Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.2988
Peer-review started: March 6, 2020
First decision: April 12, 2020
Revised: May 26, 2020
Accepted: June 19, 2020
Article in press: June 19, 2020
Published online: July 26, 2020
Endoscopic retrograde cholangiopancreatography (ERCP) is a valuable therapeutic technique for pancreatobiliary diseases, and its application in the elderly is no longer limited. However, a higher incidence of procedure difficulty and periprocedural adverse events might be expected in elderly patients due to the presence of other medical disorders and the poor general condition of this population.
To evaluate the incidence, causes, and management of difficult biliary cannulation during ERCP in elderly patients and the role of difficult cannulation as a risk factor for adverse events.
A total of 614 patients who underwent ERCP during the study period were prospectively studied and divided into two groups based on their age. One hundred and forty-six patients were aged 80 years or older and 468 patients were aged less than 80 years. The primary outcome measurements were cannulation difficulty, cannulation success rate, ERCP procedure time, and related adverse events.
There was no difference in the incidence of difficult cannulation among the two groups (32.9% vs 34.4%, P = 0.765), as well as in the cannulation success rate (96.6% vs 96.8%, P = 0.54). The cannulation techniques were shown to be safe and efficient in achieving successful cannulation. Logistic regression analysis showed that patients aged 80 years or older were not associated with increased adverse events; however, difficult cannulation cases [adjusted odds ratio (AOR) = 3.478; 95% confidence interval (CI): 1.877-6.442; P < 0.001] and patients with Charlson Comorbidity Index ≥ 2 (AOR = 1.824; 95%CI: 0.993-3.349; P = 0.045) were more likely to develop adverse events. In contrast, other factors including age ≤ 65 (AOR = 3.460; 95%CI: 1.511-7.922; P = 0.003), female gender (AOR = 2.362; 95%CI=1.089-5.124; P = 0.030), difficult cannulation (AOR = 4.527; 95%CI: 2.078-9.860; P < 0.001), and patients with cholangitis (AOR = 3.261; 95%CI: 1.204-8.832; P = 0.020) were strongly associated with a higher rate of post-ERCP pancreatitis.
Advanced age has not been proved to be a risk factor for difficult cannulation, and secondary cannulation techniques can be safely and efficaciously utilized in this group. Patients with a Charlson Comorbidity Index ≥ 2 and difficult cannulation are associated with an increased overall adverse events rate, while age ≥ 80 years is not.
Core tip: As life expectancy has increased, the application of endoscopic retrograde cholangiopancreatography in the elderly population is no longer limited. This increase may come with more difficulty in biliary cannulation or more related adverse events in senior patients. Little is known about cannulation difficulty grading in the elderly and its relationship with adverse events. Therefore, we aimed to evaluate the risk factors for adverse events in elderly patients with difficult bile duct access.
- Citation: Tabak F, Wang HS, Li QP, Ge XX, Wang F, Ji GZ, Miao L. Endoscopic retrograde cholangiopancreatography in elderly patients: Difficult cannulation and adverse events. World J Clin Cases 2020; 8(14): 2988-2999
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/2988.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.2988
Aging society is becoming a global issue, and in China, the elderly population is growing rapidly. According to China’s National Working Committee on aging, it will take just 20 years to double the proportion of the elderly Chinese population from 10% to 20%. Moreover, by 2050, about a third of the country’s population will be over 60 years, and thereby, the proportion of the elderly population, 80 years of age or more, will also rise. As a result of increased life expectancy, the incidence of choledo-cholithiasis and pancreatobiliary malignancy is increasing in advanced age.
Endoscopic retrograde cholangiopancreatography (ERCP) has become a valuable therapeutic procedure in pancreatobiliary diseases, especially for patients with concomitant diseases, which increase the risk associated with surgery. However, a higher incidence of procedure difficulty and periprocedural adverse events might be expected in elderly patients due to the presence of other medical disorders and the poor general condition of this population. Furthermore, the age-related higher probability of periampullary diverticulum and post-surgical anatomy reconstruction make ERCP a challenging procedure in this group. Therefore, there is a need to assess the possible benefits and risks of ERCP in every elderly patient. A successful ERCP procedure requires deep cannulation of the common bile duct and/or main pancreatic duct via the major duodenal papilla. A recent definition of difficult biliary cannulation was released by the Scandinavian Association for Digestive Endoscopy in 2014 and later confirmed in 2016 by the European Society of Gastrointestinal Endoscopy guidelines. According to these new criteria, biliary cannulation is considered difficult if it lasts longer than 5 min, requires more than five attempts, or the pancreatic duct is cannulated more than twice. The probability of failed biliary cannulation ranges from 5-18% based on the endoscopist’s experience and the center volume. Some studies suggest that a higher number of cannulation attempts leads to a higher incidence of post-ERCP pancreatitis (PEP).
Although multiple studies on the safety of ERCPs in the elderly have been published, not enough studies have focused on difficult cannulation and the safety of different cannulation techniques used in elderly patients.
The first objective of this study was to present a new inclusive study on the age-dependent safety and efficacy of ERCP taking into account the choice of using multiple techniques to accomplish deep cannulation of the common bile duct (CBD). The second objective was to study the influence of cannulation difficulty as a risk factor for adverse events, especially PEP.
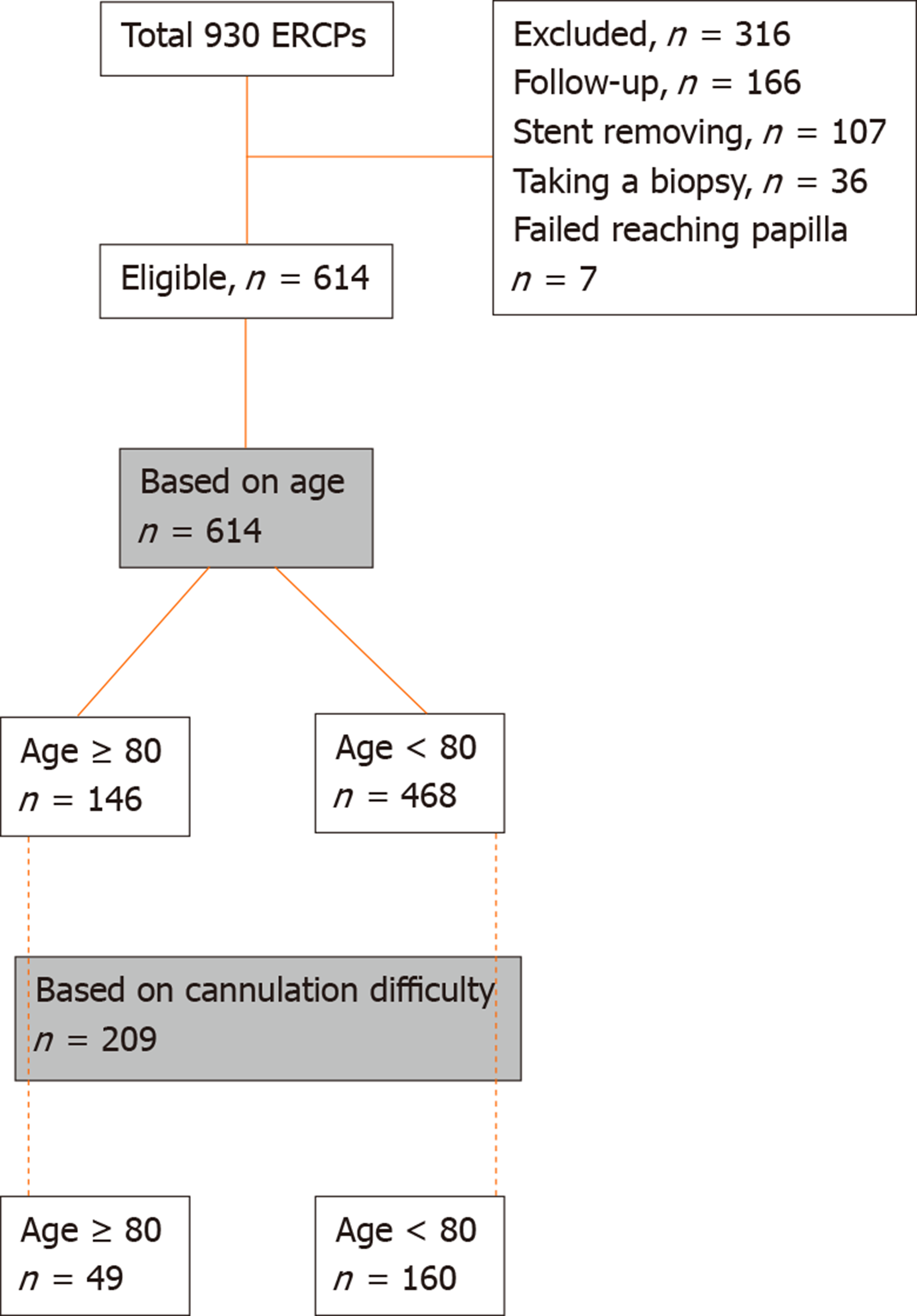
The study protocol was approved by the Institutional Review Board of the Second Affiliated Hospital of Nanjing Medical University. A total of 930 consecutive ERCPs were performed in our endoscopy center between July 2016 and January 2018, and the clinical and therapeutic related data were prospectively collected. Patients with previous sphincterotomy and patients with altered anatomy (Billroth ll, Roux-en-y reconstruction, or duodenum stricture), in whom we could not reach the papilla, were excluded. For the purpose of analysis, a total of 614 patients with a native papilla enrolled in this study were divided into two groups based on their age. Those 614 patients were subsequently filtered based on difficult cannulation grading (Figure 1). All patients signed an informed consent form before ERCP was performed.
Data describing the patients' clinical and therapeutic features, including demographics, comorbid diseases, procedure details, and ERCP-related adverse events, were prospectively collected. Also, the cannulation duration and number of attempts were carefully recorded.
Comorbid diseases were classified as hypertension, cardiac diseases (ischemic heart diseases, heart failure), diabetes mellitus, neurological diseases (cerebrovascular diseases, dementia), hepatic diseases, malignancy, chronic pulmonary diseases, and renal diseases. Additionally, comorbidities were weighted using the Charlson Comorbidity Index (CCI), which is based on varying assigned weights of comorbid conditions depending on the risk of mortality associated with each one. We used the cutoff of CCI ≥ 2 to stratify the patients based on their comorbidities.
Indications were grouped into choledocholithiasis with or without biliary pancreatitis or cholangitis, chronic pancreatitis, benign strictures, and patients with known or suspected cholangiocarcinoma, ampullary or pancreatic carcinoma. Additionally, the second ERCP was performed to complete the clearance of biliary stones, insert or exchange biliary stents.
All patients underwent therapeutic ERCP using a side-view duodenoscope in the prone or left lateral position following overnight fasting. The patients were sedated using intravenous midazolam with adjusted propofol dosage for suitable sedation in advanced age. Patients were monitored continuously during the procedure by an anesthesiologist using a pulse oximeter, electrocardiography monitoring, and supplementary oxygen when needed. Prophylactic octreotide dose was administered to all patients before ERCP for PEP prevention. In addition, prophylactic placement of a pancreatic stent was carried out in patients with difficult cannulation, especially those with multiple pancreatic cannulations. Rectal non-steroidal anti-inflammatory drugs were not administered for the prevention of PEP during the study period.
Standard biliary cannulation was initially performed using a guidewire-assisted technique with a sphincterotome. Needle knife precut (NKP) or transpancreatic sphincterotomy (TPS) were carried out when selective biliary access failed after standard cannulation attempts. Choosing the most suitable secondary cannulation technique was according to the endoscopist’s expertise, which was mainly based on the repetitive unintended guidewire insertion into the pancreatic duct. NKP was considered as the preferred choice in the absence of pancreatic cannulation and in cases with impacted biliary stones at the ampulla or the distal CBD. In cases of prior pancreatic guidewire insertion, TPS was performed with placement of a prophylactic pancreatic stent. It is standard procedure in our hospital, that all patients undergoing ERCP require a three-day hospitalization period for observation and follow-up serum amylase measurement.
Cannulation was considered difficult if it took more than 5 min, needed more than five cannulation attempts in the papilla, or the pancreatic duct was cannulated more than twice. In this study, we used cannulation time scoring to grade cannulation difficulty. Therefore, we considered the cannulation difficulty moderate if cannulation time was 5-10 min and difficult if it took more than 10 min. The most probable causes of difficult cannulation were grouped into periampullary diverticulum, CBD distal stricture, and stone impaction in the distal bile duct. The size of the papilla including small and protruding papilla, in addition to other variant anatomy in the orientation and location of the papilla were reported under the cause of papillary anatomy. Other causes of difficult cannulation were ampullary carcinoma and surgically altered anatomy in which the papilla could not be reached.
PEP was diagnosed when the patient had new or worsened abdominal pain in addition to an elevation in amylase at least three times the upper limit of the normal level, at more than 24 h after ERCP, which required hospitalization extension. Post-procedural bleeding was evidenced by a drop-in hemoglobin > 2 g/dL. Other adverse events, including perforations, cholangitis, and cardiopulmonary events, were defined according to published criteria.
Our sample size was larger than the theoretical sample size estimated by (Gpower 3.1, α 0.05; statistical power 80%; 1:3 allocation ratio, Fisher’s exact test) and could lead to sufficient conclusions. Data are presented in the form of the median, the number of patients, and percentages. The data were analyzed using SPSS version 20 (IBM Corporation, Somers, NY, United States). Differences among different patient cohorts were determined using Fisher’s exact test for categorical variables, and the Mann–Whitney U test for non-categorical variables. Variables of potential significance (P value < 0.10) were entered into a multivariate analysis (logistic regression analysis, enter method). Statistical significance was set at the level of P value < 0.05 (two-sided). Multiple statistical comparisons were performed using multivariate logistic regression analysis (binary logistic regression, enter method).
There were 146 patients (23.8%) aged 80 years or older with a median age of 83 years [interquartile range (IQR): 81-86] and 468 patients (76.2%) younger than 80 years with a median age of 62 years (IQR: 50-71) (Table 1). There was no difference in patient gender between the groups with a comparable male ratio (51.4% vs 53.8%, P = 0.636). The most common indication in both groups was biliary stone disease (82.9% vs 82.3%, P = 0.468); followed by benign biliary stricture (11% vs 13.2%, P = 0.287). The younger group had a higher proportion of patients with cholangitis and gallstone pancreatitis. Also, the older group had a higher proportion of patients undergoing the procedure due to tumors, especially ampullary carcinoma. However, no significant difference was found in the distribution of indications between the two groups. The elderly group was more likely to have comorbid diseases and a significantly higher proportion of patients with CCI ≥ 2 than the younger group (29.5% vs 18.3%, P = 0.005). The elderly group had a significantly higher rate of hypertension (38.4% vs 26.7%, P = 0.009), cardiac diseases (15.1% vs 5.1%, P < 0.001), and cerebrovascular accident (21.9% vs 9.6%, P < 0.001).
| Parameter | Overall (n = 614) | Age ≥ 80 (n = 146) | Age < 80 (n = 468) | P value | |
| Age [median (IQR)] (yr) | 68 (54-79) | 83 (81-86) | 62 (50-71) | ||
| Charlson score [median (IQR)] | 0 (0-1) | 1 (0-2) | 0 (0-1) | 0.001a | |
| Charlson score ≥ 2 | 21% (129) | 29.5% (43) | 18.4% (86) | 0.005b | |
| ERCP procedure time [median (IQR)] (min) | 30 (23-45) | 30 (23-45) | 30 (24-45) | 0.711a | |
| Cannulation time [median (IQR)] (min) | 3.6 (0.8-11.8) | 3.4 (0.8-11.2) | 3.7 (0.8-12) | 0.292a | |
| Male | 53.2% (327) | 51.4% (75) | 53.8% (252) | 0.636b | |
| Cannulation success rate | 96.7% (595) | 96.6% (141) | 96.8% (454) | 0.547b | |
| Indications | |||||
| Biliary stones | 82.4% (506) | 82.9% (121) | 82.3% (385) | 0.468b | |
| Benign strictures | 12.7% (78) | 11% (16) | 13.2% (62) | 0.287b | |
| Cholangiocarcinoma | 4.2% (26) | 4.8% (7) | 4.1% (19) | 0.424b | |
| Cholangitis | 9.1% (56) | 6.8% (10) | 9.8% (46) | 0.180b | |
| Biliary pancreatitis | 5.9% (36) | 4.8% (7) | 6.2% (29) | 0.346b | |
| Chronic pancreatitis | 1.3% (8) | 0% (0) | 1.7% (8) | 0.113b | |
| Ampullary carcinoma | 3.3% (20) | 5.5% (8) | 2.6% (12) | 0.076b | |
| Pancreatic cancer | 3.6% (22) | 2.7% (4) | 3.8% (18) | 0.371b | |
| Comorbidities | |||||
| Hypertension | 29.5% (181) | 38.4% (56) | 26.7% (125) | 0.009b | |
| Cardiac diseases | 7.5% (46) | 15.1% (22) | 5.1% (24) | < 0.001b | |
| Diabetes mellitus | 11.7% (72) | 13% (19) | 11.3% (53) | 0.558b | |
| Neurological diseases | 12.5% (77) | 21.9% (32) | 9.6% (45) | < 0.001b | |
| Hepatic diseases | 7.8% (48) | 5.5% (8) | 8.5% (40) | 0.290b | |
| Malignancy | 9.3% (57) | 11% (16) | 8.8% (41) | 0.256b | |
| Others | 9.9% (61) | 14.4% (21) | 8.5% (40) | 0.031b | |
| Periampullary diverticulum | 19.7% (121) | 29.5% (43) | 16.7% (78) | 0.001b | |
| Cannulation grade of difficulty | |||||
| Easy cannulation | 66% (405) | 67.1% (98) | 65.6% (307) | 0.621b | |
| Moderate cannulation | 11.7% (72) | 10.3% (15) | 12.2% (57) | 0.658b | |
| Difficult cannulation | 22.3% (137) | 22.6% (33) | 22.2% (104) | 0.910b | |
| Second ERCP | 20.4% (125) | 20.5% (30) | 20.3% (95) | 0.512b | |
| Adverse events | 9.8% (60) | 13% (19) | 8.8% (41) | 0.089b | |
| PEP | 5.2% (32) | 2.7% (4) | 6% (28) | 0.088b | |
| Perforation | 0.5% (3) | 0.7% (1) | 0.4% (2) | 0.557b | |
| Bleeding | 1.9% (12) | 4.1% (6) | 1.3% (6) | 0.111b | |
| Cholangitis | 0.6% (4) | 0.7% (1) | 0.6% (3) | 0.663b | |
| Cardiopulmonary | 0.6% (4) | 0.7% (1) | 0.6% (3) | 0.443b | |
| Duration of hospitalization [median (IQR)] (d) | 9 (6-13) | 9 (7-13) | 9 (6-13) | 0.208a | |
| Pancreatic stent | 10.4% (64) | 7.5% (11) | 11.3% (53) | 0.124b | |
| Anti-thrombotic drug | 5.5% (34) | 7.5% (11) | 4.9% (23) | < 0.001b | |
There were no significant differences in the cannulation success rate, cannulation, and ERCP procedure time between the two groups. The median cannulation time was 3.6 min [3.4 (0.8-11.2) vs 3.7 (0.8-12), P = 0.292], and the median ERCP procedure time was 30 min [30 (23-45) vs 30 (24-45), P = 0.711). The frequency of the second ERCP for therapy completion was the same in both groups (20.5% vs 20.3%, P = 0.512).
As expected, the elderly group had a higher prevalence of periampullary diverticulum (29.5% vs 16.7%, P = 0.001). However, cannulation difficulty grading was not significantly different between the groups; easy cannulation (67.1% vs 65.6%, P = 0.621); moderate difficulty of cannulation (10.3% vs 12.2%, P = 0.658); and difficult cannulation (22.6% vs 22.2%, P = 0.910).
PEP was the most frequent adverse event in both groups with a lower incidence in the elderly patient group without a significant difference (2.7% vs 6%, P = 0.088). Most patients in both groups were diagnosed with mild pancreatitis; only two cases of moderate pancreatitis developed in the younger group, and all patients were treated conservatively. Cardiopulmonary events and hypoxia were not significantly different in the two groups (0.7% vs 0.6%, P = 0.443). Patients with ERCP-related bleeding were managed with endoscopic submucosal injection of saline-epinephrine and/or placement of hemostatic clips, and blood transfusion when needed with no requirement for surgical intervention. There was no significant difference in the bleeding rate between the two groups, although there was a higher rate in elderly patients (4.1% vs 1.3%, P = 0.111). This may have been due to the frequent use of antithrombotic drugs in the older group (7.5% vs 4.9%, P < 0.001). In our sample, two patients had a perforation, one in each group with no significant difference (0.7% vs 0.4%, P = 0.557). These patients were identified immediately at the time of ERCP and treated conservatively, and required more than nine days of hospitalization with no need for surgical intervention. Hospitalization duration was similar in both groups, and no procedure-related deaths were recorded during the study period.
Considering the cannulation difficulty grading, 209 patients had moderate or difficult cannulation, including 49 patients (23.4%) 80 years of age or more (Table 2). The presence of periampullary diverticulum was significantly higher in the elderly group and was the most common cause of difficult cannulation in this group (26.5% vs 15.6% P = 0.047). Also, ampullary carcinoma was noted to be a significant cause of difficult cannulation in the elderly group (14.3% vs 1.9%, P = 0.001). In contrast, distal stricture or impacted stone was the most frequent cause of difficult cannulation in younger patients, but the difference was not statistically significant (22.4% vs 35.6%, P = 0.108). The second most common cause in the younger group was papillary anatomy, with a significant difference among the two groups (18.4% vs 35%, P = 0.029). NKP was the most common cannulation technique used in the elderly group for difficult cannulation cases (42.8% vs 36.2%, P = 0.239) followed by guidewire-assisted technique (38.7% vs 42.5%, P = 0.743) and TPS (16.7% vs 21.2%, P = 0.546). No significant difference was noted in the rate of techniques used between the two groups as well as the rate of pancreatic stent placement in difficult cannulation cases (22.9% vs 28.1%, P = 0.489).
| Overall (n = 209), % | Age ≥ 80 (n = 49),% | Age < 80 (n = 160), % | P value1 | |
| Causes of difficulty | ||||
| Papillary anatomy | 31.1 (65) | 18.4 (9) | 35 (56) | 0.029 |
| Distal stricture or impacted stone | 32.5 (68) | 22.4 (11) | 35.6 (57) | 0.108 |
| Diverticulum | 18.2 (38) | 26.5 (13) | 15.6 (25) | 0.047 |
| Ampullary carcinoma | 4.8 (10) | 14.3 (7) | 1.9 (3) | 0.001 |
| Altered anatomy | 8.6 (18) | 10.2 (5) | 8.1 (13) | 0.326 |
| Cannulation failure | 5.7 (12) | 8.3 (4) | 5 (8) | 0.286 |
| Cannulation techniques | ||||
| Guidewire assisted | 42.1 (88) | 40.8 (20) | 42.5 (68) | 0.868 |
| NKP | 37.7 (79) | 42.8 (21) | 36.2 (58) | 0.239 |
| TPS | 20.1 (42) | 16.7 (8) | 21.2 (34) | 0.546 |
| Pancreatic stent | 26.8 (56) | 22.9 (11) | 28.1 (45) | 0.489 |
| Adverse events | ||||
| PEP | 10 (21) | 4.2 (2) | 11.8 (19) | 0.096 |
| Perforation | 1 (2) | 2.1 (1) | 0.6 (1) | 0.407 |
| Bleeding | 1.9 (4) | 4.2 (2) | 1.2 (2) | 0.227 |
| Cholangitis | 1.9 (4) | 2.1 (1) | 1.9 (3) | 0.651 |
| Cardiopulmonary | 1 (2) | - (0) | 1.2 (2) | 0.593 |
With regard to the safety of cannulation techniques in the elderly group, Table 3 shows that there was no significant difference in the incidence of overall adverse events using different cannulation techniques. Furthermore, there were no PEP cases in elderly patients who received NKP or TPS, while PEP developed in two cases after repeating the standard cannulation using the guidewire.
| Guidewire | NKP | TPS | P value1 | |
| Adverse events | n = 20 | n = 21 | n = 8 | |
| PEP | 10% (2) | - (0) | - (0) | 0.203 |
| Overall adverse events | 15% (3) | 14.3% (3) | - (0) | 0.129 |
The adverse events multivariate analysis model was created considering age, CCI ≥ 2, indications, difficult cannulation, and cannulation techniques as independent variables (Table 4). Logistic regression analysis showed that age ≥ 80 years was not associated with increased adverse events; however, difficult cannulation (AOR = 3.478) and CCI ≥ 2 (AOR = 1.824) were more likely to result in adverse events when adjusted for the other variables.
| Adjusted odds ratio | 95% Confidence interval | P value | ||
| Lower | Upper | |||
| Adverse events | ||||
| Age ≥ 80 | 1.568 | 0.861 | 2.854 | 0.141 |
| CCI ≥ 2 | 1.824 | 0.993 | 3.349 | 0.045 |
| Difficult cannulation | 3.478 | 1.877 | 6.442 | < 0.001 |
| Ampullary carcinoma | 0.551 | 0.116 | 2.610 | 0.453 |
| NKP | 0.506 | 0.229 | 1.121 | 0.093 |
In the second multivariate model, we studied the risk factors related to PEP, as shown in Table 5. Logistic regression analysis showed that difficult cannulation (AOR = 4.527), age ≤ 65 (AOR = 3.460), cholangitis (AOR = 3.261), and female gender (AOR = 2.362) were strongly associated with increased PEP. However, a CCI ≥ 2 was less likely to be associated with PEP when adjusted for the other variables.
| Adjusted odds ratio | 95% Confidence interval | P value | ||
| Lower | Upper | |||
| PEP | ||||
| Difficult cannulation | 4.527 | 2.078 | 9.860 | < 0.001 |
| Age ≤ 65 yr | 3.460 | 1.511 | 7.922 | 0.003 |
| Female | 2.362 | 1.089 | 5.124 | 0.030 |
| Cholangitis | 3.261 | 1.204 | 8.832 | 0.020 |
| CCI ≥ 2 | 2.253 | 0.923 | 5.497 | 0.074 |
The average life expectancy worldwide continues to increase, resulting in a rising number of elderly individuals aged 80 years and older. This issue is evident in the Chinese population, which will become one of the world’s most aged society in 2030. The risk of choledocholithiasis and pancreatobiliary malignancies increases with advancing age, resulting in the older population requiring more invasive procedures.
Several studies have reported the safety and efficacy of ERCP in elderly patients, although these patients were more likely to have underlying diseases. Comorbid diseases were also more common in this group in our study. In addition, the older group had a higher proportion of patients with a CCI ≥ 2. Biliary stones were the main indication for ERCP in both groups, followed by benign stricture and malignancy. Cholangitis and biliary pancreatitis were more common in younger patients compared to elderly patients. A higher proportion of tumors, especially ampullary carcinoma, was found in older patients as these indications increase with age.
With regard to ERCP outcomes, most previous studies reported similar efficacy of therapeutic ERCP in patients over 80 years of age and younger patients. In the current study, there was no difference in the procedural success rate or the procedure time between the two groups. Although periampullary diverticulum was more common in the elderly, difficult cannulation grading according to the cannulation time, did not show any differences related to age. On the other hand, the causes of difficult cannulation were distributed differently between the two groups. As periampullary diverticula sharply increase with age, this was the leading cause of difficult cannulation in the elderly group. In addition, the higher proportion of tumors in elderly patients, especially ampullary carcinoma, resulted in tumor growth being the most common cause of difficult cannulation compared with the younger group. A lower incidence of benign CBD distal strictures and stone impaction in the elderly might be due to the age-related increase in CBD diameter, which plays a protective role on impaction in some elderly patients. Successful cannulation in difficult cases was achieved in both groups at a similar rate with no significant difference. Different cannulation techniques were effective in achieving successful biliary access in both groups.
Several studies have reported the safety of ERCP in elderly patients, and have found no significant difference in the incidence of ERCP-related adverse events. In our study, we did not find any increased rate of overall adverse events in patients aged ≥ 80 years when compared to younger patients. PEP was the most frequent adverse event in our study, and elderly patients tended to have a lower rate of pancreatitis. Possible reasons for this lower rate include pancreatic fibrosis and atrophy in the elderly, as well as decreased pancreatic enzyme secretion. There was no significant difference in the rates of ERCP-related perforation, cholangitis, and bleeding, although there was a higher rate of bleeding in elderly patients due to the frequent use of antithrombotic drugs.
With regard to the relationship between difficult cannulation techniques and adverse events, many studies have shown an association between the overall rate of adverse events, especially PEP, and repeated initial cannulation attempts or the use of advanced techniques in difficult cases. Our study found that in the elderly group, repeated standard cannulation attempts using a guidewire caused a higher rate of pancreatitis compared with NKP and TPS, but without a significant difference. This result is consistent with some studies in that early precut is associated with a lower incidence of PEP when compared with repeated standard papillary cannulation attempts. The use of TPS resulted in a lower rate of adverse events and can be considered a safe cannulation technique for elderly patients with difficult cannulation.
In terms of the risk factors for adverse events, we did not observe an increase in the odds of adverse events in the elderly group compared to the younger group. However, an increased risk of adverse events was noted with difficult cannulation and a CCI ≥ 2. Four risk factors for PEP were identified in this study: Difficult cannulation, age less than 65 years, cholangitis, and female gender. These results are consistent with previous reports on the safety of ERCP in elderly patients.
The main strength of this study is its prospective nature, and to the best of our knowledge, it is the first prospective study to focus on difficult cannulation and its causes in elderly ERCP patients. There are a few limitations to this study. First, the study was performed at a single center with a limited number of elderly patients. The second limitation is the rarity of specific adverse events, especially PEP, which may affect the results of multivariate analyses.
In conclusion, this study has shown that the prevalence of difficult cannulation in ERCP is not more common in patients over 80 years of age, and the use of different cannulation techniques is well tolerated with a lower rate of PEP compared with younger patients. Although successful cannulation rate and procedure duration in difficult cases were similar in both groups, different causes were found to affect cannulation difficulty in the two groups. Our study demonstrated that age over 80 years is not a risk factor for ERCP-related adverse events. However, difficult cannulation and increasing comorbidities with a CCI ≥ 2 are both significantly associated with overall adverse events.
Endoscopic retrograde cholangiopancreatography (ERCP) is a valuable therapeutic technique for pancreatobiliary diseases, and its application in the elderly is no longer limited. However, a higher incidence of procedure difficulty and periprocedural adverse events might be expected in elderly patients due to the presence of other medical disorders and the poor general condition of this population.
The risk of choledocholithiasis and pancreatobiliary malignancies increases with advancing age, resulting in the older population requiring more invasive procedures. Although several studies on the safety of ERCPs in the elderly have been published, further investigation regarding the association between advanced age and difficult cannulation is required.
The purpose of this study was to investigate the association between the advanced age and difficult cannulation and the efficacy of different cannulation techniques. We also aimed to evaluate the impact of difficult cannulation on the occurrence of ERCP-related adverse events.
Patients who underwent ERCP during the study period were prospectively studied and divided into two groups based on their age. The primary outcome measurements were cannulation difficulty, cannulation success rate, and ERCP procedure time in both groups. Causes of difficult cannulation, cannulation techniques used, and related adverse events were analyzed.
A total of 614 patients who underwent ERCP with a native papilla were included, of whom 146 were aged 80 years or older. The incidence of difficult cannulation and cannulation success rate in elderly patients were comparable to those in younger patients, and secondary cannulation techniques can be safely and efficaciously utilized in this group. In multivariate analyses with adjustment for potential confounders, age greater than 80 years was not associated with an increase in adverse events. However, patients with difficult cannulation and those with a Charlson Comorbidity Index ≥ 2 were more likely to develop adverse events.
The prevalence of difficult biliary cannulation during ERCP is not more common in patients over 80 years of age. Using different cannulation techniques is effective in achieving biliary access in the elderly with a lower rate of post-ERCP pancreatitis compared with younger patients.
This study was performed at a single center with a limited number of elderly patients. Multi-center prospective studies with a large sample of elderly patients are required to evaluate the short-and long-term consequences of difficult cannulation and advanced cannulation techniques.
The authors thank the editors and four reviewers for their valuable comments, which resulted in considerable improvements to our manuscript. Also, the authors thank Dr. Saeed Assani for his professional suggestions.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kitamura K, Logiudice FP, Sugimoto M, Venu R S-Editor: Zhang L L-Editor: Webster JR E-Editor: Wang LL
| 1. | Wei C, Jin-Ju L. Future Population Trends in China: 2005-2050. Available from: https://cn.bing.com/search?q=Future+Population+Trends+in+China&qs=n&form=QBRE&sp=-1&pq=future+population+trends+in+china&sc=0-33&sk=&cvid=9A4A66A2B094409191E0A5D5FF852ED4. [Cited in This Article: ] |
| 2. | Day LW, Lin L, Somsouk M. Adverse events in older patients undergoing ERCP: a systematic review and meta-analysis. Endosc Int Open. 2014;2:E28-E36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 159] [Article Influence: 12.2] [Reference Citation Analysis (1)] |
| 3. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 290] [Cited by in F6Publishing: 298] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 4. | Halttunen J, Meisner S, Aabakken L, Arnelo U, Grönroos J, Hauge T, Kleveland PM, Nordblad Schmidt P, Saarela A, Swahn F, Toth E, Mustonen H, Löhr JM. Difficult cannulation as defined by a prospective study of the Scandinavian Association for Digestive Endoscopy (SADE) in 907 ERCPs. Scand J Gastroenterol. 2014;49:752-758. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 5. | Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, Ryan M, Parker H, Frakes JT, Fogel EL, Silverman WB, Dua KS, Aliperti G, Yakshe P, Uzer M, Jones W, Goff J, Lazzell-Pannell L, Rashdan A, Temkit M, Lehman GA. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139-147. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 414] [Cited by in F6Publishing: 404] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 6. | Nakai Y, Isayama H, Sasahira N, Kogure H, Sasaki T, Yamamoto N, Saito K, Umefune G, Akiyama D, Kawahata S, Matsukawa M, Saito T, Hamada T, Takahara N, Mizuno S, Miyabayashi K, Mohri D, Hirano K, Tada M, Koike K. Risk factors for post-ERCP pancreatitis in wire-guided cannulation for therapeutic biliary ERCP. Gastrointest Endosc. 2015;81:119-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Tumi A, Magadmi M, Elfageih S, Rajab AF, Azzabi M, Elzouki AN. ERCP in a cohort of 759 cases: A 6-year experience of a single tertiary centre in Libya. Arab J Gastroenterol. 2015;16:25-28. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Yang JH, Li W, Si XK, Zhang JX, Cao YJ. Efficacy and Safety of Therapeutic ERCP in the Elderly: A Single Center Experience. Surg Laparosc Endosc Percutan Tech. 2018;28:e44-e48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Tohda G, Ohtani M, Dochin M. Efficacy and safety of emergency endoscopic retrograde cholangiopancreatography for acute cholangitis in the elderly. World J Gastroenterol. 2016;22:8382-8388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 31] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Han SJ, Lee TH, Kang BI, Choi HJ, Lee YN, Cha SW, Moon JH, Cho YD, Park SH, Kim SJ. Efficacy and Safety of Therapeutic Endoscopic Retrograde Cholangiopancreatography in the Elderly Over 80 Years. Dig Dis Sci. 2016;61:2094-2101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Ali M, Ward G, Staley D, Duerksen DR. A retrospective study of the safety and efficacy of ERCP in octogenarians. Dig Dis Sci. 2011;56:586-590. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1716] [Cited by in F6Publishing: 1607] [Article Influence: 57.4] [Reference Citation Analysis (2)] |
| 13. | Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433-435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 120] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, Prada A, Passoni GR, Testoni PA. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417-423. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Talar-Wojnarowska R, Szulc G, Woźniak B, Pazurek M, Małecka-Panas E. Assessment of frequency and safety of endoscopic retrograde cholangiopancreatography in patients over 80 years of age. Pol Arch Med Wewn. 2009;119:136-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Fritz E, Kirchgatterer A, Hubner D, Aschl G, Hinterreiter M, Stadler B, Knoflach P. ERCP is safe and effective in patients 80 years of age and older compared with younger patients. Gastrointest Endosc. 2006;64:899-905. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Ashton CE, McNabb WR, Wilkinson ML, Lewis RR. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Ageing. 1998;27:683-688. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Grönroos JM, Salminen P, Laine S, Gullichsen R. Feasibility of ERCP procedures in patients 90 years of age and older. J Clin Gastroenterol. 2010;44:227-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Panteris V, Vezakis A, Filippou G, Filippou D, Karamanolis D, Rizos S. Influence of juxtapapillary diverticula on the success or difficulty of cannulation and complication rate. Gastrointest Endosc. 2008;68:903-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Zhong H, Wang X, Yang L, Miao L, Ji G, Fan Z. Modified transprepancreatic septotomy reduces postoperative complications after intractable biliary access. Medicine (Baltimore). 2018;97:e9522. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Ince AT, Baysal B. Pathophysiology, classification and available guidelines of acute pancreatitis. Turk J Gastroenterol. 2014;25:351-357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Tabak F, Ji GZ, Miao L. Impact of Periampullary Diverticulum on ERCP Papillary Cannulation. Preprints. 2020;2020010076. [DOI] [Cited in This Article: ] |
| 23. | Sakai Y, Tsuyuguchi T, Yokosuka O. Clinical usefulness and current problems of pancreatic duct stenting for preventing post-ERCP pancreatitis. World J Clin Cases. 2014;2:426-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Sundaralingam P, Masson P, Bourke MJ. Early Precut Sphincterotomy Does Not Increase Risk During Endoscopic Retrograde Cholangiopancreatography in Patients With Difficult Biliary Access: A Meta-analysis of Randomized Controlled Trials. Clin Gastroenterol Hepatol. 2015;13:1722-1729.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Lukens FJ, Howell DA, Upender S, Sheth SG, Jafri SM. ERCP in the very elderly: outcomes among patients older than eighty. Dig Dis Sci. 2010;55:847-851. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |