Published online Mar 6, 2019. doi: 10.12998/wjcc.v7.i5.650
Peer-review started: November 13, 2018
First decision: December 29, 2018
Revised: January 28, 2019
Accepted: January 29, 2019
Article in press: January 30, 2019
Published online: March 6, 2019
Congenital maxillomandibular syngnathia is an extremely rare disorder characterized by craniofacial malformations and inability to open the mouth adequately, which leads to problems with feeding, swallowing, and breathing as well as temporomandibular joint ankylosis. The main goal of the surgery is to release the ankylosis, establish functioning mandible, and prevent re-fusion. However, surgical procedures for this disease are rarely reported.
Here, we report a 7-mo-old girl with bilateral maxillomandibular syngnathia. The patient presented with difficulty in feeding, breathing, sounding, and swallowing and had developmental dysplasia. For treatment, we performed bone isolation by computer-assisted navigation and used silicone to fix the wound surface to prevent refusion of bone. To our knowledge, this is the only syngnathia case in the literature treated using computer-assisted navigation. With the guidance of precise navigation, we were able to minimize operation time by at least one hour, the patient's blood vessels, nerves, and tooth germs were well protected, and excessive bleeding was avoided. After six weeks, the patient showed improvement in mouth opening and no major issues of feeding.
Application of computer-assisted navigation can significantly improve accuracy, effectiveness, and surgical safety in correcting congenital maxillomandibular syngnathia.
Core tip: Congenital maxillomandibular fusion is a rare anomaly of the craniofacial region. We report a 7-mo-old girl with bilateral maxillomandibular syngnathia. We performed bony isolation by computer-assisted navigation, a first-of-its-kind treatment approach for syngnathia. The operation time was minimized by at least one hour, and the patient's blood vessels, nerves, and tooth germs were well protected, and bleeding was minimized. There were major improvements in the patient's status. We concluded that application of computer-assisted navigation can significantly improve accuracy, effectiveness, and surgical safety in difficult-to-treat deformity.
- Citation: Lin LQ, Bai SS, Wei M. Application of computer-assisted navigation in treating congenital maxillomandibular syngnathia: A case report. World J Clin Cases 2019; 7(5): 650-655
- URL: https://www.wjgnet.com/2307-8960/full/v7/i5/650.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i5.650
Congenital craniofacial disorders represent approximately 20% of all birth defects. Syngnathia, a rare craniofacial disorder, is characterized by fusion of the hard and soft tissues of the jaw. The first case of syngnathia was reported by Burket in 1936 in a patient who had multiple diagnoses, including temporomandibular joint (TMJ) ankyloses, fusion of gums, associated facial hemiatrophy, and Horner syndrome[1]. A significant complication in syngnathia patients is restricted mouth opening, which results in feeding, swallowing, and respiration problems. Early recognition and treatment are critical for normal growth and development. The aim of the case report is to introduce the application of computer-assisted navigation during syngnathia corrective surgery.
A 7-month-old girl with a clinical diagnosis of congenital maxillomandibular fusion was referred to the Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine for surgery. She was suffering from bilateral maxillomandibular syngnathia and inability to open mouth.
The patient was fed through a straw by his grandmother.
She had no past history of surgery and was not taking any medication.
She was the first child of the parents (mother 28 years old, father 30 years old) and was born via an uncomplicated vaginal delivery. The parents did not have a history of consanguineous marriage. A similar symptom was not observed in other patient’s family members.
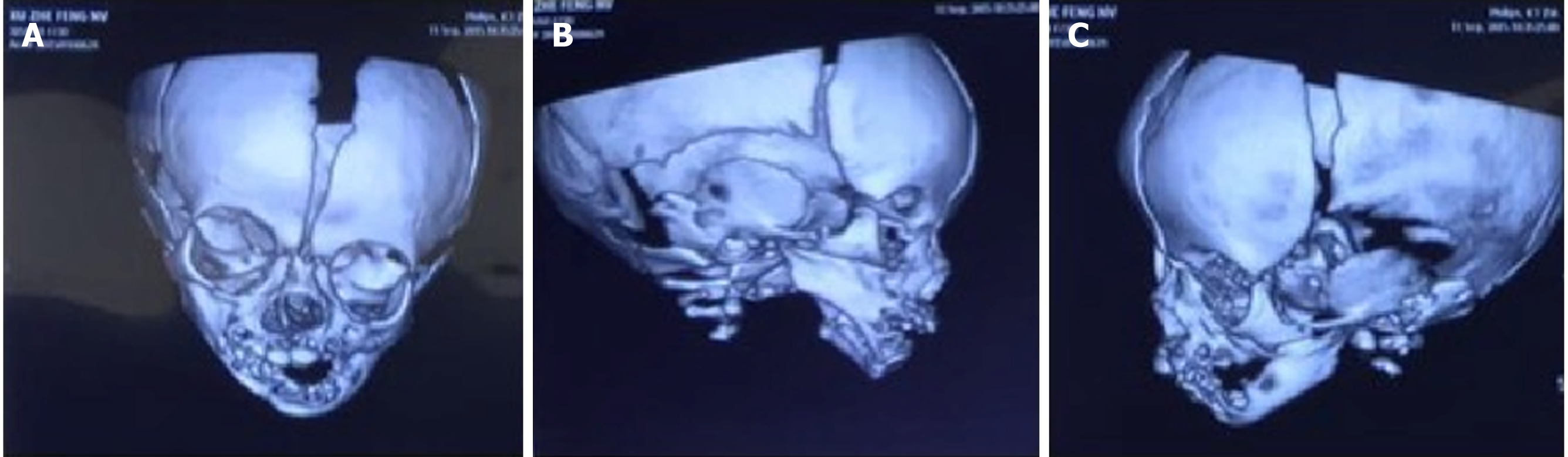
Physical examination revealed sever retardation - she was 73 cm tall and weight 5.5 kg - but did not reveal any congenital or systemic problems. She also presented with difficulty in feeding, breathing, sounding, and swallowing. The patient had difficulty in opening her mouth more than 1 mm in diameter. In her oral cavity, the upper and lower gums were completely fused and two deciduous teeth in the mandible were visible (Figure 1). Otherwise no abnormalities were noted.
No abnormality was seen in routine blood tests, biochemical tests, or ECG.
A three-dimensional CT scan showed bilateral maxillomandibular fusion and very little oral cavity (Figure 2). These observations are consistent with TMJ ankyloses, a typical clinical feature in syngnathia patients.
Congenital maxillomandibular syngnathia.
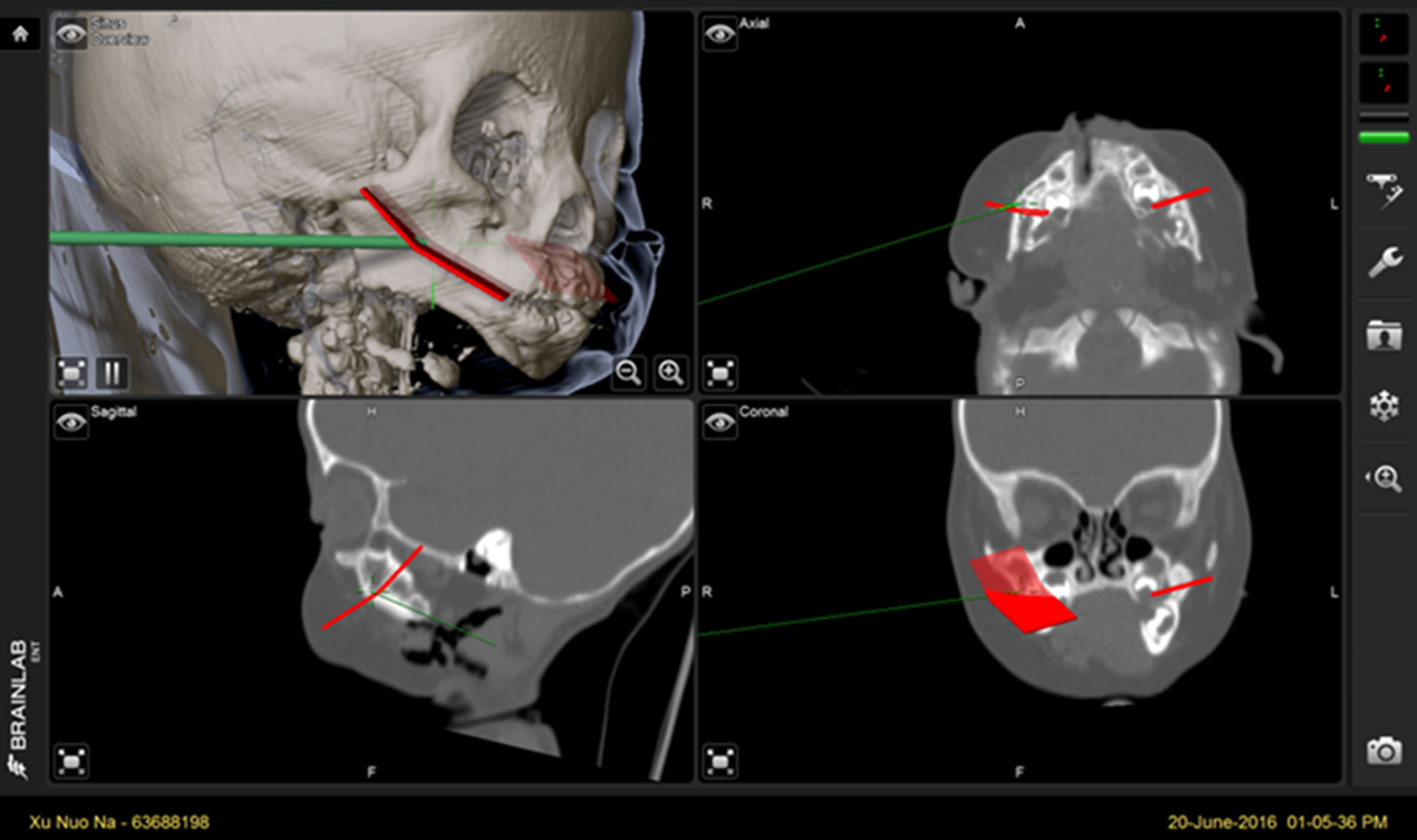
The purpose of the surgery was to separate the fused mandible and maxilla to open the mouth, which would solve the patient’s feeding issues. The patient underwent a prophylactic tracheostomy to prevent obstruction of airway during surgery 7 d in advance. Then, we prepared for computer-assisted navigation. Three-dimensional CT data were saved in the Dicom (digital imaging and communications in medicine) format and were imported into Mimics 10.0 software (Materialise, Leuven, Belgium) and the iPlan software of the VectorVision2 navigation system (BrainLAB, Feldkirchen, Germany). The anatomical landmarks were measured and analyzed on the basis of three-dimensional images. We chose the line from preauricular to marginal mandibular as the incision site. Operation simulations were performed to affirm the position of osteotomy line and the level of mandibular opening and its fixed position. The patient underwent general anaesthesia and the skin was sterilized. A navigation bracket was installed to the patient’s head first, and then face scanning by a laser scanner was performed for surface registration. The surgical instrument was registered at last. Registration accuracy (0.8 mm) was verified using the navigation pointer. The tip position and orientation of the probe were viewed continuously on screen (Figure 3). The oral space was exposed by retractors, the skin and subcutaneous tissue of incision were cut open, and the bilateral jaw lateral surface was exposed by blunt separation. It was easy to detect and isolate the mandible using the navigation system. Real-time position was verified by the navigation probe to avoid damaging important nerves, vessels, and dental germs. After the mandible was sawed off, silicone was fixed on the wound surface to prevent refusion of bone. Negative pressure drainage was put in the bilateral mandibles prior to suturing the incision. Perioperative bleeding was 100 mL. The patient was admitted to SICU after surgery.
Immediately following surgery, the patient had difficulty swallowing, so we used a nasogastric tube for feeding. The patient was discharged from the hospital one week later and was instructed to perform mouth opening and swallowing exercises. Follow-up three-dimensional CT scans of the face confirmed separation and bony healing. After six months, there was no recurrence. After eight months, the patient was 91 cm in height, weighed 11 kg, and could pronounce several single words; thus, we concluded that the surgery was successful.
Syngnathia is a rare human congenital condition. It involves connection between soft tissues or fusion between bony tissues and varies in severity from single mucosal bands (synechiae) to complete bone fusion (synotosis)[2]. Syngnathia is often accompanied by additional congenital defects, such as microglossia, micrognathia, and TMJ abnormalities. There are approximately 60 cases of congenital bony syngnathia reported in the literature[3], which reveal a high degree of variability in the location and extent of jaw fusion, and indicate that bony syngnathia may be isolated or syndromic. It is estimated that only 18% of cases are associated with known syndromes, such as aglossia-adactylia syndrome or hemifacial microsomia[4]. In the reported cases, women commonly display an isolated form of syngnathia, whereas men display a more complex pattern of disease. Syngnathia is usually detected immediately after birth because the baby is not able to open the mouth to feed normally. Notably, patients presenting with complete bilateral synostosis of the upper and lower jaw represent the least common and most severe form of syngnathia.
The etiology and pathogenesis of syngnathis remain unknown, and it is an extremely rare condition involving abnormal development of the splanchnocranium, which is the part of the skull that is derived from the branchial arches[2]. Various etiologies have been proposed, including environmental insults, medications such as meclizine, persistence of the buccopharyngeal membrane, and amniotic constriction bands[5,6]. Villanueva-García and colleagues have suggested the possibility of an autosomal recessive occurrence[7]. Moreover, a recent molecular genetics study showed that the Foxc1 and Fgf8 genes play a role in regulating mammalian jaw patterning and mutations in these genes may underlie the pathogenesis of syngnathia[4]. However, given that our patient had no other congenital abnormalities and there was no significant family history, a genetic or syndromic cause is unlikely.
Surgical division of the fusion must be carried out as soon as possible, which is necessary for normal feeding, removing airway obstruction, and allowing normal mandibular growth. Delay in surgical treatment increases the possibility of TMJ ankylosis, which leads to a lack of mandibular growth and facial deformities. The main goal of the surgery described in this care report was to release syngnathia and prevent recurrence. New management techniques, such as distraction, have been reported in congenital maxillomandicular[8]. Since most syngnathia patients are infants, major surgical challenges are intraoperative blood loss and damage to nerves and dental germs. Another challenge stems from the lack of comprehensive guidelines to ensure patient safety during this type of surgery.
In the present case, we applied computer-assisted navigation to instruct our surgical approach. Computer navigation has emerged as an essential technology for guiding and verifying operations, such as reconstruction of mandible or orbital bone, orthognathia, and many other of craniofacial surgeries[9,10]. We can understand the correlations among surgical devices, incisions, and peripheral anatomic sites in real-time easily via computer navigation, and also can check the distance between the operation positions to the position designed preoperatively. With the precise guidance of computer navigation, our operative time was minimized by at least one hour. Moreover, the patients’ blood vessels, nerves, and tooth germs were all well protected and perioperative bleeding was minimized.
We have demonstrated a novel approach to treating complex zygomaticomandibular syngnathia. Distraction techniques, like the one used here, should prove useful in addressing other craniofacial malformations. To our knowledge, this is the only syngnathia case in the literature treated using distraction techniques. In the future, our approach could be optimized to manage and prevention recurrence in other syngnathia patients.
The authors would like to thank the research staff and clinical personnel of the Shanghai 9th People’s Hospital for their outstanding performance and patient care.
Manuscript source: Unsolicited manuscript
Specialty type: Research and Experimental Medicine
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Karatza AA; Rolle U S- Editor: Dou Y L- Editor: Wang TQ E- Editor: Bian YN
| 1. | Martín LP, Pérez MM, García EG, Martín-Moro JG, González JI, García MB. Atypical case of congenital maxillomandibular fusion with duplication of the craniofacial midline. Craniomaxillofac Trauma Reconstr. 2011;4:113-120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Broome M, Vial Y, Jacquemont S, Sergi C, Kamnasaran D, Giannoni E. Complete Maxillo-Mandibular Syngnathia in a Newborn with Multiple Congenital Malformations. Pediatr Neonatol. 2016;57:65-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Al-Mahdi AH, Koppel DA, Al-Jumaily HA, Mohammed AA, Boyd D. Congenital Bilateral Zygomatico-Maxillo-Mandibular Fusion Associated With Gum Fusion. J Craniofac Surg. 2016;27:e20-e23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Inman KE, Purcell P, Kume T, Trainor PA. Interaction between Foxc1 and Fgf8 during mammalian jaw patterning and in the pathogenesis of syngnathia. PLoS Genet. 2013;9:e1003949. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Fallahi HR, Naeini M, Mahmoudi M, Javaherforoosh F. Congenital zygomatico-maxillo-mandibular fusion: a brief case report and review of literature. Int J Oral Maxillofac Surg. 2010;39:930-933. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Turksen Z, Ozakpinar HR, Tellioglu AT. A case of syngnathia, cleft palate and hypospadias: an isolated case or syndromic syngnathism? J Craniomaxillofac Surg. 2012;40:8-10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Villanueva-García D, Contreras-Masse G, Villa-Guillén M, Ramón-García G, Murguía-De Sierra T. Syngnathism in an infant born to consanguineous parents. Am J Med Genet A. 2009;149A:2303-2305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Konaş E, Aliyev A, Tunçbilek G. Congenital maxillomandibular syngnathia: a new management technique using distraction techniques. J Craniofac Surg. 2015;26:e68-e70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Rahimov CR, Farzaliyev IM, Fathi HR, Davudov MM, Aliyev A, Hasanov E. The Application of Virtual Planning and Navigation Devices for Mandible Reconstruction and Immediate Dental Implantation. Craniomaxillofac Trauma Reconstr. 2016;9:125-133. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Varley I, White L, Salvi SM, Lee N. Digital import of orbital implants to enhance navigation in reconstruction of the deep orbit. Orbit. 2016;35:20-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |