Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7671
Peer-review started: April 29, 2021
First decision: May 26, 2021
Revised: June 20, 2021
Accepted: July 29, 2021
Article in press: July 29, 2021
Published online: September 16, 2021
Endoscopic retrograde cholangiopancreatography (ERCP) is the primary choice for removing common bile duct (CBD) stones in Billroth II anatomy patients. The recurrence of CBD stones is still a challenging problem.
To evaluate CBD morphology and other predictors affecting CBD stone recurrence.
A retrospective case-control analysis was performed on 138 CBD stones patients with a history of Billroth II gastrectomy, who underwent therapeutic ERCP for stone extraction at our center from January 2011 to October 2020. CBD morphology and other predictors affecting CBD stone recurrence were examined by univariate analysis and multivariate logistic regression analysis.
CBD morphology (P < 0.01) and CBD diameter ≥ 1.5 cm (odds ratio [OR] = 6.15, 95% confidence interval [CI]: 1.87-20.24, P < 0.01) were the two independent risk factors. In multivariate analysis, the recurrence rate of patients with S type was 16.79 times that of patients with straight type (OR = 16.79, 95%CI: 4.26-66.09, P < 0.01), the recurrence rate of patients with polyline type was 4.97 times that of patients with straight type (OR = 4.97, 95%CI: 1.42-17.38, P = 0.01), and the recurrence rate of S type patients was 3.38 times that of patients with polyline type (OR = 3.38, 95%CI: 1.07-10.72, P = 0.04).
CBD morphology, especially S type and polyline type, is associated with increased recurrence of CBD stones in Billroth II anatomy patients.
Core Tip: Common bile duct (CBD) stone recurrence in Billroth II anatomy patients is challenging, and CBD morphology had never been noticed as a potential risk factor for CBD stone recurrence. In this study, CBD morphology was identified to be the independent risk factor for CBD stone recurrence in Billroth II anatomy patients. S type and polyline type were associated with an increased risk of recurrent CBD stones. Periodic surveillance and prophylactic therapy is recommended for Billroth II anatomy patients with S type and polyline type after successful endoscopic retrograde cholangiopancreatography.
- Citation: Ji X, Jia W, Zhao Q, Wang Y, Ma SR, Xu L, Kan Y, Cao Y, Fan BJ, Yang Z. Common bile duct morphology is associated with recurrence of common bile duct stones in Billroth II anatomy patients. World J Clin Cases 2021; 9(26): 7671-7681
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7671.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7671
As endoscopic retrograde cholangiopancreatography (ERCP) is widely performed for the treatment of choledocholithiasis in Billroth II anatomy patients, the complications after ERCP gradually reveal. The recurrence of choledocholithiasis, as one of the long-term complications, is still a challenging problem[1-4]. As reported, the recurrence rate of common bile duct (CBD) stones after therapeutic ERCP was 2%-22%[5-8], and once CBD stones recurred, the next recurrence rate increased with the number of recurrences[9].
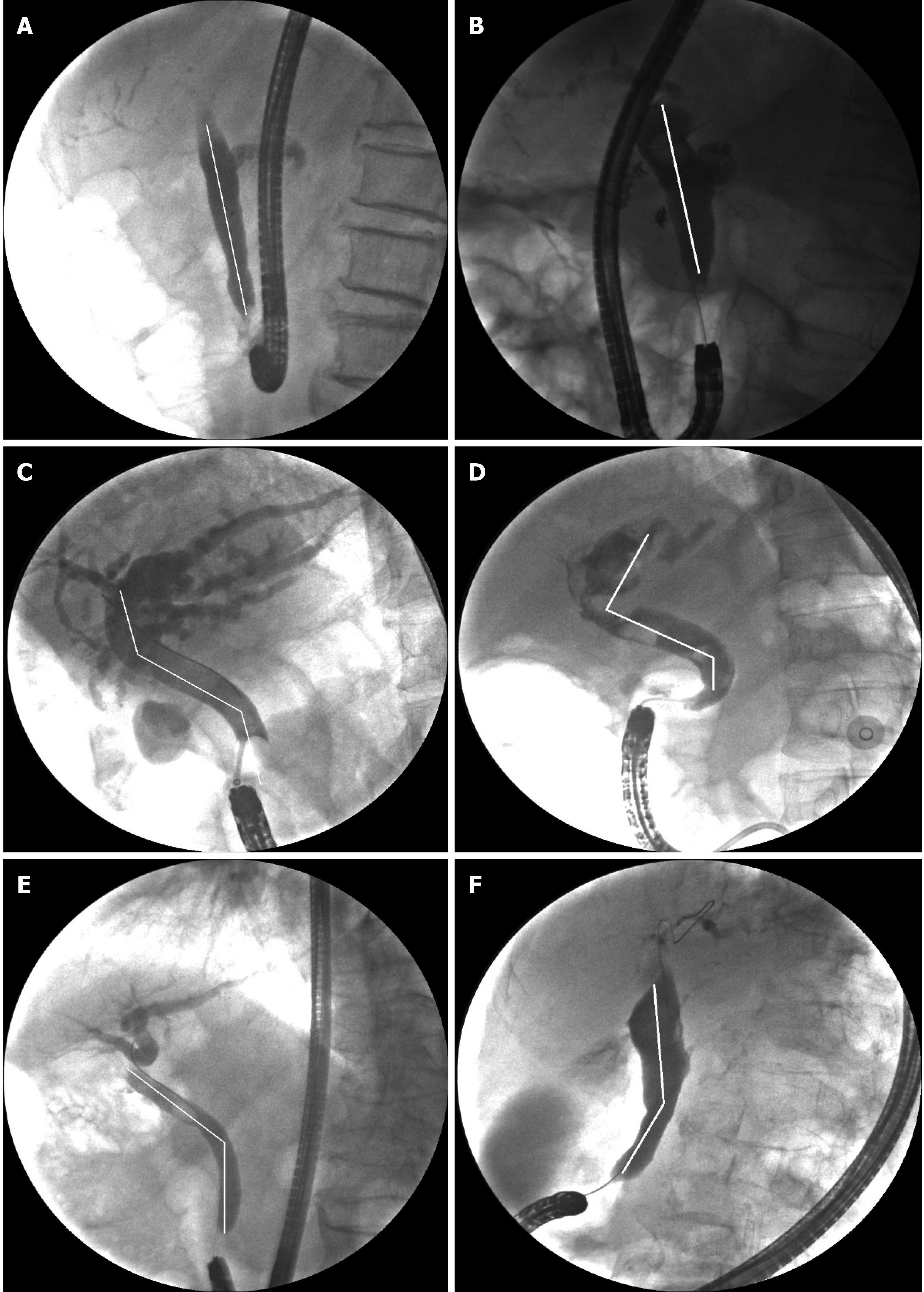
Patients with surgically altered anatomy, such as a Billroth II gastrectomy, might have an altered CBD morphology, which makes the operation of ERCP more complicated, the success rate decrease, and the recurrence rate increase[10]. Thus, we speculated that there is a potential association between CBD morphology and CBD stone recurrence. By searching the literature, we found potential factors for stone recurrence, including age, periampullary diverticulum (PAD), CBD diameter, CBD stone diameter, multiple CBD stones, endoscopic biliary sphincterotomy (EST), endoscopic papillary large balloon dilation (EPLBD), endoscopic papillary balloon dilation (EPBD), EST with balloon dilation (ESBD), cholecystectomy, and CBD angulation[11-15]. In the present study, CBD morphology was defined as the cholangiogram morphology from the confluence of the left and right hepatic ducts to the distal CBD entering the duodenum. We classified the CBD morphology into straight type (Figure 1A and B), S type (Figure 1C and D), and polyline type (Figure 1E and F) and explored whether different shapes of CBD and other factors influence CBD stone recurrence after successful endoscopic therapy in Billroth II anatomy patients.
Stone recurrence was defined by the presence of CBD stones at least 6 mo after previous CBD stones were entirely removed by ERCP. At least two stone recurrences defined multiple recurrences after the first ERCP[16]. Patients who visited our hospital had their CBD stones confirmed by abdominal computed tomography and ERCP. From January 2011 to October 2020, 629 patients with a history of Billroth II gastrectomy underwent successful ERCP for CBD stones at the General Hospital of Northern Theater Command. The exclusion criteria were as follows: (1) Patients without specific stones during the ERCP; (2) patients with tumors of the duodenal papilla, CBD, gallbladder, or liver; (3) patients who had not removed their stones completely after the first ERCP; and (4) patients with incomplete clinical data. A total of 138 patients who underwent complete stone removal were enrolled, and 27 of them recurred up.
All ERCP procedures were performed by experienced endoscopists with at least 500 cases. In our institution, prophylactic antibiotics are used in patients without evidence of cholangitis before ERCP. ERCP was served with a side-viewing duodenoscope (JF-240/260, TJF-240/260; Olympus Medical, Tokyo, Japan), a forward-viewing gastroscope (Olympus GIF-H260/Q260), or a forward-viewing colonoscope (Olympus CF-H260/Q260) after the patient was sedated with intravenous dexmedetomidine, midazolam, and propofol in the left lateral decubitus position. Briefly, the operator completed the wire-guided biliary cannulation with a double-lumen sphincterotome. Precut sphincterotomy or double-wire technique was prepared for difficult biliary cannulation. As selective biliary cannulation was achieved, depending on CBD stones, the operator executed the therapeutic intervention, which included EST, ESBD, and EPLBD. On cholangiogram, the CBD diameter and CBD stone diameter were determined by calculation with the ratio to the diameter of the duodenoscope, and the CBD morphology was determined by the operator before stone removal. After the therapeutic intervention, the operator chose to remove stones with a retrieval balloon and/or a basket with or without mechanical lithotripsy. The CBD stones were regarded as completely removed when all the present endoscopists agreed on the absence of a stone. The CBD morphology was confirmed again by the other operator on the last cholangiogram.
Assessed factors included the CBD morphology, the diameter of CBD, and the largest stone, which were measured from the cholangiogram under the condition of complete contrast injection, with the patient placed in the left lateral decubitus position. CBD morphology was determined by at least two operators before and after the operation. CBD morphology was classified as straight type, S type, or polyline type according to the shape of CBD from the endoscopic view: Straight type, the CBD was straight without bending; S type, the CBD was S-shaped with two bends; polyline type, the CBD had one bend.
Statistical analyses were performed with SPSS 26.0. Categorical data are reported as frequencies (%), and continuous data are reported as the median (range) or mean ± SD. Student’s t-test was used for continuous variables and Fisher’s exact test or χ2 test for categorical variables. Independent risk factors were analyzed by multivariate logistic regression analysis with a forward likelihood ratio. P < 0.05 was considered statistically significant.
A total of 138 patients with Billroth II anatomy who underwent ERCP between January 2011 and October 2020 were retrospectively identified from the collected database, with a follow-up period of 54.4 ± 32.6 mo. The average age was 72.3 years old, and 107 (77.5%) patients were male. The recurrence rate was 19.6% (27/138). No statistically significant differences were observed in patient characteristics between the recurrence and non-recurrence groups, which included age, sex, CBD diameter, largest CBD stone diameter ≥ 1.2 cm, CBD stone number ≥ 2, muddy stones, initial ampullary intervention (EST, EPBD/EPLBD, and ESBD), and cholecystectomy (Tables 1 and 2).
| n (%) | |
| Patients | 138 |
| Male | 107 (77.5) |
| Age (mean ± SD, yr) | 72.3 ± 10.5 |
| PAD | 40 (29.0) |
| CBD diameter (mean ± SD, cm) | 1.4 ± 0.6 |
| CBD diameter ≥ 1.2 cm | 110 (79.7) |
| CBD diameter ≥ 1.5 cm | 73 (52.9) |
| Largest CBD stone diameter ≥ 1.2 cm | 68 (49.3) |
| CBD stone number ≥ 2 | 56 (40.6) |
| Muddy stones | 20 (14.5) |
| Initial ampullary intervention | |
| EST | 8 (5.8) |
| EPBD/EPLBD | 79 (57.2) |
| ESBD | 28 (20.3) |
| CBD morphology | |
| Straight type | 69 (50.0) |
| S type | 22 (15.9) |
| Polyline type | 47 (34.1) |
| Cholecystectomy | 8 (5.8) |
| Procedure time (mean ± SD, min) | 38.3 ± 19.5 |
| Recurrence (n = 27) | Non-recurrence (n = 111) | P value | |
| Sex (male/female) | 21/6 | 86/25 | 0.97 |
| Age (mean ± SD, yr) | 71.9 ± 10.2 | 72.4 ± 10.6 | 0.82 |
| PAD, n (%) | 12 (44.4) | 28 (25.2) | 0.05 |
| CBD diameter (mean ± SD, cm) | 1.5 ± 0.6 | 1.4 ± 0.4 | 0.29 |
| CBD diameter ≥ 1.2 cm, n (%) | 27 (100.0) | 83 (74.8) | < 0.01 |
| CBD diameter ≥ 1.5 cm, n (%) | 23 (85.2) | 50 (45.0) | < 0.01 |
| Largest CBD stone diameter ≥ 1.2 cm, n (%) | 14 (51.9) | 54 (48.6) | 0.77 |
| CBD stone number ≥ 2, n (%) | 13 (48.1) | 43 (38.7) | 0.37 |
| Muddy stones, n (%) | 4 (14.8) | 16 (14.4) | 1.00 |
| Initial ampullary intervention, n (%) | |||
| EST | 2 (7.4) | 6 (5.4) | 1.00 |
| EPBD/EPLBD | 15 (55.6) | 64 (57.7) | 0.84 |
| ESBD | 6 (22.2) | 22 (19.8) | 0.78 |
| CBD morphology, n (%) | < 0.01 | ||
| Straight type | 4 (14.8) | 65 (58.6) | |
| S type | 12 (44.4) | 10 (9.0) | |
| Polyline type | 11 (40.7) | 36 (32.4) | |
| Cholecystectomy, n (%) | 3 (11.1) | 5 (4.5) | 0.39 |
| Procedure time (mean ± SD, min) | 44.9 ± 22.7 | 36.7 ± 18.4 | 0.05 |
Characteristics in patients with different CBD morphologies are shown in Table 3. Approximately 50.0% of CBDs were diagnosed as straight type, 15.9% as S type, and 34.1% as polyline type. CBD diameter (P < 0.01) and CBD diameter ≥ 1.2 cm (P < 0.01) differed significantly among different CBD morphologies. The CBD diameter in patients with S type was 1.8 ± 0.6 cm, which was larger than that in patients with straight type (1.5 ± 0.5 cm). And the patients with a CBD diameter ≥ 1.2 cm in the S type, straight type, and polyline type accounted for 100.0%, 71.0%, and 83.0%, respectively. Other factors showed no significant difference.
| Straight type (n = 69) | S type (n = 22) | Polyline type (n = 47) | P value | |
| Sex (male/female) | 49/20 | 18/4 | 40/7 | 0.19 |
| Age (mean ± SD, yr) | 72.6 ± 10.9 | 71.8 ± 10.6 | 72.0 ± 10.0 | 0.93 |
| PAD: n (%) | 20 (29.0) | 9 (40.9) | 11 (23.4) | 0.33 |
| CBD diameter (mean ± SD, cm) | 1.5 ± 0.5 | 1.8 ± 0.6 | 1.6 ± 0.5 | < 0.01 |
| CBD diameter ≥ 1.2 cm, n (%) | 49 (71.0) | 22 (100.0) | 39 (83.0) | < 0.01 |
| CBD diameter ≥ 1.5 cm, n (%) | 32 (46.4) | 16 (72.7) | 25 (53.2) | 0.10 |
| Largest CBD stone diameter ≥ 1.2 cm, n (%) | 32 (46.4) | 10 (45.5) | 26 (55.3) | 0.59 |
| CBD stone number ≥ 2, n (%) | 27 (39.1) | 13 (59.1) | 16 (34.0) | 0.13 |
| Muddy stones, n (%) | 12 (17.4) | 2 (9.1) | 6 (12.8) | 0.68 |
| Initial ampullary intervention, n (%) | ||||
| EST | 3 (4.3) | 2 (9.1) | 3 (6.4) | 0.62 |
| EPBD/EPLBD | 39 (56.5) | 14 (63.6) | 26 (55.3) | 0.80 |
| ESBD | 15 (21.7) | 3 (13.6) | 10 (21.3) | 0.78 |
| Cholecystectomy, n (%) | 3 (4.3) | 2 (9.1) | 3 (6.4) | 0.62 |
| Procedure time (mean ± SD, min) | 34.9 ± 15.7 | 49.1 ± 27.8 | 38.4 ± 18.6 | 0.07 |
The numbers of one recurrence and multiple recurrences of CBDS were 20 (14.5%) and 7 (5.1%), respectively. The average number of recurrences in the multiple recurrence group was 3.3, and the maximum was 6. All characteristics about single recurrence and multiple recurrences are shown in Table 4. Muddy stones were relatively more common in patients without recurrence (20.0%) compared to recurrent patients (0.0%). However, due to the small sample size, it did not reach a statistical difference.
| Single recurrence (n = 20) | Multiple recurrences (n = 7) | P value | |
| Sex (male/female) | 15/5 | 6/1 | 1.00 |
| Age (mean ± SD, yr) | 72.7 ± 8.9 | 69.4 ± 13.8 | 0.48 |
| PAD, n (%) | 11 (55.0) | 1 (14.3) | 0.09 |
| CBD diameter (mean ± SD, cm) | 1.9 ± 0.4 | 2.0 ± 0.8 | 0.73 |
| CBD diameter ≥ 1.2 cm, n (%) | 20 (100.0) | 7 (100.0) | |
| CBD diameter ≥ 1.5 cm, n (%) | 18 (90.0) | 5 (71.4) | 0.27 |
| Largest CBD stone diameter ≥ 1.2 cm, n (%) | 9 (45.0) | 5 (71.4) | 0.39 |
| CBD stone number ≥ 2, n (%) | 10 (50.0) | 3 (42.9) | 1.00 |
| Muddy stones, n (%) | 4 (20.0) | 0 (0.0) | 0.55 |
| Initial ampullary intervention, n (%) | |||
| EST | 2 (10.0) | 0 (0.0) | 1.00 |
| EPBD/EPLBD | 11 (55.0) | 4 (57.1) | 1.00 |
| ESBD | 4 (20.0) | 2 (28.6) | 0.63 |
| CBD morphology, n (%) | 1.00 | ||
| Straight type | 3 (15.0) | 1 (14.3) | |
| S type | 9 (45.0) | 3 (42.9) | |
| Polyline type | 8 (40.0) | 3 (42.9) | |
| Cholecystectomy, n (%) | 3 (15.0) | 0 (0.0) | 0.55 |
| Procedure time (mean ± SD, min) | 45.8 ± 17.0 | 42.4 ± 36.0 | 0.82 |
| Follow-up period (mean ± SD, yr) | 19.0 ± 10.6 | 20.1 ± 7.7 | 0.80 |
In univariate analysis, CBD diameter ≥ 1.2 cm (P < 0.01), CBD diameter ≥ 1.5 cm (P < 0.01), and CBD morphology (P < 0.01) were associated with CBD stone recurrence (Table 2).
According to multicollinearity analysis, we reported variance inflation factors (VIFs) among CBD diameter, CBD diameter ≥ 1.2 cm, CBD diameter ≥ 1.5 cm, and CBD morphology (VIF < 5). In multivariate analysis, CBD morphology (P < 0.01) and CBD diameter ≥ 1.5 cm (odds ratio [OR] = 6.15, 95% confidence interval [CI]: 1.87-20.24, P < 0.01) were the two independent risk factors. Furthermore, the recurrence rate of patients with S type was 16.79 times that of patients with straight type (OR = 16.79, 95%CI: 4.26-66.09, P < 0.01); the recurrence rate of patients with polyline type was 4.97 times that of patients with straight type (OR = 4.97, 95%CI: 1.42-17.38, P = 0.01); the recurrence rate of S type patients was 3.38 times that of patients with polyline type (OR = 3.38, 95%CI: 1.07-10.72, P = 0.04) (Table 5).
| Factor | β | OR (95%CI) | P value | β | OR (95%CI) | P value |
| PAD | 0.55 | 1.74 (0.61-4.95) | 0.30 | |||
| Procedure time | 0.01 | 1.01 (0.98-1.03) | 0.84 | |||
| CBD diameter ≥ 1.5 cm | 1.82 | 6.15 (1.87-20.24) | < 0.01 | |||
| Model 1 | Model 2 | |||||
| CBD morphology | < 0.01 | < 0.01 | ||||
| Straight type | Reference | -1.60 | 0.20 (0.06-0.70) | 0.01 | ||
| S type | 2.82 | 16.79 (4.27-66.09) | < 0.01 | 1.22 | 3.38 (1.07-10.72) | 0.04 |
| Polyline type | 1.60 | 4.97 (1.42-17.38) | 0.01 | Reference |
ERCP for CBD stones removal has always been a challenge in patients with Billroth II anatomy, and altered anatomy increases the difficulty of the operation and the incidence of complications. However, potential factors for CBD stone recurrence have not been thoroughly defined. To date, there has been no report concerning a specific description of CBD morphology and the connection between CBD morphology and CBD stone recurrence. This study investigated whether different shapes of CBD and other factors influence CBD stone recurrence after successful ERCP. Furthermore, this is the first report to introduce the new concept of CBD morphology, which was classified into straight type, S type, and polyline type.
In multivariate analysis, CBD morphology and CBD diameter ≥ 1.5 cm were the two independent risk factors for the recurrence of CBD stones in Billroth II anatomy patients. More specifically, the recurrence rate of patients with S type was higher than that of patients other types. As reported, bile stasis is an essential factor in the pathogenesis of CBD stones, which can also contribute to CBD infections[17]. Beta-glucuronidase changes bilirubin hydrolysis to nonconjugated, and calcium combines with nonconjugated bilirubin easily, which promotes bilirubin calcium formation and stone recurrence[18].
Different shapes of the CBD enter the duodenum at different angles. The straight type CBD enters the duodenum at an acute angle, while the S type and polyline type angles are close to a right angle. Due to the dysfunction of the sphincter of Oddi, CBD that enters the duodenum at a right angle is more prone to intestinal fluid reflux. Because intestinal fluid contains digestive juices, food residues, and a large number of bacteria, once reflux occurs, it causes the bile duct loop change and predisposes to bile duct infection[19].
Kim et al[20] suggested that complete endoscopic removal of CBD stones is associated with CBD angulation. From the observation, we might hypothesize that CBD morphology, particularly S type and polyline type, is the specific contribution factor affecting technical difficulty and complete CBD stones removal. Apparently, incomplete endoscopic removal can induce CBD stone recurrence.
Some prospective studies indicated that CBD diameter could predict the further recurrence of stones[11,21,22]. And they assumed that a dilated CBD could promote the formation of stone because of bacterial contamination and bile stasis. In our study, CBD diameter ≥ 1.5 cm was the independent risk factor of recurrence, which supported the assumption.
Our study noted that the presence of PAD was not an independent risk factor for the recurrence of CBD stones in multivariate analysis. PAD is known to induce functional biliary stasis because of inducing reflux of duodenal contents or compression of the distal CBD[23]. However, the effect of PAD on bile stasis is thought to disappear after ampullary interventions such as EST; PAD may not induce the CBD stone recurrence.
By analyzing the procedure time of patients with successful stone removal, we noted that the average procedure time of S type patients was significantly longer than that of the other two groups. However, it did not reach a statistical difference. According to the result, we considered the hypothesis that CBD morphology is a predictive factor for successful CBD stone removal, difficult endoscopic operation, and complications. Starting from this point, we investigated the detailed association between CBD morphology and endoscopic therapy.
Different initial ampullary interventions have different effects on the outcome and complications of CBD stones extraction[24-28]. The differences in the initial ampullary intervention (EST, EPBD/EPLBD, and ESBD) were not statistically significant in our study. Our research was probably limited by the small sample size. Therefore, a prospective study with a large sample size may be recommended to determine the appropriate ampullary intervention in patients with different CBD morphologies.
Although we cannot change the shape of CBD by surgery or ERCP, prophylactic therapy may be effective in preventing the recurrence of CBD stones. Ursodeoxycholic acid (UDCA) is known to improve bile excretion, and may suppress the CBD stone recurrence by improving cholestasis. Some studies reveal that UDCA facilitates the extraction of CBD stones or effectively reduces the diameter of stones[29,30]. According to the report that excluded patients after gastrectomy by Yamamoto et al[31], UDCA may be a therapeutic option to prevent CBD stone recurrence. Moreover, UDCA treatment for 6 mo after LSG effectively prevents cholelithiasis[32-34]. However, some studies did not recommend the use of UDCA to prevent CBD stone recurrence[12,35]. Therefore, further exploration of UDCA with a more significant number of subjects will be required in the future.
Most studies advocated that a sharply angulated bile duct might induce bile stasis and predict recurrent CBD stones. Seo et al[36] reported that the average bile duct angle in the recurrence group was 268.3°, and bile duct angulation was the independent predictor of CBD stone recurrence, while Zhang et al[16] reported that it was bile duct angulation (≤ 135°). It is challenging to define and measure sharp bile duct angulation specifically. However, measurement at ERCP of bile duct angulation is simple without any risk or additional procedure.
In the current study, the assessment of CBD morphology was on a two-dimensional plane. Compared with a more accurate three-dimensional plane, this actually may lead to bias[20]. In our study, the patients were placed in the left lateral decubitus position to eliminate bias regarding position change. The accuracy of CBD morphology assessment could be improved in future prospective studies.
The present study was limited by its small sample size and retrospective nature. The observation that there was no significant difference between single recurrence and multiple recurrences may be related to the small sample size.
In conclusion, ERCP in unique shapes of CBD, such as S type and polyline type, is challenging and requires careful assessment and other treatment options before the endoscopic procedure. CBD morphology of S type and polyline type should be regarded as a high risk factor for stone recurrence. It is beneficial to identify Billroth II anatomy patients for preventing serious complications, such as CBD stones.
Endoscopic retrograde cholangiopancreatography (ERCP) is the first choice for removing common bile duct (CBD) stones in Billroth II anatomy patients. The risk factors for CBD stone recurrence after ERCP have been discussed for many years. However, CBD morphology had never been noticed as a potential risk factor.
Our study introduced the new concept of CBD morphology on the cholangiogram and classified it into straight type, S type, and polyline type.
The objective of this study was to evaluate CBD morphology and other predictors affecting CBD stone recurrence in Billroth II gastrectomy patients.
We performed a retrospective case-control analysis of CBD stones patients with a history of Billroth II gastrectomy, and there were 138 patients who underwent therapeutic ERCP at our center from January 2011 to October 2020. We examined the possible predictors of CBD stone recurrence by univariate analysis and multivariate logistic regression analysis.
CBD morphology (P < 0.01) and CBD diameter ≥ 1.5 cm (odds ratio [OR] = 6.15, 95% confidence interval [CI]: 1.87-20.24, P < 0.01) were the two independent risk factors. Patient characteristics were not statistically significant between the recurrence and non-recurrence groups, which included age, sex, CBD diameter, largest CBD stone diameter ≥ 1.2 cm, CBD stone number ≥ 2, muddy stones, initial ampullary intervention (EST, EPBD/EPLBD, and ESBD) and cholecystectomy. In multivariate analysis, the recurrence rate of patients with S type was 16.79 times that of patients with straight type (OR = 16.79, 95%CI: 4.26-66.09, P < 0.01), the recurrence rate of patients with polyline type was 4.97 times that of patients with straight type (OR = 4.97, 95%CI: 1.42-17.38, P = 0.01), and the recurrence rate of S type patients was 3.38 times that of patients with polyline type (OR = 3.38, 95%CI: 1.07-10.72, P = 0.04).
CBD morphology, especially S type and polyline type, is associated with increased recurrence of CBD stones in Billroth II anatomy patients.
Future research with more samples should be undertaken to assess the association between CBD morphology and CBD stone recurrence in patients with or without Billroth II gastrectomy. And periodic surveillance and standard prophylactic therapy should be explored.
We thank all medical staff and technicians of digestive endoscopy center who participated in this study.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Gonoi W, Kao JT, Paik WH S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 118] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 84] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1716] [Cited by in F6Publishing: 1607] [Article Influence: 57.4] [Reference Citation Analysis (2)] |
| 4. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 158] [Cited by in F6Publishing: 170] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 5. | Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 120] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, Park HJ, Joo YH, Yoo KS, Kim HJ, Min YI. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 95] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Keizman D, Ish Shalom M, Konikoff FM. Recurrent symptomatic common bile duct stones after endoscopic stone extraction in elderly patients. Gastrointest Endosc. 2006;64:60-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763-2767. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 109] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Kawaji Y, Isayama H, Nakai Y, Saito K, Sato T, Hakuta R, Saito T, Takahara N, Mizuno S, Kogure H, Matsubara S, Tada M, Kitano M, Koike K. Multiple recurrences after endoscopic removal of common bile duct stones: A retrospective analysis of 976 cases. J Gastroenterol Hepatol. 2019;34:1460-1466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Bove V, Tringali A, Familiari P, Gigante G, Boškoski I, Perri V, Mutignani M, Costamagna G. ERCP in patients with prior Billroth II gastrectomy: report of 30 years' experience. Endoscopy. 2015;47:611-616. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 11. | Kim KH, Rhu JH, Kim TN. Recurrence of bile duct stones after endoscopic papillary large balloon dilation combined with limited sphincterotomy: long-term follow-up study. Gut Liver. 2012;6:107-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 238] [Cited by in F6Publishing: 286] [Article Influence: 57.2] [Reference Citation Analysis (0)] |
| 13. | Zhou XD, Chen QF, Zhang YY, Yu MJ, Zhong C, Liu ZJ, Li GH, Zhou XJ, Hong JB, Chen YX. Outcomes of endoscopic sphincterotomy vs open choledochotomy for common bile duct stones. World J Gastroenterol. 2019;25:485-497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 16] [Cited by in F6Publishing: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Xu XD, Chen B, Dai JJ, Qian JQ, Xu CF. Minor endoscopic sphincterotomy followed by large balloon dilation for large choledocholith treatment. World J Gastroenterol. 2017;23:5739-5745. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 8] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Zhao HC, He L, Zhou DC, Geng XP, Pan FM. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J Gastroenterol. 2013;19:3883-3891. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 50] [Cited by in F6Publishing: 48] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 16. | Zhang R, Luo H, Pan Y, Zhao L, Dong J, Liu Z, Wang X, Tao Q, Lu G, Guo X. Rate of duodenal-biliary reflux increases in patients with recurrent common bile duct stones: evidence from barium meal examination. Gastrointest Endosc. 2015;82:660-665. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Kullman E, Borch K, Lindström E, Anséhn S, Ihse I, Anderberg B. Bacteremia following diagnostic and therapeutic ERCP. Gastrointest Endosc. 1992;38:444-449. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 46] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Leung JW, Liu YL, Leung PS, Chan RC, Inciardi JF, Cheng AF. Expression of bacterial beta-glucuronidase in human bile: an in vitro study. Gastrointest Endosc. 2001;54:346-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Zhang Q, Ye M, Su W, Chen Y, Lou Y, Yang J, Ma T, Chen W, Gao S, Que R, Zhang B, Li H, Bai X, Liang T. Sphincter of Oddi laxity alters bile duct microbiota and contributes to the recurrence of choledocholithiasis. Ann Transl Med. 2020;8:1383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Kim HJ, Choi HS, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Choi SH. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66:1154-1160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 21. | Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002;34:273-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 22. | Ohashi A, Tamada K, Wada S, Hatanaka H, Tomiyama T, Tano S, Nakazawa K, Sugano K. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009;21:73-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Kim MH, Myung SJ, Seo DW, Lee SK, Kim YS, Lee MH, Yoo BM, Min MI. Association of periampullary diverticula with primary choledocholithiasis but not with secondary choledocholithiasis. Endoscopy. 1998;30:601-604. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 290] [Cited by in F6Publishing: 298] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 25. | Carr-Locke DL. Difficult bile-duct stones: cut, dilate, or both? Gastrointest Endosc. 2008;67:1053-1055. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Karsenti D, Coron E, Vanbiervliet G, Privat J, Kull E, Bichard P, Perrot B, Quentin V, Duriez A, Cholet F, Subtil C, Duchmann JC, Lefort C, Hudziak H, Koch S, Granval P, Lecleire S, Charachon A, Barange K, Cesbron EM, De Widerspach A, Le Baleur Y, Barthet M, Poincloux L. Complete endoscopic sphincterotomy with vs without large-balloon dilation for the removal of large bile duct stones: randomized multicenter study. Endoscopy. 2017;49:968-976. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 27. | Jin PP, Cheng JF, Liu D, Mei M, Xu ZQ, Sun LM. Endoscopic papillary large balloon dilation vs endoscopic sphincterotomy for retrieval of common bile duct stones: a meta-analysis. World J Gastroenterol. 2014;20:5548-5556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 40] [Cited by in F6Publishing: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 28. | Park CH, Jung JH, Nam E, Kim EH, Kim MG, Kim JH, Park SW. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc. 2018;87:43-57.e10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 29. | Chang HY, Wang CJ, Liu B, Wang YZ, Wang WJ, Wang W, Li D, Li YL. Ursodeoxycholic acid combined with percutaneous transhepatic balloon dilation for management of gallstones after elimination of common bile duct stones. World J Gastroenterol. 2018;24:4489-4498. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Johnson GK, Geenen JE, Venu RP, Schmalz MJ, Hogan WJ. Treatment of non-extractable common bile duct stones with combination ursodeoxycholic acid plus endoprostheses. Gastrointest Endosc. 1993;39:528-531. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Yamamoto R, Tazuma S, Kanno K, Igarashi Y, Inui K, Ohara H, Tsuyuguchi T, Ryozawa S. Ursodeoxycholic acid after bile duct stone removal and risk factors for recurrence: a randomized trial. J Hepatobiliary Pancreat Sci. 2016;23:132-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Coupaye M, Calabrese D, Sami O, Siauve N, Ledoux S. Effectiveness of Ursodeoxycholic Acid in the Prevention of Cholelithiasis After Sleeve Gastrectomy. Obes Surg. 2019;29:2464-2469. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Nabil TM, Khalil AH, Gamal K. Effect of oral ursodeoxycholic acid on cholelithiasis following laparoscopic sleeve gastrectomy for morbid obesity. Surg Obes Relat Dis. 2019;15:827-831. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 34. | Adams LB, Chang C, Pope J, Kim Y, Liu P, Yates A. Randomized, Prospective Comparison of Ursodeoxycholic Acid for the Prevention of Gallstones after Sleeve Gastrectomy. Obes Surg. 2016;26:990-994. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 35. | Cheon YK, Lehman GA. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006;18:461-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Seo DB, Bang BW, Jeong S, Lee DH, Park SG, Jeon YS, Lee JI, Lee JW. Does the bile duct angulation affect recurrence of choledocholithiasis? World J Gastroenterol. 2011;17:4118-4123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |