Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.563
Peer-review started: July 31, 2021
First decision: October 22, 2021
Revised: November 8, 2021
Accepted: December 10, 2021
Article in press: December 10, 2021
Published online: January 14, 2022
Irritable bowel syndrome (IBS) is a common functional bowel disease that shares features with many organic diseases and cannot be accurately diagnosed by symptom-based criteria. Alarm symptoms have long been applied in the clinical diagnosis of IBS. However, no study has explored the predictive value of alarm symptoms in suspected IBS patients based on the latest Rome IV criteria.
To investigate the predictive value of alarm symptoms in suspected IBS patients based on the Rome IV criteria.
In this multicenter cross-sectional study, we collected data from 730 suspected IBS patients evaluated at 3 tertiary care centers from August 2018 to August 2019. Patients with IBS-like symptoms who completed colonoscopy during the study period were initially identified by investigators through medical records. Eligible patients completed questionnaires, underwent laboratory tests, and were assigned to the IBS or organic disease group according to colonoscopy findings and pathology results (if a biopsy was taken). Independent risk factors for organic disease were explored by logistic regression analysis, and the positive predictive value (PPV) and missed diagnosis rate were calculated.
The incidence of alarm symptoms in suspected IBS patients was 75.34%. Anemia [odds ratio (OR) = 2.825, 95% confidence interval (CI): 1.273-6.267, P = 0.011], fecal occult blood [OR = 1.940 (95%CI: 1.041-3.613), P = 0.037], unintended weight loss (P = 0.009), female sex [OR = 0.560 (95%CI: 0.330-0.949), P = 0.031] and marital status (P = 0.030) were independently correlated with organic disease. The prevalence of organic disease was 10.41% in suspected IBS patients. The PPV of alarm symptoms for organic disease was highest for anemia (22.92%), fecal occult blood (19.35%) and unintended weight loss (16.48%), and it was 100% when these three factors were combined. The PPV and missed diagnosis rate for diagnosing IBS were 91.67% and 74.77% when all alarm symptoms were combined with Rome IV and 92.09% and 34.10% when only fecal occult blood, unintended weight loss and anemia were combined with Rome IV, respectively.
Anemia, fecal occult blood and unintended weight loss have high predictive value for organic disease in suspected IBS patients and can help identify patients requiring further examination but are not recommended as exclusion criteria for IBS.
Core Tip: The diagnosis of irritable bowel syndrome (IBS) depends on symptom-based criteria, but the accuracy of these criteria is poor. For suspected IBS patients meeting the Rome IV criteria, considering alarm symptoms does not significantly improve the positive predictive value for diagnosing IBS. However, alarm symptoms can help identify patients with organic disease; in particular, fecal occult blood, unintended weight loss and anemia have a high predictive value for organic disease. The presence of those alarm symptoms suggests that further examination may be needed, but they are not recommended as exclusion criteria for IBS.
- Citation: Yang Q, Wei ZC, Liu N, Pan YL, Jiang XS, Tantai XX, Yang Q, Yang J, Wang JJ, Shang L, Lin Q, Xiao CL, Wang JH. Predictive value of alarm symptoms in Rome IV irritable bowel syndrome: A multicenter cross-sectional study. World J Clin Cases 2022; 10(2): 563-575
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/563.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.563
As a functional bowel disease (FBD), irritable bowel syndrome (IBS) is characterized by recurrent abdominal pain with changes in bowel habits[1]. The most recent study showed that the prevalence of IBS is 4.6%[2] and ranges from 6.8% to 33.3% in Asia[3]. Although IBS does not directly increase mortality, it significantly affects patients' quality of life, the results in the waste of medical resources and increases social burden[4,5].
The diagnosis of IBS depends on symptom-based criteria. Due to a lack of reliable diagnostic tests and specific biomarkers and overlap between symptoms of IBS and those of multiple organic diseases, the accuracy of symptom-based criteria is poor in practical applications[6,7]. Guidelines and consensus[8-10] advocate positive diagno
This multicenter cross-sectional study was conducted at three academic urban tertiary care centers from August 2018 to August 2019. These included the Second Affiliated Hospital of Xi'an Jiaotong University, Tangdu Hospital of Air Force Medical University and the Affiliated Hospital of Northwest University (Xi’an No. 3 Hospital). Patients came to the centers with gastrointestinal symptoms, and they were initially evaluated and managed by gastroenterologists. Those with IBS-like symptoms who completed colonoscopy during the study period were identified by investigators through medical records. Then, investigators further called eligible patients to confirm whether they met the inclusion and exclusion criteria and whether they had completed a routine fecal exam, routine blood exam and fecal occult blood test. Patients who had undergone blood and stool tests within 6 mo were not re-examined. Otherwise, eligible patients were required to finish these tests. Detailed information on qualified candidates was obtained via telephone and a questionnaire (paper questionnaires were handed out face-to-face or sent as an electronic version via WeChat). Oral informed consent was acquired from all included patients. This study was approved by the ethics committee of the Second Affiliated Hospital of Xi'an Jiaotong University and registered at Clinical Trials.gov (NCT 03620994).
Inclusion criteria: (1) The presence of IBS symptoms that met the Rome IV criteria; (2) Age 18 years old or older; (3) Visited the gastroenterology clinics and completed colonoscopy; and (4) A routine blood examination, routine fecal examination, and fecal occult blood test were performed within the last 6 mo (otherwise, eligible patients were required to finish these tests).
Exclusion criteria: (1) Other diagnosed diseases that can explain patients’ IBS symptoms; (2) Metabolic diseases (uncontrolled thyroid diseases and diabetes); (3) Severe neurological and psychiatric disorders; (4) Severe and unstable extraintestinal conditions; (5) History of major abdominal surgery; (6) Pregnancy, possible pregnancy or lactation; (7) Colonoscopy was performed in the past 6 mo; (8) Currently taking large doses of anti-anxiety/anti-depressant drugs or enteric sensitive antibiotics; (9) Malignancy diagnosed to be in an active state within the last year of enrollment (excluding completely resected localized basal cell or squamous cell carcinoma of the skin); or (10) Refusal to take part in the study (see Supplementary material for details).
In this study, data were collected by designated researchers according to a specifically designed questionnaire. The main points included basic demographic characteristics, gastrointestinal symptoms, alarm symptoms, lifestyle habits, personal history, family history, medical expenses, psychological self-rating scale (self-rating anxiety scale, self-rating depression scale), laboratory results (routine fecal exam, routine blood exam and fecal occult blood test), colonoscopy findings and pathological results (if a biopsy was taken). Alarm symptoms included rectal bleeding, fecal occult blood [using the Fecal Occult Blood Test Kit (Colloidal Gold)], anemia, fever, nocturnal symptoms, unintended weight loss (in the last 3 mo), onset age > 50 years, and family history (CRC, inflammatory bowel disease (IBD) and celiac disease)[1,13-15]. With regard to organic diseases, we only included lesions that may explain IBS symptoms, and the results of colonoscopy and pathology were the gold standard. If not obstructive, colorectal polyps, melanosis coli, colonic diverticulum without inflammation, rectal varices, colic cyst, colonic leiomyoma, lipoma and neuroendocrine tumor, hemorr
Suspected IBS patients were those with IBS-like symptoms according to the Rome IV criteria, i.e., recurrent abdominal pain occurring, on average, at least 1 d a week in the last 3 mo and associated with 2 or more of the following criteria: defecation, a change in stool frequency, or a change in the form (appearance) of the stool. Criteria fulfilled for the last 3 mo with symptom onset at least 6 mo before diagnosis. In this study, patients with IBS-like symptoms and no organic diseases found by colonoscopy were defined as the IBS group.
In this study, all subjects signed an informed consent form for colonoscopy. Before undergoing colonoscopy, the patients were required to take 3000 mL of pegylated electrolyte powder in batches for bowel preparation. Colonoscopy was performed independently by experienced endoscopy operators who remained blinded to other patient information. The operators took biopsies when necessary according to endoscopic findings. When colorectal mucosa appeared normal, random biopsy was generally not performed. The pathologists also evaluated the specimens and made a pathological diagnosis without knowing other information about each patient.
In this study, quantitative variables are presented as the mean ± SD, and qualitative variables are expressed as percentages. Univariate analysis was performed using the chi-square test or Fisher's exact test when appropriate. Multivariate logistic regression analysis (forward stepwise) was used to explore the independent risk factors for organic diseases, and the results are presented as odds ratios (ORs) and 95% confidence intervals (CIs). The positive predictive value (PPV) and missed diagnosis rate were calculated to evaluate the predictive value of alarm symptoms. Statistical analyses were performed using SPSS 18.0 (SPSS Inc. Chicago, IL, United States) software. Double-tailed P<0.05 values were considered statistically significant.
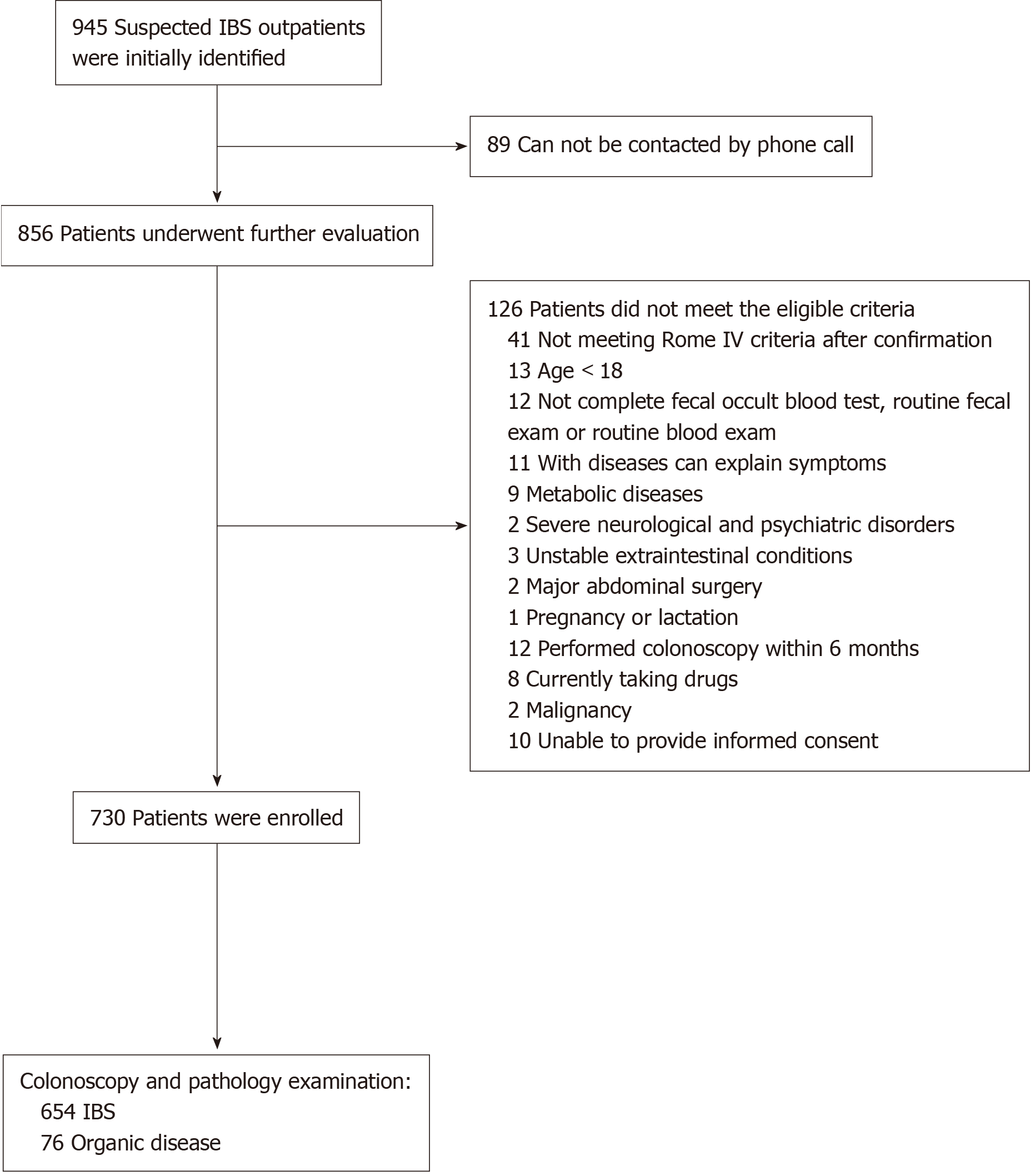
In this study, 945 patients were identified in the initial screening; of these, 89 were not successfully contacted, and 126 did not meet the eligibility criteria. Finally, a total of 730 patients were enrolled (Figure 1). With the exception of the psychological self-rating scale, which was completed by only 328 patients, all other data for the 730 patients were obtained and included in the data analysis. According to the colonoscopy and pathology results, suspected IBS patients were divided into the IBS group (n = 654) and the organic disease group (n = 76).
Univariate analysis showed that marital status (P = 0.014) was significantly different between the two groups. However, there were no significant differences in gender, body mass index, educational level, alcohol use, tobacco use, exercise time, history of gastrointestinal infection, sleep quality, dietary factors, psychological self-rating scale or medical expenses (P > 0.05) (Table 1).
| Characteristics | IBS (n = 654) | Organic disease (n = 76) | P value |
| Female | 307 (46.94) | 27 (35.53) | 0.059 |
| Onset age (yr)1 | 0.682 | ||
| > 50 | 268 (40.98) | 33 (43.42) | |
| ≤ 50 | 386 (59.02) | 43 (56.58) | |
| BMI (kg/m2) | 0.360 | ||
| < 18.5 | 37 (5.66) | 1 (1.32) | |
| 18.5-23.9 | 357 (54.59) | 45 (59.21) | |
| 24.0-27.9 | 212 (32.42) | 26 (34.21) | |
| ≥ 28 | 48 (7.34) | 4 (5.26) | |
| Marital status | 0.014 | ||
| Married | 592 (90.52) | 60 (78.95) | |
| Never married | 46 (7.03) | 11 (14.47) | |
| Divorced | 3 (0.46) | 1 (1.32) | |
| Widowed | 13 (1.99) | 4 (5.26) | |
| Educational level | 0.446 | ||
| Elementary | 88 (13.46) | 13 (17.11) | |
| Junior high school | 176 (26.91) | 14 (18.42) | |
| High school | 153 (23.39) | 19 (25.00) | |
| University or technical college | 218 (33.33) | 29 (30.86) | |
| Postgraduate | 19 (2.91) | 1 (1.32) | |
| Alcohol use | 0.394 | ||
| Almost not | 488 (74.62) | 52 (68.42) | |
| Previous | 45 (6.88) | 5 (6.58) | |
| At present | 121 (18.50) | 19 (25.00) | |
| Tobacco use | 0.102 | ||
| Almost not | 456 (69.72) | 44 (57.89) | |
| Previous | 49 (7.49) | 7 (9.21) | |
| At present | 149 (22.78) | 25 (32.89) | |
| Exercise time | 0.406 | ||
| < 0.5 h/d | 154 (23.55) | 24 (31.58) | |
| ≥ 0.5 h/d | 183 (27.98) | 21 (27.63) | |
| ≥ 1 h/d | 139 (21.25) | 12 (17.11) | |
| ≥ 2 h/d | 178 (27.22) | 19 (25.00) | |
| History of GI infection | 72 (11.01) | 6 (7.89) | 0.405 |
| Poor sleep quality | 236 (36.09) | 26 (34.21) | 0.747 |
| Dietary factor | 0.900 | ||
| Raw or cold food | 131 (20.03) | 17 (22.37) | |
| Spicy food | 258 (39.45) | 37 (48.68) | |
| Lipid food | 119 (18.20) | 18 (23.68) | |
| Milk and dairy products | 95 (14.53) | 9 (11.84) | |
| Animal protein | 32 (4.89) | 4 (5.26) | |
| FODMAP diet | 103 (15.75) | 12 (15.79) | |
| Psychological self-rating scale2 | |||
| Anxiety | 0.507 | ||
| No | 207 (71.13) | 26 (70.27) | |
| Mild | 52 (17.87) | 5 (13.51) | |
| Moderate | 27 (9.28) | 6 (16.22) | |
| Severe | 5 (1.72) | 0 (0) | |
| Depression | 0.672 | ||
| No | 184 (63.23) | 26 (70.27) | |
| Mild | 53 (18.21) | 4 (10.81) | |
| Moderate | 43 (14.78) | 5 (13.51) | |
| Severe | 11 (3.78) | 2 (5.41) | |
| Medical expenses (RMB) | 0.197 | ||
| < 500 yuan | 120 (18.35) | 17 (22.37) | |
| 500-1000 yuan | 174 (26.61) | 13 (17.11) | |
| 1000-3000 yuan | 138 (21.10) | 16 (21.05) | |
| 3000-5000 yuan | 74 (11.31) | 6 (7.89) | |
| ≥ 5000 yuan | 148 (22.63) | 24 (31.58) | |
| Rectal bleeding1 | 115 (17.58) | 20 (26.32) | 0.063 |
| Fecal occult blood1 | 75 (11.47) | 18 (23.68) | 0.003 |
| Unintended weight loss (kg)1,3 | 0.003 | ||
| Without | 507 (77.52) | 47 (61.84) | |
| < 2.5 | 68 (10.40) | 16 (21.05) | |
| 2.5-5.0 | 40 (6.12) | 7 (9.21) | |
| 5.0-7.5 | 35 (5.35) | 3 (3.95) | |
| ≥ 7.5 | 4 (0.61) | 3 (3.95) | |
| Anemia1 | 37 (5.66) | 11 (14.47) | 0.007 |
| Fever1 | 17 (2.60) | 1 (1.32) | 0.770 |
| Nocturnal symptoms1 | 164 (25.08) | 17 (22.37) | 0.605 |
| Family history of IBD, CRC or celiac disease1 | 55 (8.41) | 5 (6.58) | 0.582 |
The incidence of alarm symptoms in suspected IBS patients was as high as 75.34%. Univariate analysis indicated that fecal occult blood (P = 0.003), anemia (P = 0.007) and unintended weight loss (P = 0.003) were associated with significant differences (Table 1). All factors in Table 1, except the psychological self-rating scale (which only 328 patients completed), were included in the logistic regression analysis. The results showed that female sex [OR = 0.560 (95%CI: 0.330-0.949), P = 0.031], marital status (P = 0.030), anemia [OR = 2.825 (95%CI: 1.273-6.267), P = 0.011], fecal occult blood [OR = 1.940 (95%CI: 1.041-3.613), P = 0.037] and unintended weight loss (P = 0.009) were independently associated with organic diseases (Table 2). In addition, there was a significant difference in the prevalence of organic disease when the number of alarm symptoms varied (P = 0.013) (Table 3).
| Characteristics | OR (95%CI) | P value | Partial regression coefficient |
| Female (ref male) | 0.560 (0.330, 0.949) | 0.031 | -0.580 |
| Marital status | 0.030 | ||
| Married | — | — | — |
| Never married | 2.499 (1.199, 5.209) | 0.015 | 0.916 |
| Divorced | 1.184 (0.088,15.956) | 0.899 | 0.169 |
| Widowed | 3.260 (0.964,11.029) | 0.057 | 1.182 |
| Anemia (ref absence) | 2.825 (1.273, 6.267) | 0.011 | 1.038 |
| Fecal occult blood (ref absence) | 1.940 (1.041, 3.613) | 0.037 | 0.663 |
| Unintended weight loss (kg)2 | 0.009 | ||
| Without | — | — | — |
| < 2.5 | 2.389 (1.255, 4.548) | 0.008 | 0.871 |
| 2.5-5.0 | 1.868 (0.751, 4.642) | 0.179 | 0.625 |
| 5.0-7.5 | 0.904 (0.263, 3.110) | 0.872 | -0.101 |
| ≥ 7.5 | 8.027 (1.638,39.335) | 0.010 | 2.083 |
| Number of alarm symptoms | Number of patients (n = 730) | Patients with organic disease, n (%) | P value |
| 0 | 180 | 15 (8.33) | 0.013 |
| 1 | 250 | 21 (8.40) | |
| 2 | 180 | 20 (11.11) | |
| 3 | 91 | 12 (13.19) | |
| 4 | 19 | 2 (10.53) | |
| 5 | 7 | 3 (42.86) | |
| 6 | 3 | 2 (66.67) |
In this study, colonoscopy was used as the gold standard, and patients with a normal colonoscopy were identified as having IBS. Patients with one or more alarm symptoms were predicted to have organic disease, and those without alarm symptoms were predicted to have IBS. As shown in Table 4, the PPV for organic disease in suspected IBS patients with alarm symptoms was calculated. The PPVs of individual alarm symptoms for organic disease ranged from 5% to 30% and decreased from high to low as follows: anemia (22.92%), fecal occult blood (19.35%), unintended weight loss (16.48%), rectal bleeding (14.81%), onset age > 50 years (10.96%), nocturnal symptoms (9.39%), family history of CRC, IBD or celiac disease (8.33%) and fever (5.56%). The PPVs of anemia combined with fecal occult blood, anemia combined with unintended weight loss, and fecal occult blood combined with unintended weight loss were 69.23%, 38.89% and 30.00%, respectively. The PPV was 100% when anemia, fecal occult blood and unintended weight loss were combined. As shown in Table 5, the PPV of symptom-based criteria (Rome IV) in diagnosing IBS was calculated with and without considering alarm symptoms. The PPV of Rome IV for diagnosing IBS was 89.59% without considering alarm symptoms; the PPV and missed diagnosis rate were 91.67% and 74.77% when all alarm symptoms were combined with Rome IV and 92.09% and 34.10% when only fecal occult blood, unintended weight loss and anemia were combined with Rome IV.
| Alarm symptoms | PPV (%) |
| Onset age > 50 yr | 10.96 |
| Rectal bleeding | 14.81 |
| Fecal occult blood | 19.35 |
| Unintended weight loss1 | 16.48 |
| Anemia | 22.92 |
| Fever | 5.56 |
| Nocturnal symptoms | 9.39 |
| Family history of IBD, CRC or celiac disease | 8.33 |
| Anemia + fecal occult blood | 69.23 |
| Anemia + unintended weight loss | 38.89 |
| Fecal occult blood + unintended weight loss | 30.00 |
| Anemia + fecal occult blood + unintended weight loss | 100.00 |
| Colonoscopy findings | PPV (%) | Missed diagnosis (%) | ||
| IBS | Organic disease | |||
| Without considering alarm symptoms | 654 | 76 | 89.59 | — |
| All alarm symptoms considered | ||||
| Absence (predicted IBS) | 165 | 15 | 91.67 | 74.77 |
| Presence (predicted organic disease) | 489 | 61 | ||
| Certain alarm symptoms considered1 | ||||
| Absence (predicted IBS) | 431 | 37 | 92.09 | 34.10 |
| Presence (predicted organic disease) | 223 | 39 | ||
The prevalence of organic disease was 10.41% in suspected IBS patients. The most common lesion was non-IBD and noninfectious colitis (a significant colonoscopic finding indicative of inflammation, differentiated from IBD and infectious colitis[16]) (n = 42, 5.75%), followed by terminal ileitis (n = 18, 2.47%), CRC (n = 11, 1.51%), and ulcerative colitis (n = 8, 1.10%) (Table 6). We also randomly collected colonoscopy findings of 725 healthy examiners who went to the physical examination centers in the same period. The prevalence of terminal ileitis, CRC, ulcerative colitis and total organic disease were higher in suspected IBS patients than in healthy examiners (P < 0.05) (Supplementary Table 1).
| Colonoscopy findings | Number | Percentage (%) |
| Ulcerative colitis | 8 | 1.10 |
| Non-IBD and noninfectious colitis | 42 | 5.75 |
| CRC | 11 | 1.51 |
| Terminal ileitis | 18 | 2.47 |
| Total organic diseases | 76 | 10.41 |
Alarm symptoms are common in IBS patients, but not all alarm symptoms have good predictive value for organic disease[13]. Hammer et al[6] suggested that onset age > 50 years and blood stains on toilet paper had good predictive value for organic disease. In China, one study[17] showed that onset age > 40 years, hemafecia, melena and anemia helped distinguish organic disease from functional disease, while another study[18] found that hematochezia, emaciation and anemia helped distinguish the two. However, both of these studies focused on patients with lower gastrointestinal symptoms rather than suspected IBS patients. Based on the Rome IV criteria, we found that fecal occult blood, unintended weight loss and anemia had high predictive value for organic disease. Hemorrhoids were not regarded as organic disease, considering that their prevalence rate is as high as 50.28% in Chinese adults[19], which could affect the judgment of the value of rectal bleeding. In addition, the proportion of patients with organic disease increased as the number of alarm symptoms increased, consistent with previous studies[15].
Some studies[6,11,12] have shown that symptom-based criteria combined with alarm symptoms have high predictive value for diagnosing IBS. Vanner et al[11] found that the PPVs in prospective and retrospective studies were 98% and 100%, respectively. Whitehead et al[12] showed that the PPV was 47.9% without considering alarm symptoms and increased to 52.1% when considering alarm symptoms, with a missed diagnosis rate of 84%, and the PPV of individual alarm symptoms for identifying organic disease was 7%-9%. In this study, the PPV of Rome IV for diagnosing IBS was 89.59% when ignoring alarm symptoms and increased to 91.67% when all alarm symptoms were considered, with a missed diagnosis rate of 74.77%. When only fecal occult blood, unintended weight loss and anemia were considered, the PPV was 92.09%, but the missed diagnosis rate decreased to 34.10%. Furthermore, anemia, fecal occult blood and unintended weight loss alone had a higher PPV for organic disease, and the PPV for organic disease was 100% when anemia, fecal occult blood and unintended weight loss were combined.
These results indicate that for suspected IBS patients, considering alarm symptoms does not significantly improve PPV for diagnosing IBS. However, alarm symptoms can help identify patients with organic disease; in particular, fecal occult blood, unintended weight loss and anemia have a high value in predicting organic disease. The presence of those factors suggests that further examination may be needed, but they are not recommended as exclusion criteria for diagnosing IBS, consistent with the findings of Whitehead et al[12], for several reasons. First, the prevalence of organic disease is relatively low, making the PPV of Rome IV criteria for diagnosing IBS high. As the incidence of alarm symptoms is high, the PPV is not significantly improved when considering all alarm symptoms, and the missed diagnosis rate is high. When only fecal occult blood, unintended weight loss and anemia are considered, the PPV remains high and almost unchanged, while the missed diagnosis rate decreases significantly. Second, a missed diagnosis of organic disease, such as IBD or CRC, has serious consequences[1]. However, a comprehensive diagnostic examination of all suspected IBS patients to exclude organic disease would place a huge burden on patients and society, especially given the expensive and invasive nature of colono
Some results of this study differ from those presented in previous studies. Reasons for these discrepancies include the following: (1) Hammer et al[6] evaluated all presenting patients and performed a full diagnostic workup for patients; Vanner et al[11] included only patients without alarm symptoms; Whitehead et al[12] conducted systematic chart reviews of patients with clinical diagnoses of IBS. In the above studies, the physician’s final diagnosis was the gold standard; (2) The diagnostic criteria for IBS and definitions of alarm symptoms vary among studies. We used the Rome IV criteria, while other studies used the Manning criteria and Rome I or Rome II criteria; and (3) The prevalence of organic disease, which could affect the assessment of predictive value, was 10.41% in this study, compared with 10.3% and 30.3% in previous studies[21,22]. Currently, there is no standard definition of organic disease that distinguishes it from IBS. The organic diseases in this study included ulcerative colitis, CRC, terminal ileitis, non-IBD and noninfectious colitis, which could explain IBS symptoms.
It has been suggested that not all symptoms should be attributed to IBS, which would delay colonoscopy[16,22]. Studies have also shown that a negative colonoscopy does not provide protection for IBS patients[23]. In this study, the prevalence of terminal ileitis, CRC and ulcerative colitis was significantly higher in suspected IBS patients than in healthy examiners. Although the prevalence of organic diseases is low, they incur a great deal of harm. Thus, a necessary colonoscopy should not be delayed in suspected IBS patients. The Chinese consensus recommends colonoscopy for patients aged over 40 years[9]. However, our results suggest that the predictive value of onset age is poor in suspected IBS patients. It is necessary to conduct more research based on IBS patients.
We also found that male sex (reference female) and never-married status were risk factors for organic disease. Studies have shown that females are more likely to have IBS[2]. The relationship between marital status and FBD may be related to differences in lifestyle and stress according to marital status[24].
One of the major advantages of this study is its large sample size. A total of 730 subjects were enrolled. Patients were evaluated independently by the receiving doctors. Colonoscopy and pathology were performed independently by operators without knowledge of other patient information, ensuring that the results were more consistent with the clinical reality. This is also the first study to explore the predictive value of alarm symptoms in suspected IBS patients based on the Rome IV criteria.
There were some limitations in this study. First, older patients are more likely to undergo colonoscopy, which may lead to a high incidence of alarm symptoms. However, the incidence of alarm symptoms in previous studies is similar to that in our study (70%-84%)[12,13,15]. Second, this study was mainly conducted in the form of questionnaires, which may have caused information bias. Third, due to the normal appearance of microscopic colitis under colonoscopy and because tests related to celiac disease, lactose malabsorption and bacterial overgrowth were not widely evaluated, we could not exclude the above diseases. However, the prevalence of these diseases is low in China. Finally, this study was conducted in 3 tertiary centers and limited to a northwest Chinese population. The findings deserve further validation in primary care units in gastrointestinal clinics and in national multicenters.
In conclusion, based on the Rome IV criteria, anemia, fecal occult blood and unin
The diagnosis of irritable bowel syndrome (IBS) depends on symptoms, while the accuracy of symptom-based criteria is poor. Alarm symptoms have long been applied in the diagnosis of IBS. However, no study has explored the predictive value of alarm symptoms in suspected IBS patients based on the latest Rome IV criteria.
The symptoms of IBS overlap with those of many organic diseases, and IBS lacks specific diagnostic tests and biomarkers. There are differences in previous research results on the predictive value of alarm symptoms in IBS, and there is no relevant study based on Rome IV. Evaluating the value of alarm symptoms provides guidance for clinical evaluation of the risk of organic diseases in suspected IBS patients, giving necessary auxiliary examination and correct diagnosis of IBS.
The objective was to investigate the predictive value of alarm symptoms in suspected IBS patients based on Rome IV. Furthermore, an IBS prediction model was established to guide the clinical and scientific work of IBS.
This cross-sectional study was conducted at three academic urban tertiary care centers to ensure the sample size, sample representativeness and reliability of the results. Eligible patients completed questionnaires (paper version or electronic version), underwent laboratory tests, and were assigned to the IBS or organic disease group according to colonoscopy findings and pathology results. Investigators did not give any intervention to the patients and inspectors, and the results were more in line with clinical practice.
Anemia, fecal occult blood, unintended weight loss, female sex and marital status were independently correlated with organic disease. The positive predictive value (PPV) of alarm symptoms for organic disease was highest for anemia, fecal occult blood and unintended weight loss, and it was 100% when these three factors were combined. The PPV and missed diagnosis rate for diagnosing IBS were 91.67% and 74.77% when all alarm symptoms were combined with Rome IV and 92.09% and 34.10% when only fecal occult blood, unintended weight loss and anemia were combined with Rome IV, respectively.
Alarm symptoms, especially fecal occult blood, unintended weight loss and anemia, have a high predictive value for organic disease in suspected IBS patients based on Rome IV. The presence of those alarm symptoms suggests that further examination may be needed, but they are not recommended as exclusion criteria for diagnosing IBS.
By collecting large-scale, high-quality and national multicenter data, a simple, practical and efficient IBS diagnosis model can be further constructed. Of course, we should continue to deepen the research on the etiology and mechanism of IBS, actively look for specific biomarkers and/or diagnostic tests and achieve a more accurate diagnosis of IBS.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Caballero-Mateos AM, Gravina AG S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel Disorders. Gastroenterology. 2016;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1781] [Cited by in F6Publishing: 1554] [Article Influence: 194.3] [Reference Citation Analysis (2)] |
| 2. | Palsson OS, Whitehead W, Törnblom H, Sperber AD, Simren M. Prevalence of Rome IV Functional Bowel Disorders Among Adults in the United States, Canada, and the United Kingdom. Gastroenterology. 2020;158:1262-1273.e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 171] [Cited by in F6Publishing: 214] [Article Influence: 53.5] [Reference Citation Analysis (0)] |
| 3. | Gwee KA, Ghoshal UC, Chen M. Irritable bowel syndrome in Asia: Pathogenesis, natural history, epidemiology, and management. J Gastroenterol Hepatol. 2018;33:99-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther. 2014;40:1023-1034. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 280] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 5. | Tack J, Stanghellini V, Mearin F, Yiannakou Y, Layer P, Coffin B, Simren M, Mackinnon J, Wiseman G, Marciniak A; IBIS-C Study group. Economic burden of moderate to severe irritable bowel syndrome with constipation in six European countries. BMC Gastroenterol. 2019;19:69. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 6. | Hammer J, Eslick GD, Howell SC, Altiparmak E, Talley NJ. Diagnostic yield of alarm features in irritable bowel syndrome and functional dyspepsia. Gut. 2004;53:666-672. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Chey WD, Nojkov B, Rubenstein JH, Dobhan RR, Greenson JK, Cash BD. The yield of colonoscopy in patients with non-constipated irritable bowel syndrome: results from a prospective, controlled US trial. Am J Gastroenterol. 2010;105:859-865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 125] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 8. | Ford AC, Lacy BE, Talley NJ. Irritable Bowel Syndrome. N Engl J Med. 2017;376:2566-2578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 344] [Cited by in F6Publishing: 357] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 9. | Study Group of Functional Gastrointestinal Disorders; Study Group of Gastrointestinal Motility; Chinese Society of Gastroenterology; Chinese Medical Association. Chinese expert consensus of irritable bowel syndrome in 2020. Zhonghua Xiaohua Zazhi. 2020;40:803-818. [DOI] [Cited in This Article: ] |
| 10. | Gwee KA, Gonlachanvit S, Ghoshal UC, Chua ASB, Miwa H, Wu J, Bak YT, Lee OY, Lu CL, Park H, Chen M, Syam AF, Abraham P, Sollano J, Chang CS, Suzuki H, Fang X, Fukudo S, Choi MG, Hou X, Hongo M. Second Asian Consensus on Irritable Bowel Syndrome. J Neurogastroenterol Motil. 2019;25:343-362. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Vanner SJ, Depew WT, Paterson WG, DaCosta LR, Groll AG, Simon JB, Djurfeldt M. Predictive value of the Rome criteria for diagnosing the irritable bowel syndrome. Am J Gastroenterol. 1999;94:2912-2917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 172] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 12. | Whitehead WE, Palsson OS, Feld AD, Levy RL, VON Korff M, Turner MJ, Drossman DA. Utility of red flag symptom exclusions in the diagnosis of irritable bowel syndrome. Aliment Pharmacol Ther. 2006;24:137-146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Black TP, Manolakis CS, Di Palma JA. "Red flag" evaluation yield in irritable bowel syndrome. J Gastrointestin Liver Dis. 2012;21:153-156. [PubMed] [Cited in This Article: ] |
| 14. | Quigley EM, Fried M, Gwee KA, Khalif I, Hungin AP, Lindberg G, Abbas Z, Fernandez LB, Bhatia SJ, Schmulson M, Olano C, LeMair A; Review Team:. World Gastroenterology Organisation Global Guidelines Irritable Bowel Syndrome: A Global Perspective Update September 2015. J Clin Gastroenterol. 2016;50:704-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Patel P, Bercik P, Morgan DG, Bolino C, Pintos-Sanchez MI, Moayyedi P, Ford AC. Prevalence of organic disease at colonoscopy in patients with symptoms compatible with irritable bowel syndrome: cross-sectional survey. Scand J Gastroenterol. 2015;50:816-823. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Gu HX, Zhang YL, Zhi FC, Jiang B, Huang Y. Organic colonic lesions in 3,332 patients with suspected irritable bowel syndrome and lacking warning signs, a retrospective case--control study. Int J Colorectal Dis. 2011;26:935-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Li XB, Liu WZ, Ge ZZ, Xiao SD. Clinical value of warning symptoms and signs in the diagnosis of gastrointestinal diseases. Chin J Gastroenterol. 2005;10:198-202. [Cited in This Article: ] |
| 18. | Zhong XF, Gan AH, Huang RX, Xu AG, Liu YH, Yu ZG. Predictive value of gastrointestinal warning symptoms in the diagnosis of intestinal diseases. Linchuang Yixue Gongcheng. 2017;24:33-34. [DOI] [Cited in This Article: ] |
| 19. | Shi Y, Yang D, Chen S, Wang S, Li H, Ying J, Zhang M, Li Y, Xing Z, Sun J. Factors influencing patient delay in individuals with haemorrhoids: A study based on theory of planned behavior and common sense model. J Adv Nurs. 2019;75:1018-1028. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Lee V, Guthrie E, Robinson A, Kennedy A, Tomenson B, Rogers A, Thompson D. Functional bowel disorders in primary care: factors associated with health-related quality of life and doctor consultation. J Psychosom Res. 2008;64:129-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Ishihara S, Yashima K, Kushiyama Y, Izumi A, Kawashima K, Fujishiro H, Kojo H, Komazawa Y, Hamamoto T, Yamamoto T, Sasaki Y, Shimizu T, Okamoto E, Yoshimura T, Furuta K, Noguchi N, Tanaka H, Murawaki Y, Kinoshita Y. Prevalence of organic colonic lesions in patients meeting Rome III criteria for diagnosis of IBS: a prospective multi-center study utilizing colonoscopy. J Gastroenterol. 2012;47:1084-1090. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Akhtar AJ, Shaheen MA, Zha J. Organic colonic lesions in patients with irritable bowel syndrome (IBS). Med Sci Monit. 2006;12:CR363-CR367. [PubMed] [Cited in This Article: ] |
| 23. | Begtrup LM, Engsbro AL, Kjeldsen J, Larsen PV, Schaffalitzky de Muckadell O, Bytzer P, Jarbøl DE. A positive diagnostic strategy is noninferior to a strategy of exclusion for patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2013;11:956-62.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Yao X, Yang YS, Cui LH, Sun G, Peng LH, Wang WF, Hyder Q, Zhang XL. The overlap of upper functional gastrointestinal disorders with irritable bowel syndrome in Chinese outpatients: A multicenter study. J Gastroenterol Hepatol. 2016;31:1584-1593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |