Published online Jul 26, 2021. doi: 10.12998/wjcc.v9.i21.6005
Peer-review started: January 26, 2021
First decision: April 29, 2021
Revised: May 7, 2021
Accepted: June 3, 2021
Article in press: June 3, 2021
Published online: July 26, 2021
Isolated fungus ball (FB) in a single cell of the left ethmoid roof is a very rare condition.
We report the case of a 51-year-old female patient whose computed tomography presented a soft tissue mass filling in the left ethmoid roof cell. The patient did not complain of any specific sinonasal symptoms, such as nasal discharge, nasal obstruction, and loss of smell, apart from headache in the left retro-orbital region.
The patient underwent functional endoscopic sinus surgery under general anesthesia, and the inflammatory material collected was histologically diagnosed as a rare case of a FB in a single cell of the left ethmoid roof.
Core Tip: In this case, preoperative computed tomography did not lead to the correct diagnosis, which showed a round soft tissue mass in the left ethmoid sinus without any calcification. Functional endoscopic sinus surgery in the patient revealed cheesy, clay-like material that was highly suggestive of a fungus ball (FB). The histological investigation confirmed the accurate diagnosis; however, negative results were obtained from FB cultures.
- Citation: Zhou LQ, Li M, Li YQ, Wang YJ. Isolated fungus ball in a single cell of the left ethmoid roof: A case report. World J Clin Cases 2021; 9(21): 6005-6008
- URL: https://www.wjgnet.com/2307-8960/full/v9/i21/6005.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i21.6005
Although rare, diagnoses of fungal infections of the paranasal sinuses have been increasing in the past two decades. This is mainly due to refinements in radiologic evaluation, fungal culture techniques, and surgical technology. Fungal infections can be roughly divided into two types: Invasive and noninvasive fungal rhinosinusitis[1]. The invasive form is distinguished from the noninvasive variety depending on the presence of microscopic evidence of tissue invasion through the epithelium. Fungus ball (FB) and eosinophilic localizations (allergic fungal sinusitis and eosinophilic fungal sinusitis) are forms of chronic, noninvasive fungal infection[1,2].
Immunocompetent patients are most susceptible to FB of the paranasal sinuses especially middle-aged females[3]. The mechanism of FB infection is largely unknown, although there are several hypotheses, including environmental factors, changes in air flow resistance in the nasal cavity, and anatomic structural variations in the nasal cavity. FB usually only appears in one sinus, most commonly in the maxillary sinus (94%), with the majority of the remaining cases occurring in the sphenoid. Single-cell ethmoid sinus involvement is very rare in paranasal sinus FB cases[4]. The most commonly encountered fungus is Aspergillus species, though other pathogens such as Mucor, Alternaria, and Bipolaris have also been detected[5].
The ethmoid cells are divided into anterior ethmoid cells and posterior ethmoid cells. Anterior ethmoid cells empty into the middle meatus while posterior ethmoid cells empty into the superior meatus. The ethmoid roof cell is one of the posterior ethmoid cells which empty into the superior meatus, and it is clinically significant as its superior boundary is the skull base (ethmoid roof). Hence, we name the cell as ethmoid roof cell, which is one of the posterior ethmoid cells that is connected to the ethmoid roof.
A 51-year-old woman with headache in the left retro-orbital region as first symptom was referred to the Department of Otolaryngology of Wuhan Union Hospital. Her headache had worsened progressively over 1 year.
The patient had taken medication that was prescribed at a local clinic for 3 mo, but her condition did not relieve.
The patient did not complain of any specific sinonasal symptoms, such as nasal discharge, nasal obstruction, and loss of smell apart from headache.
The patient denied any history of underlying systemic disease, dental surgery, facial trauma, or previous sinus surgery.
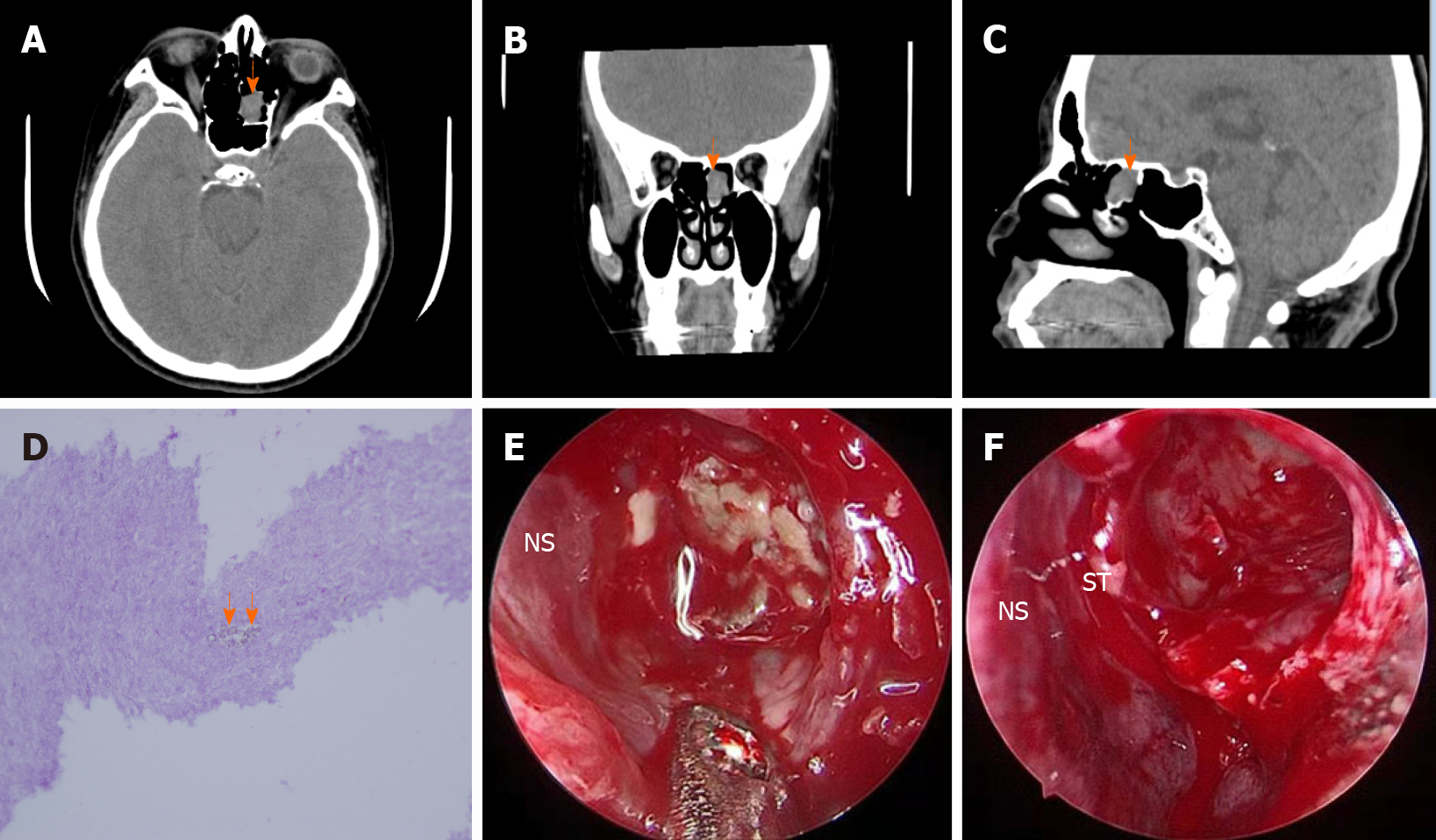
The patient underwent brain computed tomography (CT), which showed no significant alterations in brain tissue; instead, a round soft tissue mass in the left ethmoid roof cell was observed (Figure 1).
The patient underwent brain CT, which showed a round soft tissue mass in the left ethmoid roof cell with no significant alterations in brain tissue (Figure 1).
The accurate diagnosis of left ethmoid sinus FB was confirmed by histopathological examination.
The patient underwent functional endoscopic sinus surgery (FESS). After opening the left ethmoid roof cell, a cheesy, clay-like material which was highly suggestive of an FB was observed.
The patient’s headache was relieved gradually after surgery.
The diagnosis of FB is usually delayed due to the nonspecific and asymptomatic presentation of FB[6]. Therefore, it is often encountered as a part of the investigation of and treatment for chronic sinusitis. Nonspecific chronic inflammatory changes without tissue invasion by the fungi may be observed by endoscopic examination of the nasal cavity examination[7].
CT and magnetic resonance imaging (MRI) examinations are both reliable tools for the diagnosis and preoperative and postoperative evaluations of sinonasal FB. On CT scan, typical FB is usually limited to a single sinus which appears as a hyperdense mass with linear or punctuate central calcifications. On MRI, the FB demonstrates an intermediate to hypointense signal on T1-weighted images, while T2-weighted images show an isointense or hypointense signal, or even no signal, while areas of T2 low signal may be caused by calcification and paramagnetic substances[7,8]. The cost of MRI is much higher than that of CT scans; hence, CT scanning is the most preferred choice, and MRI can be used to augment CT scans. FESS can be considered the most useful treatment for FB, and the recurrence rate is very low. It is important to completely eliminate the FB and reestablish ventilation together with draining of the sinus to its natural ostium during surgery. Histopathology plays a key role in the identification of tissue invaded by the fungi.
In this case, preoperative CT scan showed a round soft tissue mass in the left ethmoid sinus without any calcification, which did not lead to the correct diagnosis. The patients revealed cheesy, clay-like material that was highly suggestive of an FB in the FESS. The histological investigation confirmed the accurate diagnosis as FB; however, negative results were obtained from FB cultures. It is reported that only 23%-50% of FB cultures are positive according to the literature.
Manuscript source: Unsolicited manuscript
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abdullah B, Lobo D, Unal M S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997;337:254-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 303] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Hora JF. Primary aspergillosis of the paranasal sinuses and associated areas. Laryngoscope. 1965;75:768-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 128] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Lop-Gros J, Gras-Cabrerizo JR, Bothe-González C, Montserrat-Gili JR, Sumarroca-Trouboul A, Massegur-Solench H. Fungus ball of the paranasal sinuses: Analysis of our serie of patients. Acta Otorrinolaringol Esp. 2016;67:220-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Karkas A, Klossek JM. Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology. 2005;43:34-39. [PubMed] [Cited in This Article: ] |
| 5. | Ferguson BJ. Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am. 2000;33:389-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Grosjean P, Weber R. Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol. 2007;264:461-470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 7. | Zinreich SJ, Kennedy DW, Malat J, Curtin HD, Epstein JI, Huff LC, Kumar AJ, Johns ME, Rosenbaum AE. Fungal sinusitis: diagnosis with CT and MR imaging. Radiology. 1988;169:439-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 323] [Cited by in F6Publishing: 335] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Seo YJ, Kim J, Kim K, Lee JG, Kim CH, Yoon JH. Radiologic characteristics of sinonasal fungus ball: an analysis of 119 cases. Acta Radiol. 2011;52:790-795. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |