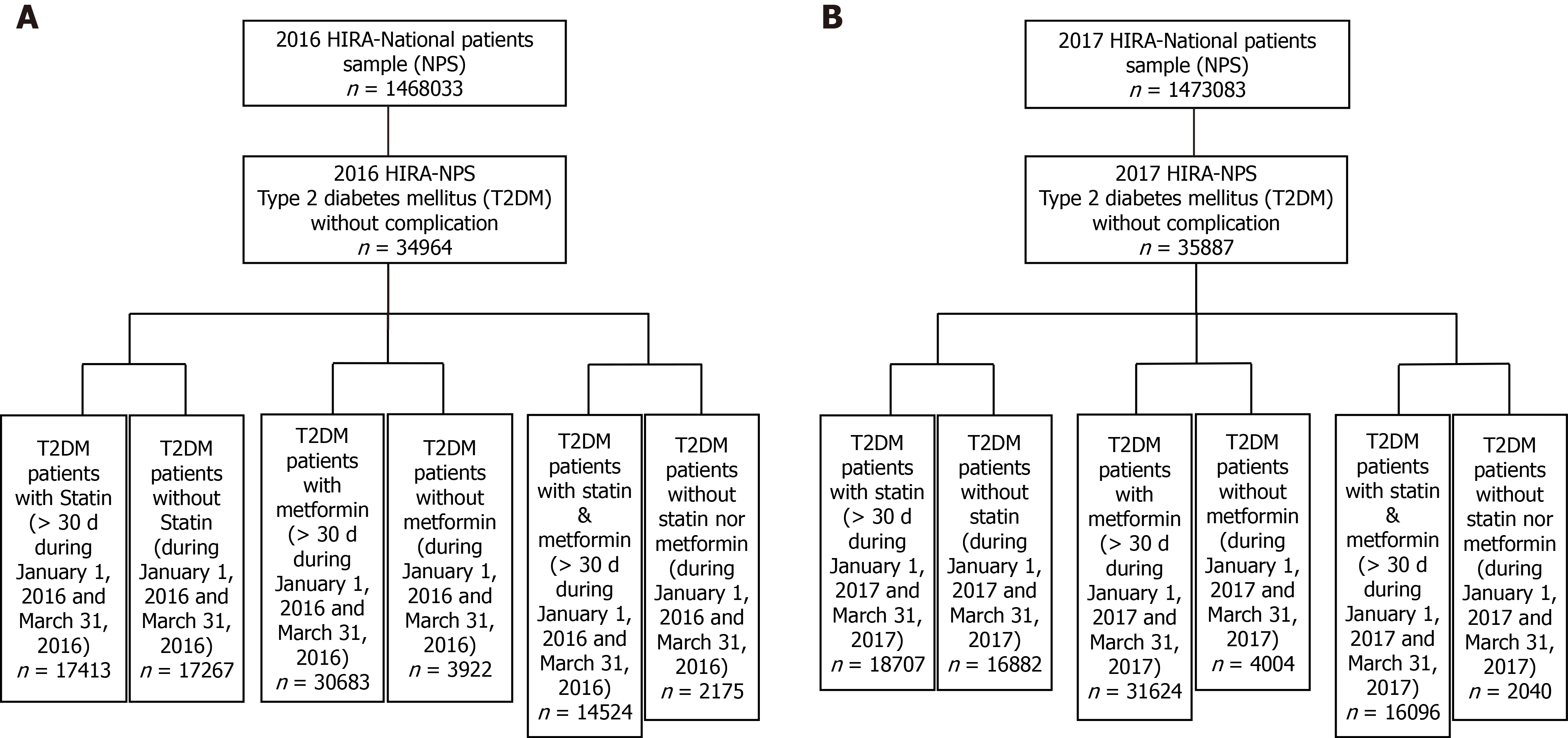
The HIRA-NPS datasets for 2016 and 2017 included 1468033 and 1473083 patients, respectively. In each year, 34964 and 35887 patients had T2DM without diabetic complications, respectively (Figure 2). Statin therapy analyses showed that 17413 patients received statin therapy, and 17267 patients did not receive statin therapy in 2016. In 2017, 18707 patients received statin therapy, and 16882 patients did not. The overall age distributions between the two groups were comparable in both 2016 and 2017 (Supplementary Tables 1 and 2). The incidence of neuropathy was greater in statin users than in statin non-users in 2016 [582/17413 (3.34%) vs 477/17267 (2.76%), P = 00017]. In 2017, statin users had a greater incidence of neuropathy compared with statin non-users, but this difference was not statistically significant [562/18707 (3.00%) vs 449/16882 (2.66%), P = 0.0507]. However, comparisons after PS matching showed similar results in both 2016 and 2017, such that the incidence of neuropathy was greater in statin users than in statin non-users [2016: 579/17267 (3.35%) vs 477/17267 (2.76%), P = 0.0014; 2017: 523/16882 (3.10%) vs 449/16882 (2.66%), P = 0.0160; Table 1].
| Propensity score-matched1 | ||||||
| Statin user, n (%) | Statin non-user, n (%) | P value | Statin user, n (%) | Statin non-user, n (%) | P value | |
| 2016 | ||||||
| Neuropathy incidence | 582/17413 (3.34) | 477/17267 (2.76) | 0.0017 | 579/17267 (3.35) | 477/17267 (2.76) | 0.0014 |
| 2017 | ||||||
| Neuropathy incidence | 562/18707 (3.00) | 449/16882 (2.66) | 0.0507 | 523/16882 (3.10) | 449/16882 (2.66) | 0.0160 |
Metformin therapy analyses showed that 30683 patients received metformin therapy, and 3922 patients did not receive metformin therapy in 2016. In 2017, 31624 patients received metformin therapy, and 4004 patients did not. The overall age distribution did not differ significantly between the two groups in 2016 or 2017 (Supplementary Tables 3 and 4). The incidence of neuropathy was lower in metformin users than in metformin non-users in 2016 [914 (2.98%) vs 158 (4.03%), P = 0.0004]. In 2017, metformin users had a reduced incidence of neuropathy compared with metformin non-users, but this difference was not statistically significant [959 (3.03%) vs 143 (3.57%), P = 0.0635]. Comparisons after PS matching showed lower incidences of neuropathy in metformin users in both 2016 and 2017 (Table 2).
| Propensity score-matched1 | ||||||
| Metformin user, n (%) | Metformin non-user, n (%) | P value | Metformin user, n (%) | Metformin non-user, n (%) | P value | |
| 2016 | ||||||
| Neuropathy incidence | 914/30683 (2.98) | 158/3922 (4.03) | 0.0004 | 49/3922 (1.25) | 158/3922 (4.03) | < 0.0001 |
| 2017 | ||||||
| Neuropathy incidence | 959/31624 (3.03) | 143/4004 (3.57) | 0.0635 | 64/4004 (1.60) | 143/4004 (3.57) | < 0.0001 |
Combined statin + metformin therapy analyses showed that 14524 patients received both therapies in 2016, but 2175 patients received neither therapy. In 2017, 16096 received both therapies, but 2040 patients received neither therapy. The age distributions were comparable between statin + metformin users and non-users in both 2016 and 2017 (Supplementary Tables 5 and 6). In 2016, statin + metformin users had a lower incidence of neuropathy compared with statin + metformin non-users [438 (3.02%) vs 83 (3.82%), P = 0.0452]. This difference was also present in 2017 but was not statistically significant [472 (2.93%) vs 65 (3.19%), P = 0.5239]. Comparisons after PS matching showed that the incidences of neuropathy were comparable between the two groups in both 2016 and 2017 (Table 3).
| Propensity score-matched1 | ||||||
| Statin + metformin user, n (%) | Non-user, n (%) | P value | Statin + metformin user, n (%) | Non-user, n (%) | P value | |
| 2016 | ||||||
| Neuropathy incidence | 438/14524 (3.02) | 83/2175 (3.82) | 0.0452 | 71/2175 (3.26) | 83/2175 (3.82) | 0.3248 |
| 2017 | ||||||
| Neuropathy incidence | 472/16096 (2.93) | 65/2040 (3.19) | 0.5239 | 62/2040 (3.04) | 65/2040 (3.19) | 0.7868 |
Logistic regression analysis demonstrated that statin therapy was significantly and positively associated with neuropathy incidence in both 2016 and 2017 [PS-matched OR = 1.22, 95% confidence interval (CI): 1.08-1.38; PS-matched OR = 1.17, 95%CI: 1.03-1.33, respectively]. Furthermore, metformin therapy was consistently negatively associated with neuropathy incidence in both 2016 and 2017 (PS-matched OR = 0.30, 95%CI: 0.21-0.42; PS-matched OR = 0.44, 95%CI: 0.32-0.60, respectively). Combined statin + metformin therapy was not associated with a significant risk of neuropathy in 2016 or 2017. The results of logistic regression analyses are summarized in Table 4.
| Propensity score-matched1 | ||||
| OR | 95%CI | OR | 95%CI | |
| 2016 | ||||
| Statin use | 1.22 | 1.07-1.38 | 1.22 | 1.08-1.38 |
| Metformin use | 0.73 | 0.61-0.87 | 0.30 | 0.21-0.42 |
| Statin + metformin use | 0.78 | 0.62-1.01 | 0.85 | 0.61-1.19 |
| 2017 | ||||
| Statin use | 1.13 | 1.00-1.29 | 1.17 | 1.03-1.33 |
| Metformin use | 0.84 | 0.71-1.02 | 0.44 | 0.32-0.60 |
| Statin + metformin use | 0.92 | 0.70-1.21 | 0.95 | 0.66-1.38 |
In the present study, we demonstrated an elevated risk of neuropathy among statin users and a reduced risk of neuropathy among metformin users in patients with T2DM. Notably, combined statin + metformin therapy was not associated with new-onset neuropathy in patients with T2DM. These findings were based on real-world insurance claims data from the Korean population. Statins can cause neuropathy, and impaired mitochondrial transport and a reduction in vitamin E levels have been proposed as underlying mechanisms[16]. An analysis of 757 patients with diabetes revealed a significantly greater relative risk of peripheral neuropathy in patients with diabetes who were receiving statin therapy[6]. Our results included a larger sample size than in previous studies and confirmed the elevated risk of neuropathy in patients with T2DM during statin therapy.
The influence of metformin therapy on neuropathy incidence is not yet established. Strict control of hyperglycemia is the most important treatment principle for preventing diabetic microvascular complications including neuropathy[17], and metformin exerts anti-diabetic effects via several mechanisms. Therefore, metformin can function to prevent the onset of diabetic neuropathy. In an animal study, metformin treatment protected against neural damage by increasing the levels of neural growth factor, vascular endothelial growth factor and anti-inflammatory factors[18]. Another animal study demonstrated that metformin preserved peripheral nerve fiber density and that the beneficial effects of metformin were comparable with those of alpha lipoic acid, an antioxidant used in the clinical treatment of diabetic neuropathy[19].
By contrast, metformin causes vitamin B12 deficiency and may subsequently induce diabetic neuropathy[20]. In a cross-sectional study, low to borderline vitamin B12 levels were more common in patients with diabetic neuropathy than in patients without (64% vs 17%)[9]. However, another study demonstrated a non-significant association between metformin therapy and vitamin B12 levels and showed that vitamin B12 levels were not associated with the severity or prevalence of neuropathy in patients with T2DM[10]. The vitamin B12 reductions were dose-dependent in patients with T2DM who were receiving metformin therapy, and patients with metformin daily doses greater than 1500 mg had a significant risk of vitamin B12 deficiency[21]. In the present study, we found a reduced risk of neuropathy in patients with T2DM who were receiving metformin therapy. Further studies to stratify patients according to metformin daily doses and prospectively collect vitamin B12 and blood glucose levels could reveal whether metformin dose influences the incidence of neuropathy and which aspect (vitamin B12 or blood glucose) more strongly influences neuropathy development during metformin therapy.
We demonstrated that combined metformin + statin therapy did not enhance or reduce the risk of neuropathy in patients with T2DM, although statin therapy enhanced the risk of neuropathy and metformin therapy reduced the risk of neuropathy in these patients. The present results do not clearly indicate whether concomitant metformin administration can reduce the risk of statin-induced neuropathy in patients with T2DM because the findings were based on epidemiological data. However, metformin is regarded as background anti-diabetic medication and is used in most patients with T2DM, except those with contraindications or severe metformin-related side effects[4,8]. Our results suggest a beneficial effect of metformin in terms of reducing the risk of neuropathy, especially in patients with T2DM who are receiving statin therapy.
There were some limitations in the present study. First, the data were retros
We demonstrated the influence of statin and metformin therapies on the incidence of neuropathy in patients with T2DM. Statin therapy enhanced the risk of neuropathy in patients with T2DM, whereas metformin therapy reduced this risk. Combined statin + metformin therapy did not have a significant impact on the incidence of neuropathy. Therefore, when prescribing statin therapy for patients with T2DM, physicians should assess the potential for neuropathy development and consider the addition of metformin to reduce this risk.
Statin and metformin are widely used medications in patients with type 2 diabetes mellitus (T2DM). These medications have been claimed as causative agents for neuropathy.
To identify the incidence and risk of statin, metformin and statin + metformin therapy on new onset neuropathy.
The incidence of neuropathy was evaluated and compared between T2DM patients who used or did not use statin/metformin/statin + metformin by using Korean Health Insurance Review and Assessment - national patient sample data.
The prospective cohort study used nation-wide health insurance data.
Statin therapy showed a positive association (odds ratio = 1.22, 95% confidence interval: 1.08-1.38], whereas metformin therapy showed a negative association with new onset neuropathy (odds ratio = 0.30, 95% confidence interval: 0.21-0.42) in patients with T2DM. Combination therapy of statin and metformin did not have an effect on new onset neuropathy of T2DM patients.
The widely used medications in T2DM, statin and metformin, could have an effect on neuropathy development in T2DM patients. Physicians should pay attention to new onset neuropathy when using statin in T2DM patients.
Nevertheless, further studies are required to reveal underlying mechanisms of statin and metformin on new onset neuropathy of T2DM.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Endocrinology and metabolism
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang DM S-Editor: Yan JP L-Editor: Filipodia P-Editor: Xing YX
| 1. | Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol. 2014;2:56-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 534] [Cited by in F6Publishing: 519] [Article Influence: 51.9] [Reference Citation Analysis (0)] |
| 2. | Gan W, Liu Y, Luo KH, Liang SS, Wang H, Li M, Zhang YX, Huang HJ. The prevalence change of hyperlipidemia and hyperglycemia and the effectiveness of yearly physical examinations: an eight-year study in Southwest China. Lipids Health Dis. 2018;17:70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/ NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 678] [Cited by in F6Publishing: 1049] [Article Influence: 209.8] [Reference Citation Analysis (1)] |
| 4. | Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, Park SO, Hur KY, Chon S, Moon MK, Kim NH, Kim SY, Rhee SY, Lee KW, Kim JH, Rhee EJ, Chun S, Yu SH, Kim DJ, Kwon HS, Park KS; Committee of Clinical Practice Guidelines, Korean Diabetes Association. 2019 Clinical Practice Guidelines for Type 2 Diabetes Mellitus in Korea. Diabetes Metab J. 2019;43:398-406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 155] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 5. | Gaist D, Jeppesen U, Andersen M, García Rodríguez LA, Hallas J, Sindrup SH. Statins and risk of polyneuropathy: a case-control study. Neurology. 2002;58:1333-1337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 197] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | Hammad MA, Syed Sulaiman SA, Alghamdi S, Mangi AA, Aziz NA, Mohamed Noor DA. Statins-related peripheral neuropathy among diabetic patients. Diabetes Metab Syndr. 2020;14:341-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Cameron AR, Morrison VL, Levin D, Mohan M, Forteath C, Beall C, McNeilly AD, Balfour DJ, Savinko T, Wong AK, Viollet B, Sakamoto K, Fagerholm SC, Foretz M, Lang CC, Rena G. Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status. Circ Res. 2016;119:652-665. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 340] [Cited by in F6Publishing: 417] [Article Influence: 52.1] [Reference Citation Analysis (0)] |
| 8. | American Diabetes Association. 8. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41:S73-S85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 521] [Cited by in F6Publishing: 535] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 9. | Alvarez M, Sierra OR, Saavedra G, Moreno S. Vitamin B12 deficiency and diabetic neuropathy in patients taking metformin: a cross-sectional study. Endocr Connect. 2019;8:1324-1329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Elhadd T, Ponirakis G, Dabbous Z, Siddique M, Chinnaiyan S, Malik RA. Metformin Use Is Not Associated With B12 Deficiency or Neuropathy in Patients With Type 2 Diabetes Mellitus in Qatar. Front Endocrinol (Lausanne). 2018;9:248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2009;5:150-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 415] [Cited by in F6Publishing: 496] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 12. | DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, Hu FB, Kahn CR, Raz I, Shulman GI, Simonson DC, Testa MA, Weiss R. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 865] [Cited by in F6Publishing: 982] [Article Influence: 109.1] [Reference Citation Analysis (0)] |
| 13. | Bayram F, Kocer D, Gundogan K, Kaya A, Demir O, Coskun R, Sabuncu T, Karaman A, Cesur M, Rizzo M, Toth PP, Gedik V. Prevalence of dyslipidemia and associated risk factors in Turkish adults. J Clin Lipidol. 2014;8:206-216. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 14. | Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, Sosenko JM, Ziegler D. Diabetic Neuropathy: A Position Statement by the American Diabetes Association. Diabetes Care. 2017;40:136-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1095] [Cited by in F6Publishing: 1117] [Article Influence: 159.6] [Reference Citation Analysis (1)] |
| 15. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32099] [Cited by in F6Publishing: 34949] [Article Influence: 944.6] [Reference Citation Analysis (0)] |
| 16. | Pergolizzi JV Jr, Magnusson P, LeQuang JA, Razmi R, Zampogna G, Taylor R Jr. Statins and Neuropathic Pain: A Narrative Review. Pain Ther. 2020;9:97-111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | American Diabetes Association. 10. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41:S105-S118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 192] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 18. | Lós DB, Oliveira WH, Duarte-Silva E, Sougey WWD, Freitas EDSR, de Oliveira AGV, Braga CF, França MER, Araújo SMDR, Rodrigues GB, Rocha SWS, Peixoto CA, Moraes SRA. Preventive role of metformin on peripheral neuropathy induced by diabetes. Int Immunopharmacol. 2019;74:105672. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Kim SH, Park TS, Jin HY. Metformin Preserves Peripheral Nerve Damage with Comparable Effects to Alpha Lipoic Acid in Streptozotocin/High-Fat Diet Induced Diabetic Rats. Diabetes Metab J. 2020;44:842-853. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Aroda VR, Edelstein SL, Goldberg RB, Knowler WC, Marcovina SM, Orchard TJ, Bray GA, Schade DS, Temprosa MG, White NH, Crandall JP; Diabetes Prevention Program Research Group. Long-term Metformin Use and Vitamin B12 Deficiency in the Diabetes Prevention Program Outcomes Study. J Clin Endocrinol Metab. 2016;101:1754-1761. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 240] [Cited by in F6Publishing: 247] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 21. | Kim J, Ahn CW, Fang S, Lee HS, Park JS. Association between metformin dose and vitamin B12 deficiency in patients with type 2 diabetes. Medicine (Baltimore). 2019;98:e17918. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |