Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2513
Peer-review started: May 14, 2019
First decision: May 30, 2019
Revised: July 15, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 6, 2019
Cutaneous involvement in Hodgkin lymphoma (HL) is a rare finding. Few cases have been reported in literature, most describing paraneoplastic manifestations. Only very few papers have described primary HL skin infiltration, reporting a wide range of clinical presentations that frequently include ulcers; plaques, nodules and papules have also been noticed.
We report the case of a 56-year-old man who presented fever, multiple adenomegalies of neck and axilla and thick serpiginous skin lesions involving bilateral pectoral regions. After an initial diagnostic workup for a suspected active infectious disease, a lymph node biopsy was performed, which showed a neoplastic invasion from a mixed cellularity classical HL. The same histological pattern was described in a cutaneous biopsy of the chest lesions. The other staging procedures performed revealed an advanced disease, with unfavourable clinical prognostic features. The patient was prescribed 6 cycles of ABVD chemotherapy scheme (doxorubicin, bleomycin, vinblastine, dacarbazine), a regiment that requires demonstration of metabolic response achievement at the interim PET/CT scan to confirm continuation or to change therapeutic strategy.
Skin involvement in HL is a rare finding and may represent a challenging clinical presentation due to extremely various types of lesions observed.
Core tip: We report the case of a 56-year-old man presenting with neck and armpits swelling, fever and thick cutaneous chest lesions. Active infectious disease was ruled out and a lymph node biopsy was carried out, diagnostic for Hodgkin lymphoma (HL). Histological examination of pectoral cutaneous serpiginous plaques resulted positive for the same haematological malignancy infiltration. Skin involvement in HL is a rare finding, with main clinical manifestations being ulcers, papules and nodules. We describe this peculiar finding to underline the need for a correct differential diagnosis, especially for other malignancies and infectious disorders.
- Citation: Massaro F, Ferrari A, Zendri E, Zanelli M, Merli F. Atypical cutaneous lesions in advanced-stage Hodgkin lymphoma: A case report. World J Clin Cases 2019; 7(17): 2513-2518
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2513.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2513
Hodgkin lymphoma (HL) is a B-cell neoplasm accounting for 10%-15% of all lymphomas in Europe and the United States[1,2]. The disease is characterised by nodal infiltration, typically involving cervical, mediastinal and axillary regions (accounting for almost 90% of HL presentations), while extranodal involvement occurs in almost a quarter of cases, more often secondary to contiguous spreading from bulky masses [3]. Skin involvement is rare in HL (< 1%) and has been reported both in specific and non-specific presentations[4,5]. Specific lesions are related to the histological demonstration of HL cutaneous infiltration secondary to direct, lymphatic or haematogenous spread and usually occurs in advanced stage diseases, despite the rare finding of a primary cutaneous HL (PCHL) having been reported in literature[6,7]. Non-specific lesions have several clinical types of presentation (pityriasis-like, psoriatic, erythema nodosum, eczematoid) and must be considered as paraneoplastic events[8].
We describe the case of a 56-year-old male patient, who came to our attention for the onset of fever, multiple cervical and axillary lymphadenopathy and bilateral cutaneous pectoral lesions.
A 56-year-old male patient, born in Pakistan and of Pakistani ethnicity, was admitted to the Emergency Room of our hospital for fever and multiple adenomegalies.
The patient referred a 20-d history of fever and the appearance of bilateral neck and axillary adenomegalies, showing no signs of improvement after a broad-spectrum antibiotic treatment prescribed by his general practitioner.
Past medical history did not reveal any relevant illness.
The patient was unmarried and had been working as a cook since he moved to Italy from Pakistan 7 years earlier.
Physical examination showed enlarged lymphadenopathy in the supradiaphragmatic regions, with the largest lesions measuring 2.5 cm in the left subclavian area and 3 cm in the left axilla. Moreover, the patient presented with erythematous and serpiginous nodules and plaques on the chest, with a cobblestone-like surface. Few faint erythematous macules and plaques were distributed near the nodules (Figures 1 and 2).
Laboratory data reported an increased white blood count (22600/µL) with neutrophilia (21000/µL), hypoalbuminemia (2.7 g/dL), increased hyperuricemia (12.6 mg/dL), LDH (230 U/L; normal range: 125-220 U/L), Beta 2 microglobulin (3.6 mg/L), C-reactive protein (CRP; 8.18 mg/dL) and erythrocyte sedimentation rate (ESR; 120 mm). A Quantiferon-TB gold assay revealed positive response to Micobacterium tuberculosis antigens.
An ultrasound scan of the described adenopathies revealed multiple round and hypoechogenic nodes; a chest X-ray did not show any significant finding. A whole-body CT scan revealed a dimensional increase of nodal lesions, the largest measuring 3 cm in the left supraclavicular area, 5 cm in the homolateral subclavian district and 4.3 cm in the right axilla. Positron emission tomography (PET) scan showed diffuse 18-fluorodeoxyglucose (FDG) uptake involving bilateral cervical, supraclavicular, subclavian, intrapectoral, axillary, mediastinal, celiac, retrocaval, para-aortic and iliac regions. A suspiciously increased uptake also involved skin thickening lesions in bilateral pectoral areas.
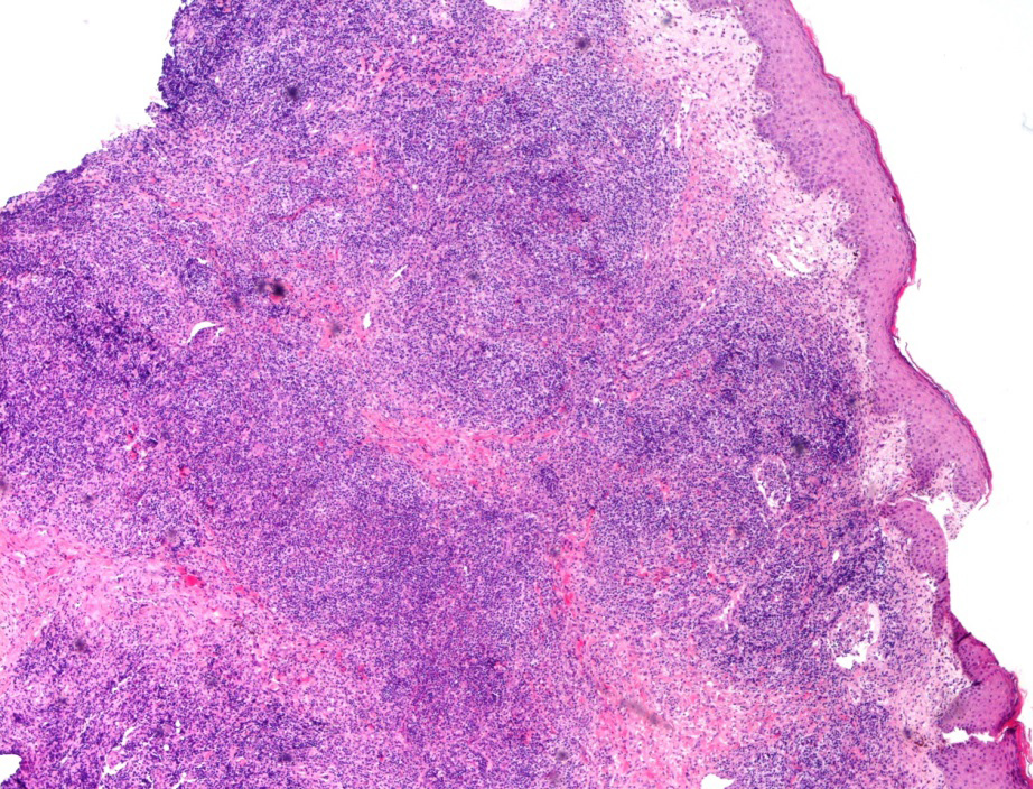
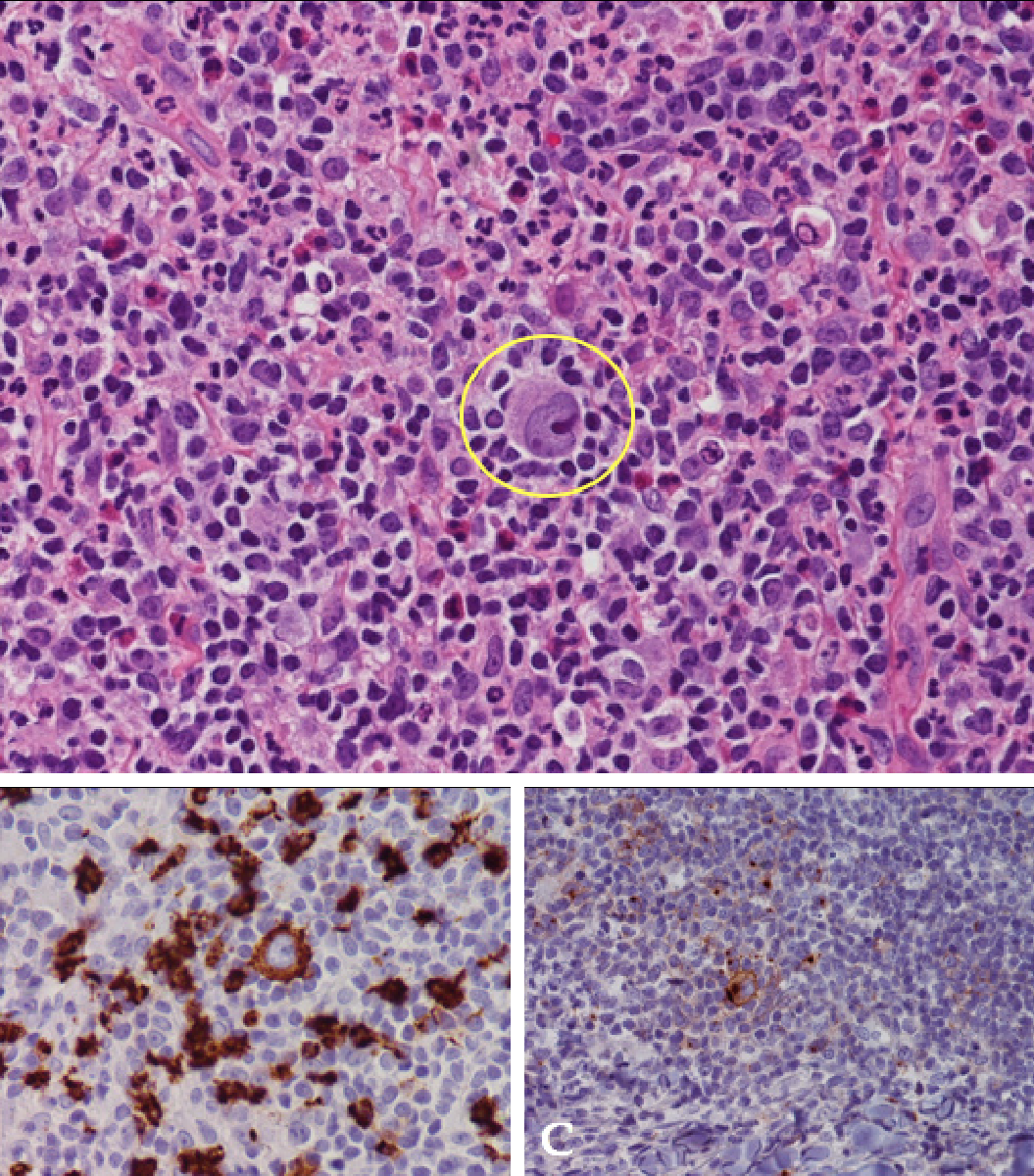
A lymph node biopsy was performed, revealing an immunohistochemical staining positive for CD30, CD15 +/-, PAX5 +/-, OCT2 -/+ and negative for CD20 and CD3, and a morphological pattern diagnostic for a mixed cellularity classical HL. A fluorescence in situ hybridization (FISH) assay excluded the presence of Epstein Barr virus (EBV) in analysed cells. The same neoplastic infiltration was detected in the cutaneous lesions through the execution of an incisional biopsy (Figures 3 and 4). Nodal tissue was also examined for microbiological testing, which excluded the presence of active tubercular infection.
In the clinical and epidemiological suspicion of an active tubercular infection, a 4-drug regimen including ethambutol, rifampicin, isoniazid and pyrazinamide was started. However, after two weeks the patient returned to the Emergency Room due to worsening of both fever and lymphadenomegalies. Dermoscopy of a cutaneous nodular lesion offered no specific clinical clues. A lymph node biopsy was diagnostic for HL. The bone marrow biopsy did not show lymphoma infiltration. The patient was classified as stage IV A with an International Prognostic Score of 5 points (age, sex, stage, leukocytosis and hypoalbuminemia) and started on conventional treatment with ABVD regimen (doxorubicin, bleomycin, vinblastine, dacarbazine).
To date, the patient has completed the first of six planned cycles, showing significant clinical improvement in both lymphadenomegalies and in skin lesions.
HL is a lymphoproliferative disorder usually characterised by supradiaphragmatic nodal involvement and infrequent extranodal localisations, generally developing due to contiguous spread (especially for bulky presentations). The involvement of distant organs is usually limited to spleen, liver, bone or lung, and rarely to other districts. The incidence of cutaneous lesions associated with HL infiltration have been reported as 0.5%-3.4% in several clinical records; lesions are often related to advanced stage disease[9,10]. Plaques, nodules, papules and ulcers are the most common findings[11]. Skin involvement might be explained by different mechanisms of tumour dissemination: the most common is thought to be the retrograde lymphatic diffusion starting from pathologic lymph nodes. Two other pathophysiological patterns are the direct extension due to contiguity and haematogenous spread[5,8]. Differential diagnosis between HL skin involvement and other histological subtypes such as mycosis fungoides, lymphomatoid papulosis, anaplastic large cell lymphoma and granulomatous slack skin disease must be performed[12]. We report a peculiar clinical presentation characterised by serpiginous nodular plaque lesions related to axillary lymphadenopathies in a patient presenting with a diagnostic delay probably related to poor sociocultural conditions. In fact, considering disease biology and size, it is plausible that adenopathies developed several months before ER admission. Furthermore, after the first clinical evaluation an active tubercular infection was suspected, due to fever, a positive Quantiferon-TB gold assay, increased blood CRP and ESR and epidemiological data identifying Pakistan as a country where tuberculosis remains endemic. Cutaneous tuberculosis is a rare but well-known finding that could have explained the skin lesions that we observed in our patient[13]. It is interesting to note that, despite the wide surface area covered by this cord-like lesion, the wall integrity of lesions was preserved without evidence of ulceration, which is a common finding in these clinically HL advanced conditions[8]. There is no specific treatment for cutaneous HL localisation: for advanced stage disease, the patient is prescribed six ABVD cycles. However, this schedule must be confirmed by the achievement of an early metabolic response, documented by a PET/CT scan after the first two chemotherapy cycles[14].
The patient has received the first chemotherapy cycle, with good tolerance to treatment, and has shown initial response both in the adenopathies and in the cutaneous localisations.
Manuscript source: Unsolicited manuscript.
Specialty type: Medicine, research and experimental
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hu SCS, Vento S S-Editor: Ma YJ L-Editor: A E-Editor: Zhou BX
| 1. | Ansell SM. Hodgkin Lymphoma: Diagnosis and Treatment. Mayo Clin Proc. 2015;90:1574-1583. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | Smith A, Crouch S, Lax S, Li J, Painter D, Howell D, Patmore R, Jack A, Roman E. Lymphoma incidence, survival and prevalence 2004-2014: sub-type analyses from the UK's Haematological Malignancy Research Network. Br J Cancer. 2015;112:1575-1584. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 221] [Cited by in F6Publishing: 275] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 3. | Connors JM. Clinical manifestations and natural history of Hodgkin's lymphoma. Cancer J. 2009;15:124-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Pranteda G, Osti MF, Cox MC, Cacchi C, Carlesimo M, Grimaldi M, Fidanza L, Bartolazzi A. Primary cutaneous Hodgkin lymphoma. J Am Acad Dermatol. 2010;63:e52-e53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Introcaso CE, Kantor J, Porter DL, Junkins-Hopkins JM. Cutaneous Hodgkin's disease. J Am Acad Dermatol. 2008;58:295-298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Bartus CL, Parker SR. Hodgkin lymphoma presenting as generalized pruritus in an adolescent. Cutis. 2011;87:169-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Koch K, Patel M, Pather S, Modi D. Primary cutaneous Hodgkin lymphoma: a rare disease variant and review of the literature. J Case Rep Stud. 2016;4:204. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Hayes TG, Rabin VR, Rosen T, Zubler MA. Hodgkin's disease presenting in the skin: case report and review of the literature. J Am Acad Dermatol. 1990;22:944-947. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | White RM, Patterson JW. Cutaneous involvement in Hodgkin's disease. Cancer. 1985;55:1136-1145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 10. | Smith JL, Butler JJ. Skin involvement in Hodgkin's disease. Cancer. 1980;45:354-361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 11. | Pagliaro JA, White SI. Specific skin lesions occurring in a patient with Hodgkin's lymphoma. Australas J Dermatol. 1999;40:41-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Cerroni L, Goteri G. Differential diagnosis between cutaneous lymphoma and pseudolymphoma. Anal Quant Cytol Histol. 2003;25:191-198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb). 2015;95:629-638. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 14. | Johnson P, Federico M, Kirkwood A, Fosså A, Berkahn L, Carella A, d'Amore F, Enblad G, Franceschetto A, Fulham M, Luminari S, O'Doherty M, Patrick P, Roberts T, Sidra G, Stevens L, Smith P, Trotman J, Viney Z, Radford J, Barrington S. Adapted Treatment Guided by Interim PET-CT Scan in Advanced Hodgkin's Lymphoma. N Engl J Med. 2016;374:2419-2429. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 574] [Cited by in F6Publishing: 533] [Article Influence: 66.6] [Reference Citation Analysis (0)] |