Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12345
Peer-review started: July 23, 2022
First decision: October 12, 2022
Revised: October 19, 2022
Accepted: November 2, 2022
Article in press: November 2, 2022
Published online: November 26, 2022
Since Kambin experimentally induced arthroscopy to treat herniated nucleus pulposus, percutaneous endoscopic lumbar discectomy (PELD) has been developed. The branch of the segmental artery around the neural foramen may be damaged during PELD using the transforaminal approach. We report 2 rare cases in which segmental artery injury that occurred during PELD was treated with emergency embolization.
In case 1, a 31-year-old man was transferred to our emergency department with left lower quadrant abdominal pain after PELD at a local hospital. Lumbar spine magnetic resonance imaging after the surgery showed a hematoma of the left retroperitoneal area and the psoas muscle area. Under suspicion of vascular injury, arteriography was performed. Pseudoaneurysm and blood leakage from the left 4th lumbar segmental artery into the abdominal cavity were identified. Emergency transarterial embolization was performed using fibered microcoils for bleeding of the segmental artery. In case 2, a 75-year-old woman was transferred to our emergency department with low blood pressure, right flank pain, and drowsy mental status after PELD at a local hospital. When the patient arrived at the emergency room, the blood pressure decreased from 107/55 mmHg to 72/47 mmHg. Low blood pressure persisted. Under suspicion of vessel injury, arteriography was performed, and the right 4th lumbar segmental artery rupture was confirmed. Emergency transarterial embolization was performed for bleeding of segmental artery.
We were able to find the bleeding focus by angiography and treat the injury of the segmental artery successfully through emergency transarterial embolization.
Core Tip: The branch of the segmental artery around the neural foramen may be damaged during percutaneous endoscopic lumbar discectomy using the transforaminal approach. When segmental artery rupture is suspected, angiography is helpful in finding the bleeding focus, and emergency embolization is considered an effective treatment method. In our 2 cases, clear bleeding focus was found by angiography, and the bleeding was controlled successfully through emergency transarterial embolization.
- Citation: Cho WJ, Kim KW, Park HY, Kim BH, Lee JS. Segmental artery injury during transforaminal percutaneous endoscopic lumbar discectomy: Two case reports. World J Clin Cases 2022; 10(33): 12345-12351
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12345.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12345
After the endoscope was developed, it began to be actively used in the field of spinal surgery. Since Pan et al[1] experimentally induced arthroscopy to treat herniated nucleus pulposus, percutaneous endoscopic lumbar discectomy (PELD) has been developed. PELD has several advantages, including less paravertebral muscle injury, preservation of bony structure, and rapid recovery[2]. On the other hand, surgery-related complications of PELD including dural tear, intervertebral infection, hypoesthesia, bleeding, and recurrence are common[1]. Lumbar segmental arteries originate from the aorta and primarily distribute on the lateral surface of the vertebrae, forming an extensive arterial network that feeds the nerve root, vertebral body, and associated muscles or extradural structures[3]. The segmental artery branches into the intercostal branch, muscular branch, and spinal artery near the neural foramen[4]. Of these, spinal arteries enter the vertebral canal and divide into postcentral, prelaminar, and radicular branches[5]. The branch of the segmental artery around the neural foramen may be damaged during PELD using a transforaminal approach. Here we report 2 rare cases of segmental artery injury during PELD.
Case 1: A 31-year-old man presented with left lower quadrant abdominal pain after PELD at a local hospital.
Case 2: A 75-year-old woman presented with low blood pressure, right flank pain, and drowsy mental status after PELD at a local hospital.
Case 1: He was transferred to the emergency department at our hospital 17 h after surgery. When the patient arrived at the emergency room, the abdominal pain worsened.
Case 2: She was transferred to the emergency department of our hospital 8 h after surgery. When the patient arrived at the emergency room, her blood pressure decreased from 107/55 mmHg to 72/47 mmHg. Her low blood pressure persisted.
Case 1: The patient was medically healthy without taking any medications.
Case 2: The patient had diabetes mellitus, hypertension, and hyperlipidemia as comorbidities.
Cases 1 and 2: There were no specific family health histories.
Case 1: Tenderness in the left lower quadrant area was observed. He had no neurologic deficit.
Case 2: There was no neurologic deficit other than the right flank pain.
Case 1: When the patient arrived at the emergency room, laboratory investigations revealed low levels of hemoglobin (11.9 g/dL, normal range: 14.0-18.0 g/dL) with low levels of hematocrit (35.0%, normal range: 42.0%-52.0%). White blood cell count was 10.65 × 109/L (normal range: 4.0-10.0 × 109/L), and platelet count was 170 × 109/L (normal range: 150-450 × 109/L). At 2 h after arrival, follow-up laboratory investigations showed rapidly decreasing hemoglobin (10.0 g/dL) and hematocrit (29.2%).
Coagulation function test revealed: prothrombin time (PT), 10.3 s (normal range: 9.7-13.3 s); PT%, 106.1% (normal range: 77%-120%); international normalized ratio, 0.97 (normal range: 0.88-1.20); and activated partial thromboplastin time, 24.9 s (normal range: 23.1-37.3 s). These results were all within normal ranges.
Case 2: When the patient arrived at the emergency room, laboratory investigations revealed low levels of hemoglobin (9.4 g/dL, normal range: 12.0-16.0 g/dL) with low levels of hematocrit (27.5%, normal range: 37.0%-47.0%). White blood cell count was 15.52 × 109/L (normal range: 4.0-10.0 × 109/L), and platelet count was 170 × 109/L (normal range: 150 - 450 × 109/L).
Coagulation function test revealed: PT, 10.7 s (normal range: 9.7-13.3s); PT%, 93.4% (normal range: 77%-120%); international normalized ratio, 1.03 (normal range: 0.88-1.20); and activated partial thromboplastin time: 20.4 s (normal range: 23.1-37.3 s). These results were all within normal ranges.
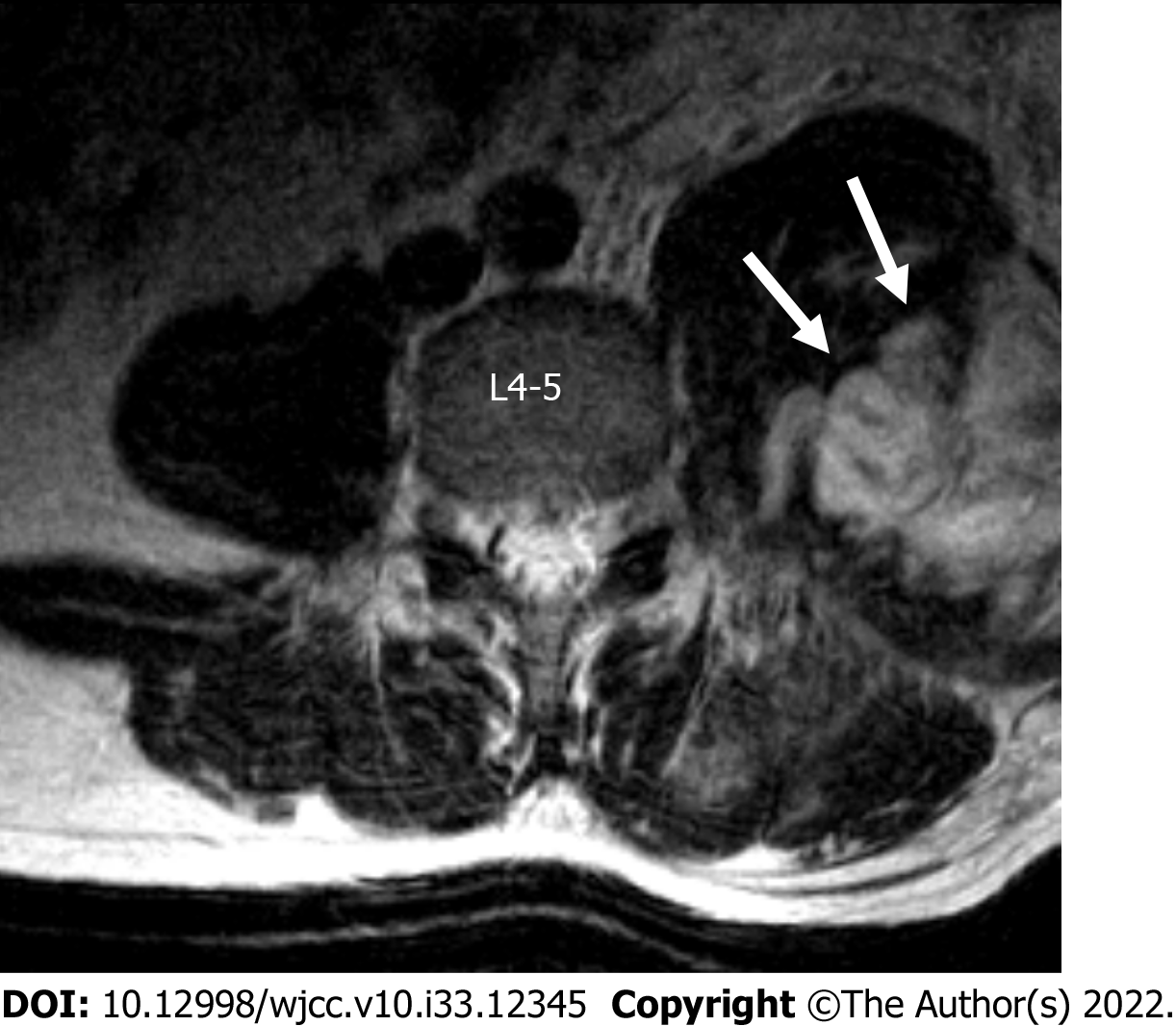
Case 1: Lumbar spine magnetic resonance imaging after the surgery showed hematoma of the left retroperitoneal area and the psoas muscle area (Figures 1 and 2).
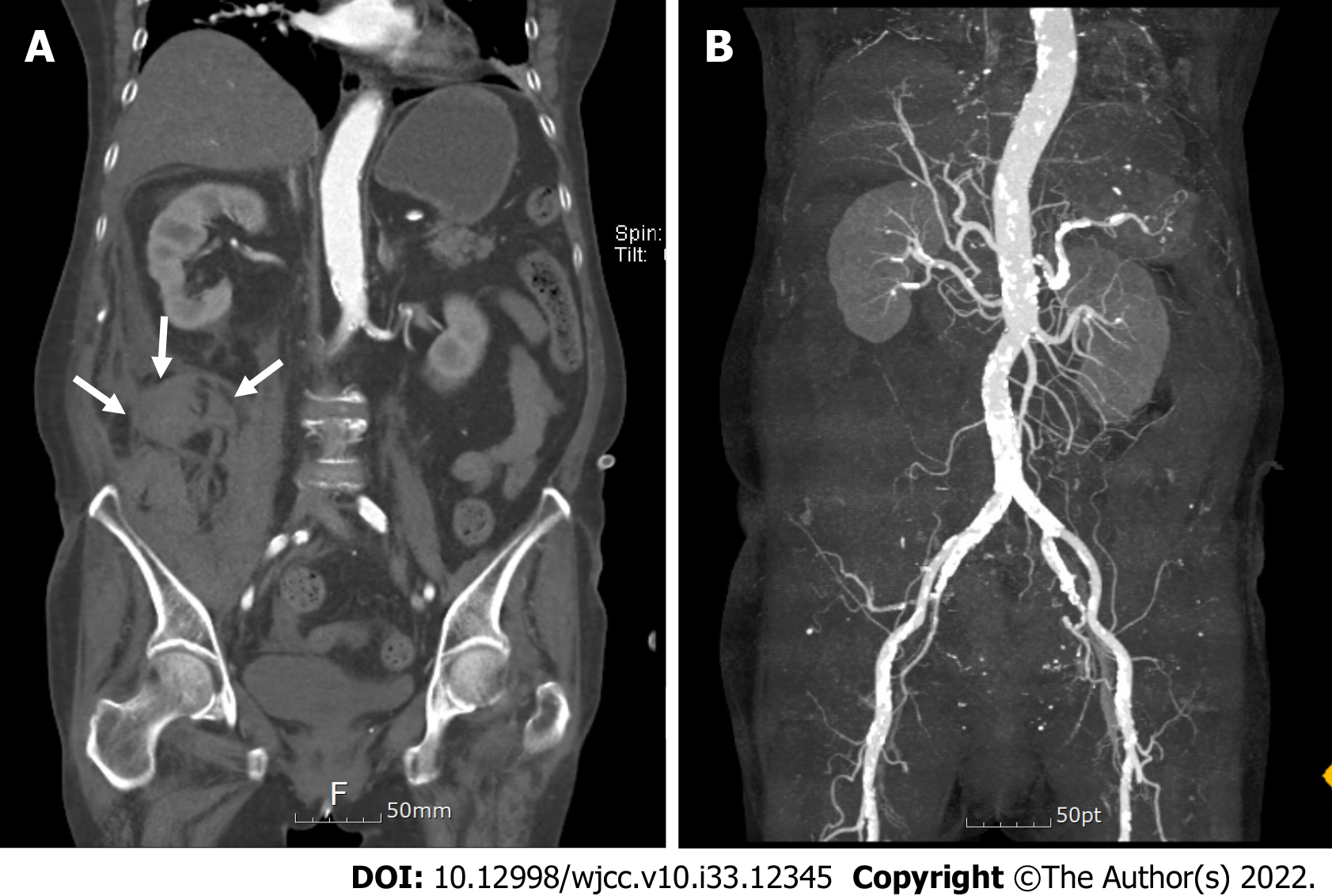
Case 2: Computed tomography scan of the abdomen aorta showed hemorrhage in the right retroperitoneal area without a clear bleeding focus (Figure 3A and B).
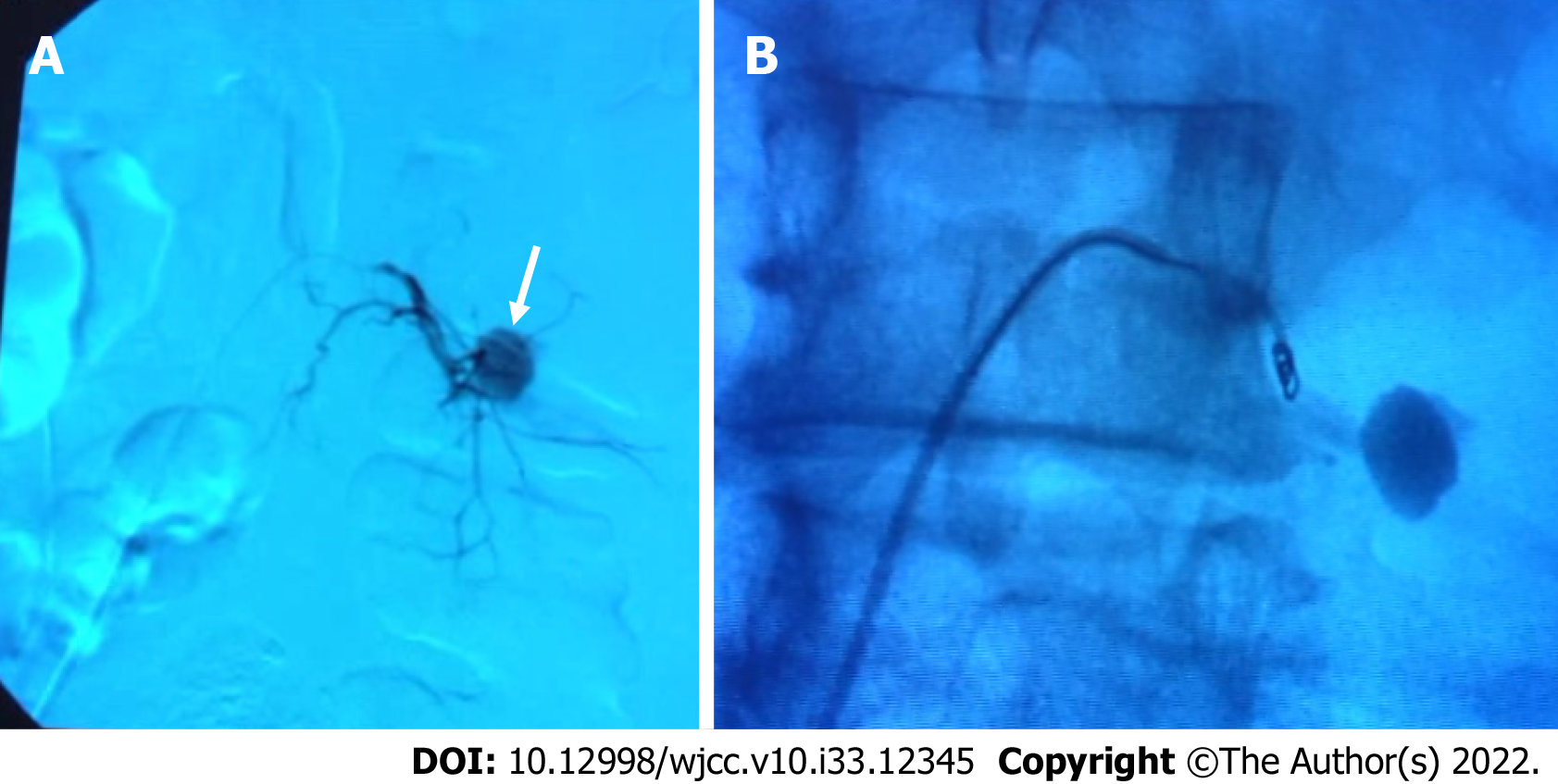
Pseudoaneurysm and blood leakage from the left 4th lumbar segmental artery into the abdominal cavity were identified by arteriography (Figure 2A).
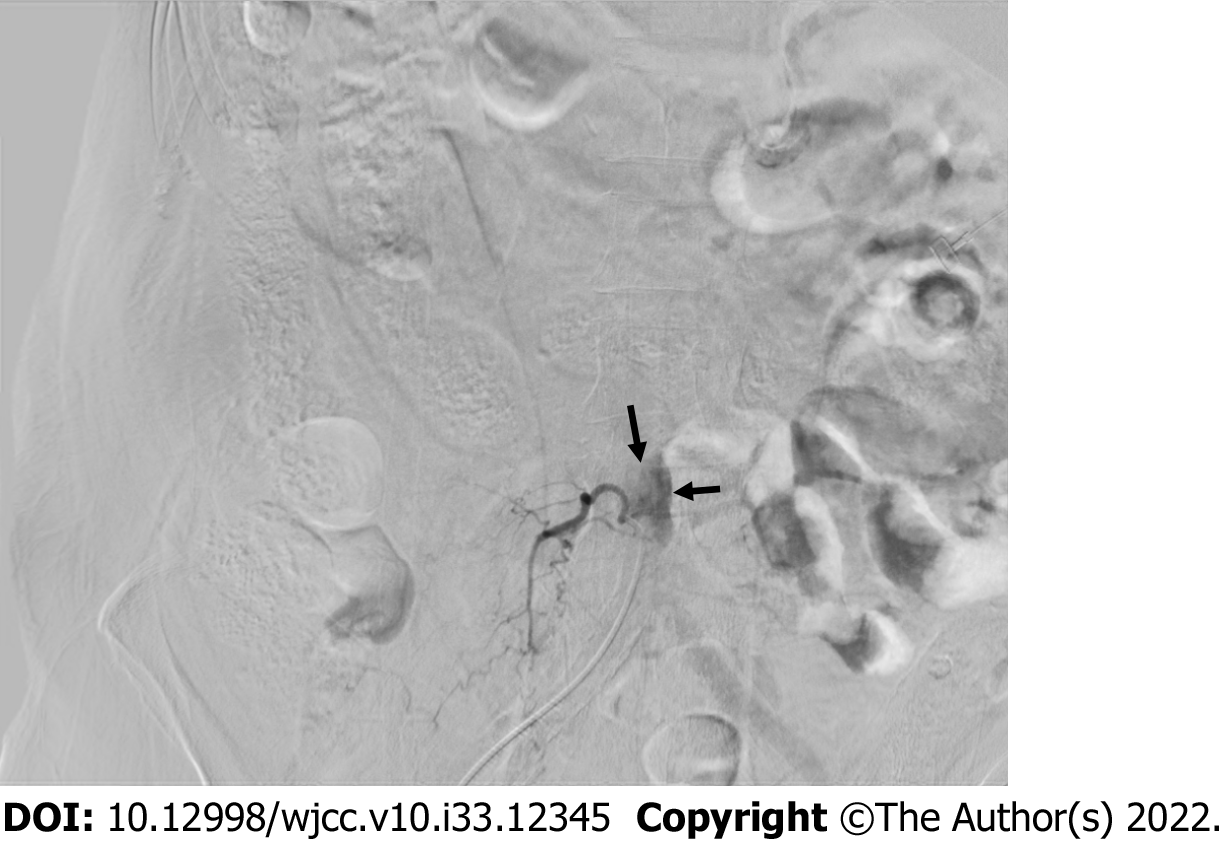
The right 4th lumbar segmental artery rupture was confirmed by arteriography (Figure 4).
Emergency transarterial embolization was performed using fibered microcoils for bleeding of the segmental artery (Figure 2B).
After the embolization, the pain improved. The patient was discharged in a tolerable state in the 1st wk after the procedure.
After the procedure, the patient’s flank pain improved. Her vital signs were stable. The patient was discharged in a tolerable state on the 4th d after the procedure.
PELD can be broadly divided into percutaneous endoscopic transforaminal discectomy and per
We found a total of 7 cases of vessel injury that occurred during PELD[7-10]. In 6 of the 7 cases, vessel injury occurred during a transforaminal approach. Our 2 cases also had a segmental artery injury during transforaminal PELD. The segmental artery branches into the intercostal branch, muscular branch, and spinal artery near the neural foramen. Accordingly, during a transforaminal approach, the guide wire may come close to the branch of the segmental artery, causing injury. During guide wire insertion before reaching the disc, the guide tip should be placed behind the posterior vertebral line to avoid damage to the segmental artery terminal branch[7]. In the extraforaminal area, the arterial branches are complex, and care must be taken because vascular damage may occur during exploration[7]. If blood vessel damage is found, hemostasis can be attempted by electrocautery or compressing a gelatin sponge. If bleeding persists even after trying the above method, an artery injury is suspected, and transarterial embolization can be performed as in our cases. Complications of transarterial embolization include contrast reaction, vascular injury, and coil migration, but the incidence is known to be low[11].
In the literature, patients have complained of flank pain and inguinal pain as symptoms of vessel injury. However, in our cases 1 patient complained of abdominal pain and 1 patient complained of flank pain. Of the 7 cases reported so far, only 2 cases on which angiography was performed could detect an accurate bleeding focus in a segmental artery. For the other 5 cases, both computed tomography and magnetic resonance imaging were performed. However, no bleeding focus was found because angiography was not performed. Of the 5 cases where no bleeding focus was found, 3 cases received conservative treatment and 2 cases underwent abdominal exploration (Table 1). In our 2 cases, a clear bleeding focus was found by angiography, and the bleeding was controlled successfully through emergency transarterial embolization. Therefore, when segmental artery rupture is suspected, angiography is helpful in finding the bleeding focus, and emergency embolization is considered an effective treatment method.
| Ref. | Age | Sex | HNP level | HNP operation | Symptom | Diagnosis | Treatment |
| Kim et al[8], 2009 | 60 | F | L4-5 | PELD | Flank and leg pain, hip flexion weakness, low BP | Psoas hematoma | Transfusion |
| Ahn et al[7], 2009 | 64 | M | L4-5 | Trans foraminal PELD | Inguinal and flank pain | Retroperitoneal hematoma | Retroperitoneal exploration |
| Ahn et al[7], 2009 | 31 | F | L4-5 | Trans foraminal PELD | Inguinal and thigh pain | Retroperitoneal hematoma | Paraspinal and retroperitoneal exploration |
| Ahn et al[7], 2009 | 34 | M | L4-5 | Trans foraminal PELD | Inguinal and thigh pain | Psoas hematoma | Conservative |
| Ahn et al[7], 2009 | 41 | F | L3-4, 4-5 | Trans foraminal PELD | Inguinal pain, hip flexion weakness | Retroperitoneal hematoma | Conservative |
| Wang et al[10], 2018 | 64 | F | L3-4 | Trans foraminal PELD | Intraoperative bleeding | Lumbar artery injury | Coil embolization |
| Panagiotopoulos et al[9], 2019 | 39 | M | L4-5 | Trans foraminal PELD | Flank pain | Segmental artery pseudoaneurysm | Coil embolization |
We report 2 rare cases of segmental artery injury during transforaminal PELD. We were able to find the bleeding focus by angiography and treat the injury of the segmental artery successfully through emergency transarterial embolization.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Zhang JW, China; Yuan HJ, China S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Pan M, Li Q, Li S, Mao H, Meng B, Zhou F, Yang H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician. 2020;23:49-56. [PubMed] [Cited in This Article: ] |
| 2. | Choi KC, Lee JH, Kim JS, Sabal LA, Lee S, Kim H, Lee SH. Unsuccessful percutaneous endoscopic lumbar discectomy: a single-center experience of 10,228 cases. Neurosurgery. 2015;76:372-80; discussion 380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 122] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 3. | Beckman JM, Vincent B, Park MS, Billys JB, Isaacs RE, Pimenta L, Uribe JS. Contralateral psoas hematoma after minimally invasive, lateral retroperitoneal transpsoas lumbar interbody fusion: a multicenter review of 3950 lumbar levels. J Neurosurg Spine. 2017;26:50-54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Shimizu S, Tanaka R, Kan S, Suzuki S, Kurata A, Fujii K. Origins of the segmental arteries in the aorta: an anatomic study for selective catheterization with spinal arteriography. AJNR Am J Neuroradiol. 2005;26:922-928. [PubMed] [Cited in This Article: ] |
| 5. | Zhao Q, Zhong E, Shi B, Ding Z, Jin D, Li Q. Clinical Anatomy and Possible Clinical Significance of the Postcentral Branches of Spinal Arteries in the L1-L5 Levels. Clin Spine Surg. 2020;33:328-332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Huang Y, Yin J, Sun Z, Song S, Zhuang Y, Liu X, Du S, Rui Y. Percutaneous endoscopic lumbar discectomy for LDH via a transforaminal approach versus an interlaminar approach: a meta-analysis. Orthopade. 2020;49:338-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ahn Y, Kim JU, Lee BH, Lee SH, Park JD, Hong DH, Lee JH. Postoperative retroperitoneal hematoma following transforaminal percutaneous endoscopic lumbar discectomy. J Neurosurg Spine. 2009;10:595-602. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Kim HS, Ju CI, Kim SW, Kim JG. Huge Psoas Muscle Hematoma due to Lumbar Segmental Vessel Injury Following Percutaneous Endoscopic Lumbar Discectomy. J Korean Neurosurg Soc. 2009;45:192-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Panagiotopoulos K, Gazzeri R, Bruni A, Agrillo U. Pseudoaneurysm of a segmental lumbar artery following a full-endoscopic transforaminal lumbar discectomy: a rare approach-related complication. Acta Neurochir (Wien). 2019;161:907-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Wang Y, Ai P, Zhan G, Shen B. Lumbar Artery Injury during Transforaminal Percutaneous Endoscopic Lumbar Discectomy: Successful Treatment by Emergent Transcatheter Arterial Embolization. Ann Vasc Surg. 2018;53:267.e11-267.e14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Bauer JR, Ray CE. Transcatheter arterial embolization in the trauma patient: a review. Semin Intervent Radiol. 2004;21:11-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |