Published online Oct 6, 2019. doi: 10.12998/wjcc.v7.i19.3027
Peer-review started: May 10, 2019
First decision: August 1, 2019
Revised: August 3, 2019
Accepted: August 20, 2019
Article in press: August 20, 2019
Published online: October 6, 2019
Uterine myomas are the most common benign gynecological soft tissue tumors in women but polycythemia associated with these tumors is rare. Polycythemia is significantly associated with risk of venous thromboembolism (VTE), which is further increased in case of a large pelvic mass and obesity. Here we report the surgical challenges in the case of an obese patient with a giant fibromatous uterus and associated polycythemia.
A 42-year-old obese woman was referred to our department for treatment for a huge fibromatous uterus. She suffered of pelvic pressure and abdominal distension and reported severe dyspnea from several months. Laboratory analyses including hemoglobin (Hb) 19.2 g/dL and hematocrit (Hct) 59.7% were indicative of polycythemia. Arterial blood gas analysis showed arterial oxygen pressure (pO2) of 81.5 mmHg. Abdominal computed tomography confirmed a giant fibromatous uterus measuring 28.2 cm × 17 cm × 25 cm. To reduce the thromboembolic risk, the patient underwent low molecular weight heparin, phlebotomy twice before surgery, and we opted for a laparoscopic hysterectomy. The uterus weighed 5400 g and the histology confirmed a diagnosis of leiomyoma. We did not find increased erythropoietin levels in the supernatant of the myomatous uterine tissue. There were no complications. On postoperative day 1, the Hb and the Hct levels normalized to 13.3 g/dL and 41.7%, respectively. Arterial blood gas analysis after surgery showed a pO2 of 144.7 mmHg. These results suggested the diagnosis of myomatous erythrocytosis syndrome. The patient was discharged on the second postoperative day in very good condition with no symptoms.
We believe this is the first reported laparoscopic hysterectomy in a patient with a giant uterus, polycythemia and obesity. Multiple VTE risk factors warranted a laparoscopic approach.
Core tip: Uterine myoma are rarely associated with polycythemia. Here we report the challenging case of an obese patient with a giant fibromatous uterus and associated polycythemia; these factors increased significantly the risk of venous thromboembolism. To reduce such risk, we opted for a laparoscopic hysterectomy, which was preceded by phlebotomy. Laparoscopy was successfully completed without complications. The uterus weighed 5400 g. After surgery the patient’s hematological profile normalized. The final diagnosis was myomatous erythrocytosis syndrome (MES). To our knowledge, this is the first case of laparoscopic hysterectomy in an obese patient with a very large uterus and polycythemia due to MES.
- Citation: Macciò A, Chiappe G, Lavra F, Sanna E, Nieddu R, Madeddu C. Laparoscopic hysterectomy as optimal approach for 5400 grams uterus with associated polycythemia: A case report. World J Clin Cases 2019; 7(19): 3027-3032
- URL: https://www.wjgnet.com/2307-8960/full/v7/i19/3027.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i19.3027
Uterine myomas are the most common benign gynecological soft tissue tumors in women but polycythemia associated with these tumors is rare[1-3]. In 1953 Thomson and Marson described the first patients with polycythemia linked to uterine myomas, in which tumor excision resulted in the cure of this hematological disorder[4]. In 1957 Fleming et al[5] defined this condition as myomatous erythrocytosis syndrome (MES) when associated with polycythemia, a myomatous uterus, and a return to a normal hematological profile following hysterectomy or myomectomy.
Typically, secondary polycythemia is related to defective lung function, congenital heart disorder and tumors[6]. In MES it is believed that polycythemia is strictly linked to the excessive production of erythropoietin (EPO) by the tumors[7], but oxygenation disorders in the presence of a large abdomino-pelvic mass may also be the cause[8]. Complications of polycythemia include a significantly increased risk of arterial and venous thromboembolism (VTE)[9] and pose a problem in the choice of surgical approach. In fact, in this syndrome the polycythemia is typically resolved with the removal of the tumor and therefore the choice of surgical approach is crucial in patient’s management. It is also known that the surgery and the time of bed-rest and convalescence are associated with increased rates of VTE[10]. Here we discuss the case of an obese patient with a giant fibromatous uterus and polycythemia that raised challenges about the choice of surgical approach. In fact, it is known that both obesity and a large pelvic mass are common risk factors for venous thrombosis. The invasive venography or contrast-enhanced computed tomography have exactly showed that large uterine fibroids can constrict pelvic veins[11], and it is known that obesity further increases the thrombotic risk in all types of surgery[12].
To our knowledge this is the first described report of a laparoscopic hysterectomy performed in a patient with a giant uterus (5400 g), polycythemia and obesity.
A 42-year-old woman was referred to our department for treatment for a huge fibromatous uterus.
Her symptoms included pelvic pressure and abdominal distension and for several months’ severe dyspnea.
Her medical history included a thyroidectomy for a thyroid cancer under treatment with L-thyroxine.
The patient was gravida 0, para 0.
Her weight was 85 kg and height 156 cm (body mass index 35). At physical examination her abdomen appeared filled by a pelvic mass arriving at the xiphoid process.
Laboratory analysis produced the following results: red blood cell count, 7.04 ×106/mm3; hemoglobin (Hb), 19.2 g/dL; hematocrit (Hct), 59.7%; white blood cell count, 9400/mm3; platelets 325/mm3; iron 47 mcg/dL; ferritin 14 mcg/L; transferrin 310 mg/dL; C-reactive protein 0.5 mg/dL (range ≤ 0.10 mg/dL); serum levels of EPO 45 mIU/mL (normal range: 0-29.0 mU/mL); Ca-125: 11.9 U/mL; Ca 19-9: 26 U/mL; Ca 15.3: 41 U/mL; and He4: 34.4 pmol/L. These results were in line with the diagnosis of polycythemia[13,14].
The arterial blood gas analysis showed arterial oxygen pressure (pO2) of 81.5 mmHg (pCO2 38.4 mmHg; Oxygen saturation, sO2 96.2%; Hct 61%; and total Hb 20.6 g/dL). The preoperative cytology of the endometrium was normal.
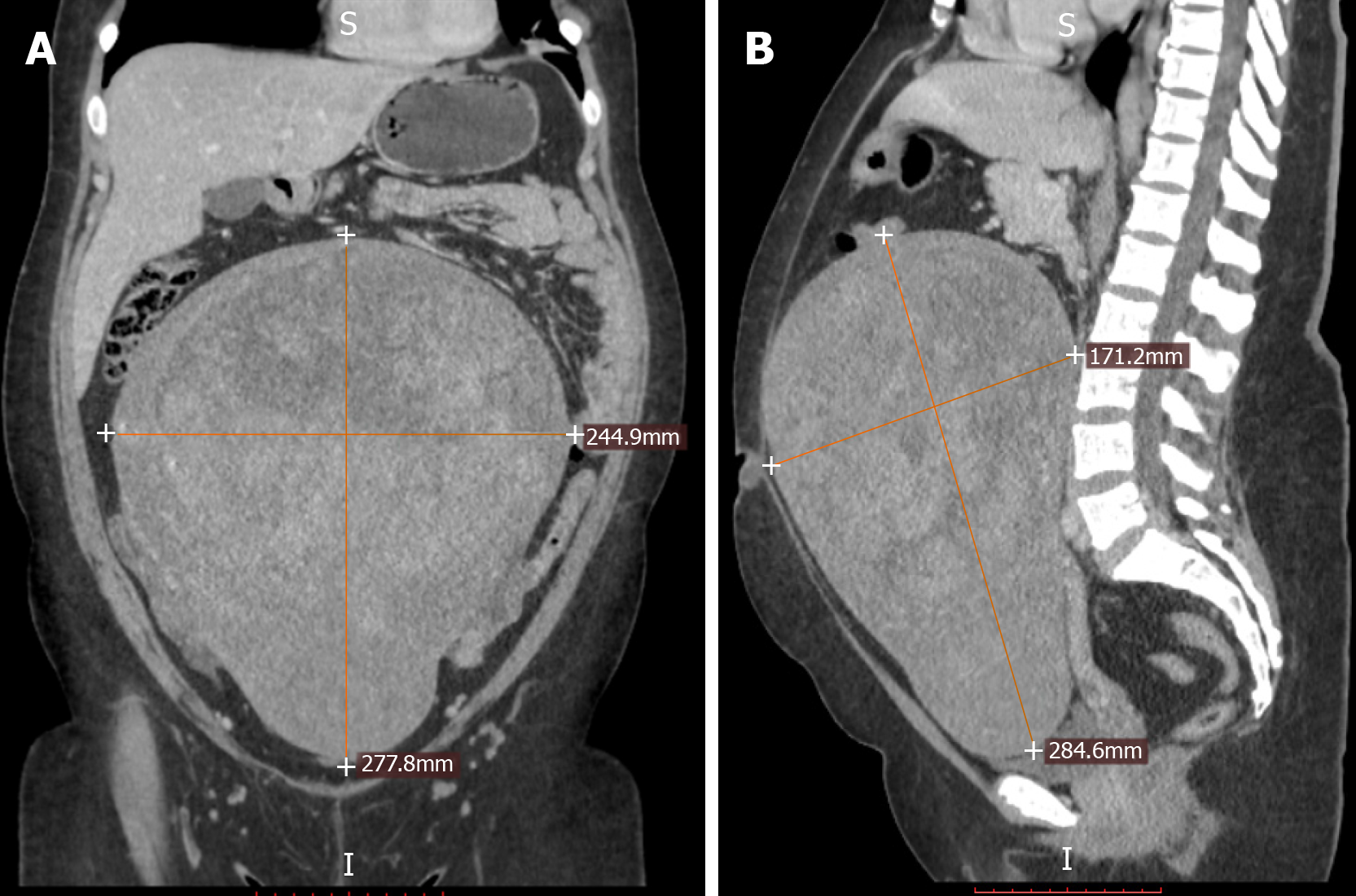
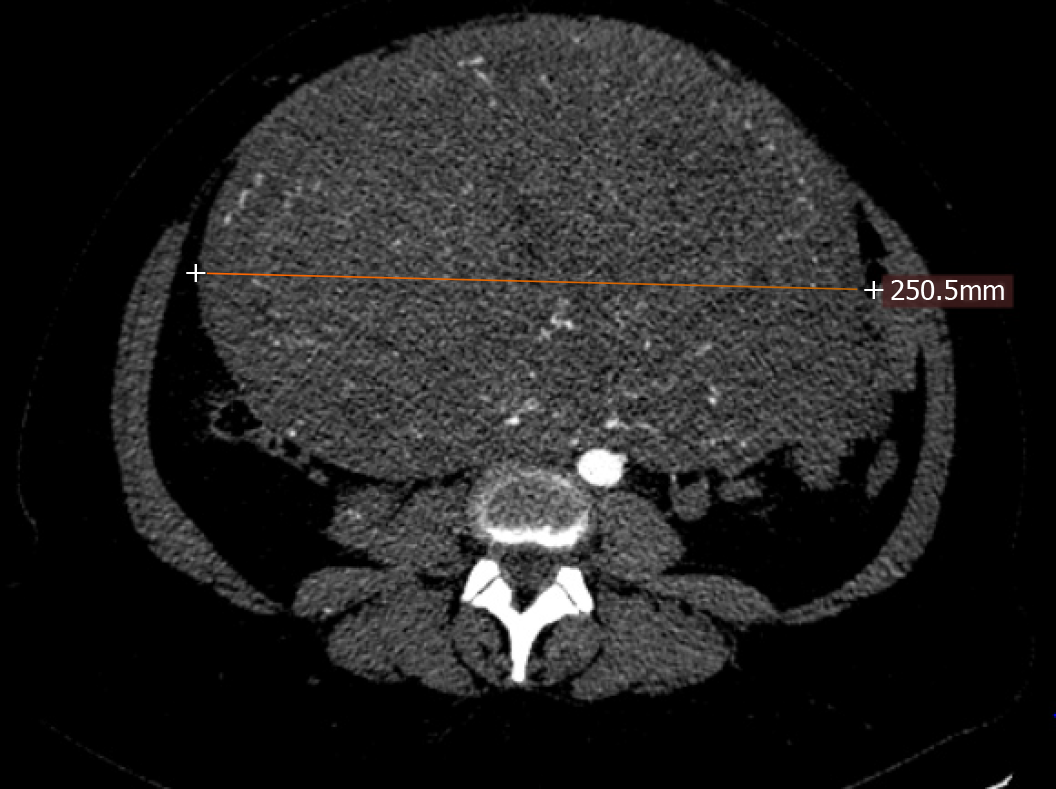
Preoperative abdominal and transvaginal ultrasound showed a huge fibromatous uterus. The abdominal CT scan (Figure 1 and Figure 2) confirmed a giant fibromatous uterus with important vascularization and inhomogeneous contrast enhancement, with clear limits and regular margins measuring 28.2 cm × 17 cm × 25 cm. The mass displaced the ileal loops upward and to the left.
These results suggested the diagnosis of polycythemia associated with a giant fibromatous uterus (MES).
To reduce the thromboembolic risk in the perioperative period, the patient underwent treatment with low weight molecular heparin (enoxaparin 4000 UI/die), phlebotomy two times before surgery, and to further reduce this fearsome complication we opted for a laparoscopic hysterectomy approach (total laparoscopic hysterectomy, TLH). After the phlebotomies, the day of surgery, the patient’s preoperative Hb and Hct values were reduced to 16.8 g/dL and 51.2%, respectively.
We performed the surgery with the patient under general anesthesia in the lithotomy position. We placed a nasogastric tube to reduce the risk of stomach distention and perforation. For better uterus manipulation, we utilized the ClearView® Uterine Manipulator-7 cm (Ethicon Endo-Surgery, Cincinnati, United States). A 12-mm trocar was placed exactly under the xiphoid process and a pneumoperitoneum of 10-14 mmHg was generated in a neutral position and kept for the whole duration of the surgery. Intra-abdominal view was obtained with a 10 mm, 0° telescope (Karl Storz, Tuttlingen, Germany). We placed two 5-mm trocars in the hypochondrium lateral to the rectus abdominis muscle, a third 12-mm trocar at the umbilicus and another 5 mm trocar in the suprapubic position. TLH was then carried out in a consolidated technique reported in detail in our previous manuscripts[15,16]. To perform all the procedures, we used the LigaSure™ (Medtronic; AutoSuture Co., Norwalk, CT) and the BiClamp® LAP forceps (ERBE GmbH, Tubingen, Germany). Once completed the extrafascial hysterectomy, we extracted the uterus through a very low transverse laparotomic incision of about 5 cm, utilizing a wound protector/retractor (Wound Edge Protector - 3M™ Steri-Drape™ 1073, Diegem, Belgium) to safeguard the cut site, and morcellated it using a cold blade scalpel outside to avoid spillage.
At the conclusion of surgery, following the suture of the accessory laparotomy, we laparoscopically examine the abdominal cavity and washed it carefully to remove any possible residue. There were no complications; the operative time was approximately 220 min. Intraoperative blood loss was ≤ 10 ml. The arterial blood gas analysis after surgery showed a pO2 of 144.7 mmHg (pCO2 40.4 mmHg; sO2 98.8; Hct 45%; tHb 15.4 g/dL).
The weight of the uterus was 5400 g. The histological examination confirmed the diagnosis of leiomyoma. In order to determine whether the uterine leiomyoma was producing EPO, 200 mg frozen samples of the myoma tissue were blended with 500 mL of lysis buffer including the tissue protein extraction reagent and protease inhibitor mixture (Thermo Scientific). The supernatant was gathered by centrifugation at 10000 x g for 5 min, and the EPO levels were analyzed by a human EPO enzyme-linked immunosorbent assay (ELISA) (DRG Instruments GmbH, Marburg, Germany). A same size sample of myoma tissue from a patient without polycythemia was used as a control. The EPO level in the myomatous tissue of our patient was 1.5 mIU/mg, similar to the level found in the control sample (1 mIU/mg).
The patient’s postoperative course was wonderful. On postoperative day 1, the Hb level had normalized to 13.3 g/dL, and the Hct level had fallen to 41.7%. The patient left the hospital on the second postoperative day in very good general status and with no symptoms.
Repeated blood analyses after 1 wk (Hb 12.6 g/dL, Hct 38.7%) and 4 mo (Hb 12.8 g/dL, Hct 40.6%), confirmed the normalization of the patient’s hematological profile, so we were able to report the case in question as a MES.
Hysterectomy for uterine fibromatosis is the most common procedure in gynecologic surgery[17]. Surgeons are increasingly employing laparoscopy for hysterectomy[18]. However, the role of laparoscopy in the presence of giant uteri is still debated. Siedhoff et al[19] carried out a decision analysis comparing laparoscopic hysterectomy to abdominal hysterectomy for the treatment of the large uteri with supposed benign myomas, examining mortality, surgical complications, and quality of life. They demonstrated a decreased overall mortality associated with laparoscopic hysterectomy and morcellation compared to laparotomic approach. In particular, the laparoscopic group had lesser incidence of VTE (690 vs 840 per 100000) associated with reduced bedrest compared to the abdominal group[19]. This evidence finds its emphasis in clinical conditions such as large uterine volume and obesity that predispose to VTE, and becomes even more important in rare conditions such as polycythemia associated with uterine fibromatosis, that further increase the risk. The clinical case described here is the first relative to laparoscopic hysterectomy in a patient with MES and a giant fibromatous uterus (5400 g). The polycythemia associated with this clinical case and the possibility of an associated VTE strongly suggests the need for a careful choice of the hysterectomy procedure. There is no doubt that laparoscopic hysterectomy has certain advantages over abdominal hysterectomy in terms of less bed rest and convalescence time and should be considered the option of choice, especially in conditions predisposing to thromboembolism[20]. The problem of the volume of the uterus still influences the choice of the most adequate surgical procedure, but this clinical case demonstrates once again that laparoscopic hysterectomy is feasible and free of side effects even in case of giant uterus[15,16].
Notably, this patient's polycythemia did not depend on uterine EPO production but was probably due to the excessive number of months in which the patient suffered dyspnea with a physiological obstacle to the oxygenation of the blood due to the large volume of the uterus.
This study highlights the need for careful screening so that women suffering from uterine fibromatosis are treated before this results in excessive uterine volume with potentially very severe related symptoms. Laparoscopic hysterectomy should be considered as the optimal surgical approach to reduce the risk of VTE, even in cases of very large uteri.
The authors thank Gianluigi Crabu for his technical assistance.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Daniilidis A S-Editor: Dou Y L-Editor: A E-Editor: Qi LL
| 1. | Blockeel C, De Beeck BO, Bourgain C, Amy JJ. Myomatous erythrocytosis syndrome. Natl Med J India. 2005;18:247-249. [PubMed] [Cited in This Article: ] |
| 2. | LevGur M, Levie MD. The myomatous erythrocytosis syndrome: a review. Obstet Gynecol. 1995;86:1026-1030. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 33] [Article Influence: 1.1] [Reference Citation Analysis (2)] |
| 3. | Mui J, Yang MMH, Cohen T, McDonald DI, Hunt H. More Than a Myoma: A Review of Myomatous Erythrocytosis Syndrome. J Obstet Gynaecol Can. 2019;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Thomson AP, Marson FB. Polycythemia with fibroids. Lancet. 1953;262:759–760. [DOI] [Cited in This Article: ] |
| 5. | Fleming AR, Markley JC. Polycythemia associated with uterine myomas. Am J Obstet Gynecol. 1957;74:677-679. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Thiele J, Kvasnicka HM, Muehlhausen K, Walter S, Zankovich R, Diehl V. Polycythemia rubra vera versus secondary polycythemias. A clinicopathological evaluation of distinctive features in 199 patients. Pathol Res Pract. 2001;197:77-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Hertko EJ. Polycythemia (erythrocytosis) associated uterine fibroids and apparent surgical cure. Am J Med. 1963;34:288-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 8] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Abdul Ghaffar NA, Ismail MP, Nik Mahmood NM, Daud K, Abu Dzarr GA. Huge uterine fibroid in a postmenopausal woman associated with polycythaemia: a case report. Maturitas. 2008;60:177-179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Gordeuk VR, Key NS, Prchal JT. Re-evaluation of hematocrit as a determinant of thrombotic risk in erythrocytosis. Haematologica. 2019;104:653-658. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Moulder JK, Siedhoff MT, Till SR, Moll S. Management considerations for patients with uterine fibroids and concurrent venous thromboembolism. Curr Opin Obstet Gynecol. 2016;28:329-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Lacharite-Roberge AS, Raza F, Bashir R, Dass CA, Moser GW, Auger WR, Toyoda Y, Forfia PR, Vaidya A. Case series of seven women with uterine fibroids associated with venous thromboembolism and chronic thromboembolic disease. Pulm Circ. 2019;9:2045894018803873. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Hunt BJ. Hemostasis at Extremes of Body Weight. Semin Thromb Hemost. 2018;44:632-639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Huber FL, Latshang TD, Goede JS, Bloch KE. Does venous blood gas analysis provide accurate estimates of hemoglobin oxygen affinity? Ann Hematol. 2013;92:517-521. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | McMullin MFF, Mead AJ, Ali S, Cargo C, Chen F, Ewing J, Garg M, Godfrey A, Knapper S, McLornan DP, Nangalia J, Sekhar M, Wadelin F, Harrison CN; British Society for Haematology Guideline. A guideline for the management of specific situations in polycythaemia vera and secondary erythrocytosis: A British Society for Haematology Guideline. Br J Haematol. 2019;184:161-175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 15. | Macciò A, Kotsonis P, Lavra F, Chiappe G, Sanna D, Zamboni F, Madeddu C. Laparoscopic removal of a very large uterus weighting 5320 g is feasible and safe: a case report. BMC Surg. 2017;17:50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Macciò A, Chiappe G, Kotsonis P, Nieddu R, Lavra F, Serra M, Onnis P, Sollai G, Zamboni F, Madeddu C. Surgical outcome and complications of total laparoscopic hysterectomy for very large myomatous uteri in relation to uterine weight: a prospective study in a continuous series of 461 procedures. Arch Gynecol Obstet. 2016;294:525-531. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Wright JD, Herzog TJ, Tsui J, Ananth CV, Lewin SN, Lu YS, Neugut AI, Hershman DL. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122:233-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 459] [Cited by in F6Publishing: 489] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 18. | Lee J, Jennings K, Borahay MA, Rodriguez AM, Kilic GS, Snyder RR, Patel PR. Trends in the national distribution of laparoscopic hysterectomies from 2003 to 2010. J Minim Invasive Gynecol. 2014;21:656-661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Siedhoff MT, Wheeler SB, Rutstein SE, Geller EJ, Doll KM, Wu JM, Clarke-Pearson DL. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212:591.e1-591.e8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 20. | Qu H, Li Z, Zhai Z, Liu C, Wang S, Guo S, Zhang Z. Predicting of Venous Thromboembolism for Patients Undergoing Gynecological Surgery. Medicine (Baltimore). 2015;94:e1653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |