Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1116
Peer-review started: July 10, 2021
First decision: September 28, 2021
Revised: October 11, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: January 21, 2022
Since 2006, introducing a tibial intramedullary nail via the suprapatellar approach has been established; however, nail removal must be carried out using classic infrapatellar access, which can lead to complications. Here, we report a new method to remove the intramedullary nail through the original suprapatellar incision.
A 39-year-old man was hit by a vehicle in 2019. He was immobilized with a 10-mm × 330-mm tibial intramedullary nail via the suprapatellar approach due to left middle tibial fracture. Two years later, the patient requested for the implant to be removed. We used a new method to remove the tibial intramedullary nail through the original suprapatellar incision, and the operation went smoothly.
This case report indicates that suprapatellar access can be used to remove the intramedullary nail via the original incision without infrapatellar access, thus avoiding surgical complications.
Core Tip: A 39-year-old man was immobilized with a 10-mm × 330-mm tibial intramedullary nail via the suprapatellar approach due to left middle tibial fracture. The end cap of the nail was purposely not inserted. Two years later, we used a novel method to remove the tibial intramedullary nail through the original suprapatellar incision.
- Citation: He M, Li J. New method to remove tibial intramedullary nail through original suprapatellar incision: A case report. World J Clin Cases 2022; 10(3): 1116-1121
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1116.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1116
The advantages of intramedullary nail internal fixation, such as small trauma, central fixation, and closed reduction, are consistent with the biological osteosynthesis concept; thus, intramedullary nail internal fixation has become the gold-standard treatment for tibial shaft fracture[1].
Removal of the tibial intramedullary nail via the infrapatellar approach is simple, and it is performed under direct vision through the original incision. Thus, researchers tend to use the infrapatellar approach to remove the internal fixation inserted via the suprapatellar approach[2]; however, with this approach, new scars form, and the patellar ligament and the infrapatellar fat pad can become damaged[3].
The other option is to remove the tibial intramedullary nail via the suprapatellar approach. However, this method remains controversial because there are many difficulties in using the original incision to remove the internal fixation. In this paper, a quick and simple method of nail extraction via the original suprapatellar incision is proposed. To the best of our knowledge, this is the first report of this type of removal.
A 33-year-old man requested for the implant to be removed.
The patient who was hit by a car in 2019 had a history of multiple fractures. These fractures, including left mid-tibial fracture, were fixed with a 10-mm × 330-mm suprapellar tibial nail. The end cap of the nail was purposely not inserted. Two years later, the patient requested for the implant to be removed.
The patient had a history of internal fixation.
The patient had no genetic or familial disease history.
Multiple surgical scars were visible on the left calf, and there was no sign of limited motion in the left knee joint.
No abnormalities were observed on preoperative examination.
An X-ray examination showed that the broken end of the tibia had bony union (Figure 1).
The patient’s final diagnosis was bony union after multiple fractures.
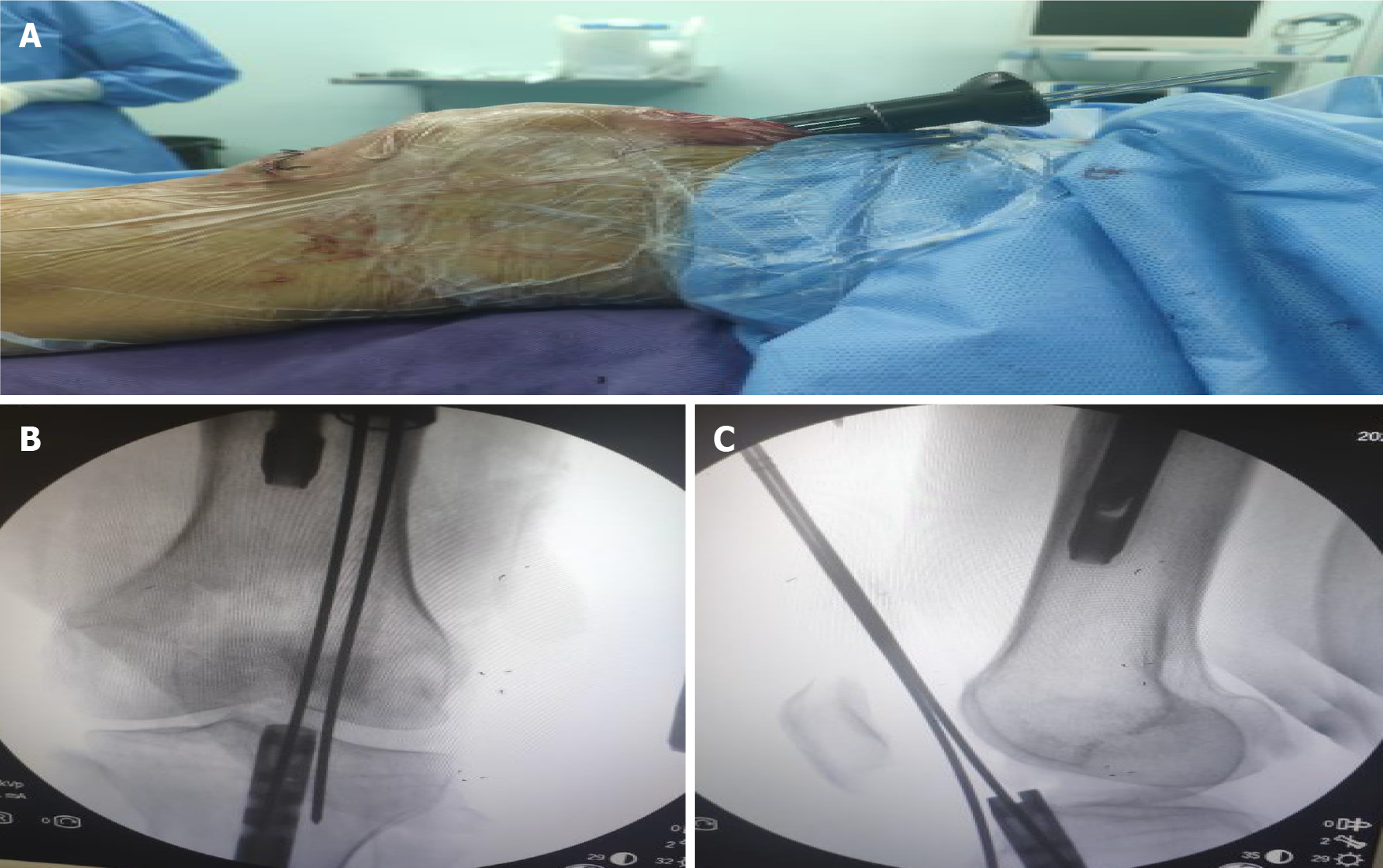
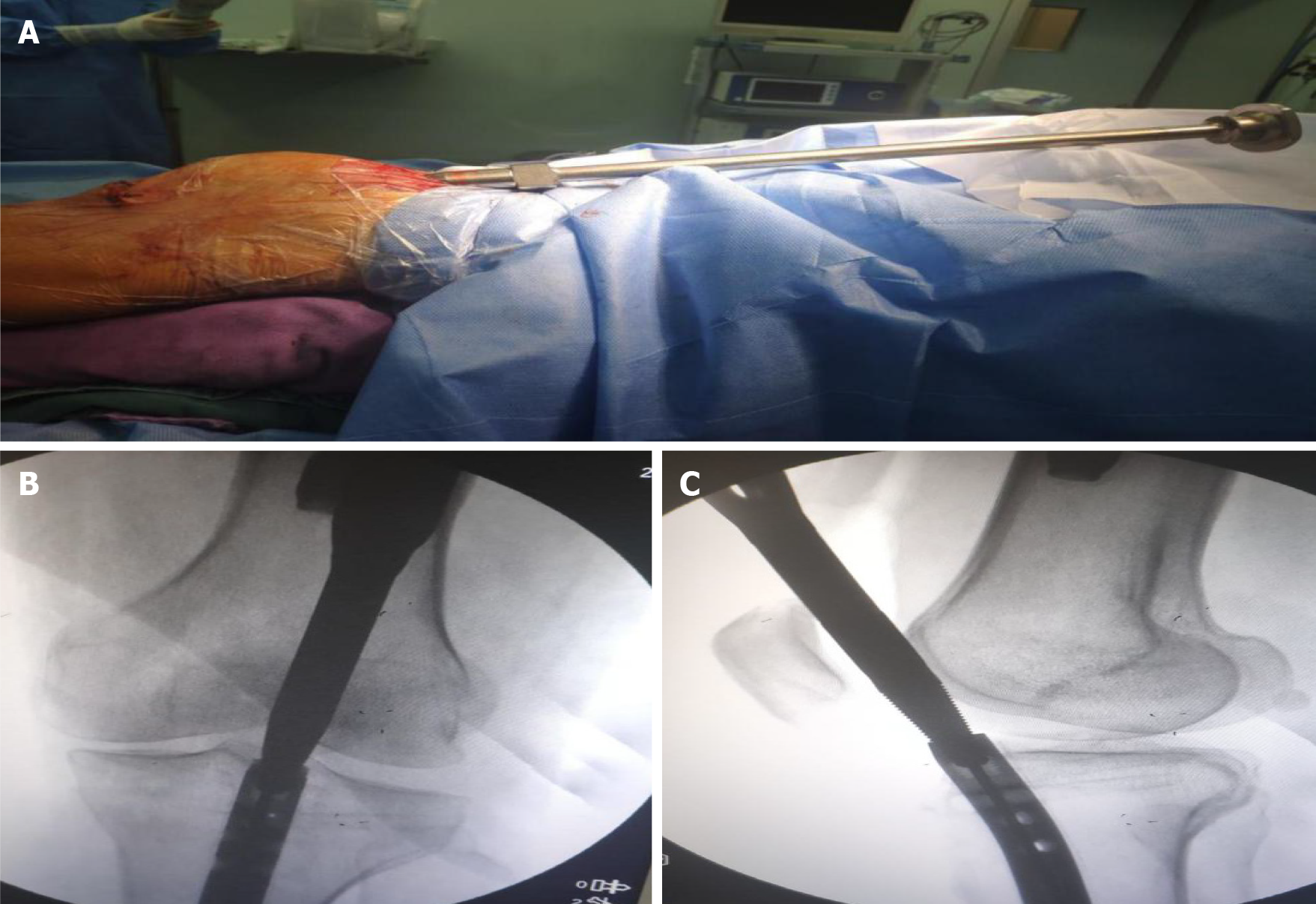
The patient was examined before surgery and had no contraindications. After administering epidural anesthesia, the proximal locking nail was removed. Then, the knee was bent 30°, and a multi-holed guide pin sleeve was fine-tuned to allow a 2-mm guide needle to be accurately inserted into the cavity of the intramedullary nail with a depth of at least 2–3 cm via the original suprapatellar incision. The results were confirmed by intraoperative X-ray (Figure 2). A hollow jig was used to screw the end of the nail along the guide needle. This process accurately removed the bone on top of the nail without damaging surrounding structures, such as the meniscus and ligaments. After the jig was screwed into the end of the intramedullary nail and tightened, intraoperative fluoroscopy was used for confirmation (Figure 3). The proximal and distal locking nails were removed, and the intramedullary nail was retracted using a mallet (Figure 4).
Two weeks postoperatively, the patient’s wound had healed well. At the 4-mo postoperative follow-up, the patient did not complain of pain in the left knee joint. The left knee could extend 0° and flex 120° (Figure 5). The Kujala score was 95 on the left knee.
Tibial intramedullary nail placement can be achieved by both suprapatellar and infrapatellar access. The suprapatellar approach has more advantages than the infrapatellar approach[4-8]; however, how best to remove the nail via the original suprapatellar incision used for nail insertion is uncertain.
When using the traditional method to remove the intramedullary nail through the original suprapatellar incision, it is necessary to first remove the bone above the intramedullary nail with a hollow drill, remove the end cap, and take out the end of the intramedullary nail and screw it into the target device to remove the intramedullary nail. Because the whole process is not performed under direct vision, the operation is difficult and time-consuming. The main difficulty lies in how to accurately remove the bone above the intramedullary nail. If care is not exercised, the meniscus and anterior and posterior cruciate ligaments can become damaged. The cap should then be safely removed without being lost in the joint space. Therefore, most surgeons have no choice but to use the infrapatellar access to remove the internal fixation, but this often leads to new scar formation. Moreover, surgical incision can also damage the saphenous nerve, the patellar ligament, and the infrapatellar fat pad, resulting in a high probability of postoperative knee pain.
A previous study has shown that the end cap of an intramedullary nail stops bony in-growth of tissue[9]. To facilitate the method presented in this paper, the end cap was not used in the initial nail placement, and bony in-growth of tissue enclosed the end of the nail. To remove the tibial intramedullary nail, a guide needle was inserted into the cavity of the intramedullary nail. The results were confirmed by intraoperative X-ray. A hollow jig was used to screw the end of the nail along the guide needle. This process accurately removed the bone on top of the nail. Thus, the difficulty in removing the nail via the original incision was greatly reduced. The whole process was easy, and no special tools were needed. Due to the use of a sleeve during surgery to protect important tissues within the joint, the likelihood of damage to the patellofemoral joint was greatly reduced.
However, this novel approach has some potential limitations that should be noted. First, removal of the bone above the intramedullary nail may lead to possible entry of large bone fragments into the articular cavity. Second, after intramedullary nail removal, the intramedullary content entering the joint cavity may lead to joint cavity extravasation and increase the risk of infection.
In this study, removal of the intramedullary nail via the original suprapatellar incision was simple and reliable, did not require special equipment, and did not require infrapatellar access, which reduced the likelihood of complications.
The authors would like to thank the patient for providing consent for publication of this case report and accompanying images.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shekouhi R S-Editor: Liu M L-Editor: Wang TQ P-Editor: Liu M
| 1. | Bode G, Strohm PC, Südkamp NP, Hammer TO. Tibial shaft fractures - management and treatment options. A review of the current literature. Acta Chir Orthop Traumatol Cech. 2012;79:499-505. [PubMed] [Cited in This Article: ] |
| 2. | Noia G, Fulchignoni C, Marinangeli M, Maccauro G, Tamburelli FC, De Santis V, Vitiello R, Ziranu A. Intramedullary nailing through a suprapatellar approach. Evaluation of clinical outcome after removal of the device using the infrapatellar approach. Acta Biomed. 2018;90:130-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 6] [Reference Citation Analysis (0)] |
| 3. | Katsoulis E, Court-Brown C, Giannoudis PV. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br. 2006;88:576-580. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 126] [Article Influence: 7.0] [Reference Citation Analysis (1)] |
| 4. | Chan DS, Serrano-Riera R, Griffing R, Steverson B, Infante A, Watson D, Sagi HC, Sanders RW. Suprapatellar Versus Infrapatellar Tibial Nail Insertion: A Prospective Randomized Control Pilot Study. J Orthop Trauma. 2016;30:130-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Wang C, Chen E, Ye C, Pan Z. Suprapatellar vs infrapatellar approach for tibia intramedullary nailing: A meta-analysis. Int J Surg. 2018;51:133-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Gao Z, Han W, Jia H. Suprapatellar vs infrapatellar intramedullary nailing for tibal shaft fractures: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97:e10917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Chen X, Xu HT, Zhang HJ, Chen J. Suprapatellar vs infrapatellar intramedullary nailing for treatment of tibial shaft fractures in adults. Medicine (Baltimore). 2018;97:e11799. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Williamson M, Iliopoulos E, Williams R, Trompeter A. Intra-operative fluoroscopy time and radiation dose during suprapatellar tibial nailing vs infrapatellar tibial nailing. Injury. 2018;49:1891-1894. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | Underwood J, Chakrabarti AJ. A 'Seldinger' method to facilitate accurate placement of an end cap following femoral nailing. Ann R Coll Surg Engl. 2006;88:225-226. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |