Published online Jan 20, 2021. doi: 10.5662/wjm.v11.i1.1
Peer-review started: December 3, 2020
First decision: December 11, 2020
Revised: December 17, 2020
Accepted: December 27, 2020
Article in press: December 27, 2020
Published online: January 20, 2021
In the ongoing coronavirus disease 2019 (COVID-19) pandemic, when children remain home-confined secondary to the closure of schools, little is known of the burden of the parents being their index case.
To determine the prevalence of parents being the index case of COVID-19 infected children.
A database search in PubMed and Scopus ensued to recruit studies reporting the index case information of COVID-19 infected individuals aged ≤ 18. The reviewed articles' quality evaluation included the use of the National Heart, Lung, and Blood Institute's tool. A random-effect meta-analysis ensued to determine the prevalence of the parent being and not-being the index case. Heterogeneity was assessed by I2 and Chi2 statistics. The publication bias was evaluated by funnel plots and Egger’s test.
Overall, this review included 13 eligible studies sourcing data from 622 children of 33 nations. Study designs were heterogeneous and primarily included descriptive reports (38.4%). The prevalence of parent being the index case was 54% (95%CI: 0.29-0.79; I2: 62.3%, Chi2 P < 0.001). In > 70% of children, their index-case parent was symptomatic due to COVID-19 at the time of infection transmitting. Studies for which a risk of bias assessment was possible were of fair quality.
There is a substantial global burden of parents being the index case of COVID-19 infected children, and frequently these parents are symptomatic. Therefore, from a public health perspective, early detection of these parents is crucial.
Core Tip: During the ongoing coronavirus disease 2019 (COVID-19) pandemic situation, while schools remain closed and children primarily stay at home, the prevalence of parent to child COVID-19 transmissibility remains unknown. Therefore, this meta-analysis chiefly quantifies this epidemiological burden. Globally, this burden was substantial (about 54%) and was highest in Asia. The majority of these parents (> 70%) were symptomatic. This study highlights the public health importance of early detection of COVID-19 infected parent index cases to decrease transmission to their wards.
- Citation: Saha S, Saha S. Epidemiological burden of parents being the index cases of COVID-19 infected children. World J Methodol 2021; 11(1): 1-14
- URL: https://www.wjgnet.com/2222-0682/full/v11/i1/1.htm
- DOI: https://dx.doi.org/10.5662/wjm.v11.i1.1
In March 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) epidemic that originated in China as a pandemic[1]. By August 2020, the toll of COVID-19 cases crossed 22 million globally[2]. Our knowledge of COVID-19 has increased at a remarkably fast pace as new research findings became available. Nevertheless, COVID-19 has been less well studied in children, as their reported number of cases, disease severity, and fatality have been less than the adults[3,4]. However, as the testing of the disease increased in different nations and because young children often fail to use face masks effectively[5], the COVID-19 cases in children are rising and it can be severe in children with comorbidities like congenital heart disease and malnutrition[6]. The inability of the children to report their symptoms or contact history is a major challenge in identifying pediatric COVID-19 infection[7]. In the ongoing pandemic scenario, while children often stay at home with parents as schools remain closed in various nations[8], the household transmission risk of the infection from their parents remain high. Moreover, contemporary research[4] has primarily focused on the possibility of children being the index case and not on the other way around when parents can be the index case. Consequently, it's imperative to investigate the vulnerability of children's infectivity from their parents.
Therefore, in this study, we primarily quantified the epidemiologic burden of parents being the index cases of COVID-19 transmission in children.
This review report adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline[9] and is registered in the PROSPERO (CRD 42020209006)[10].
Population: COVID-19 diagnosed children aged ≤ 18.
Study design: Articles reporting the index cases of the above study population was incorporated. Publications of all types including experimental and observational studies, case reports, case series, letters, descriptive reports, and editorials were eligible.
Studies were excluded if its study population included pregnant females.
The search for title and abstract of articles published in the English language took place in the PubMed and Scopus databases irrespective of the publication date and geographical boundary. The last date of the search was Sep 12, 2020. We also searched the Google search engine and the bibliography of the reviewed articles. The search terms used to search the PubMed were: “index case*” OR "index patient*" OR "patient zero" AND child* OR pediatric* OR infant OR toddler OR Adolescent and “Syndrome Coronavirus 2” OR “coronavirus” OR “COVID-19” OR “COVID 19.”
Following the uploading of the database search results to the Rayyan systematic review software[11] and successive duplicate elimination, we skimmed the remaining excerpts while matching these against the eligibility criteria. Articles likely to meet these criteria or when decision-making was not possible by reading the title and abstracts only, a full-text reading ensued. Salient features like the study design, inclusion criteria, COVID-19 diagnostic method of children and their index case, relation to the index case, the symptom and death information of the index case, and the number of COVID-19 positive children were abstracted using a pre-piloted form.
The risk of bias assessment (RoB) evaluation categorized each study as good, fair, or poor utilizing the National Heart, Lung, and Blood Institute's tool[12]. For case reports, descriptive reports (not categorizable to any study design), letters, and editorials, we did not perform RoB assessment as validated tools to appraise such articles don't exist. We independently selected studies, abstracted data, and assessed the RoB, and resolved all disagreements by discussion. For experimental studies, the RoB assessment was planned by the Cochrane tool[13]; however, it was not used as the reviewed studies did not include a clinical trial.
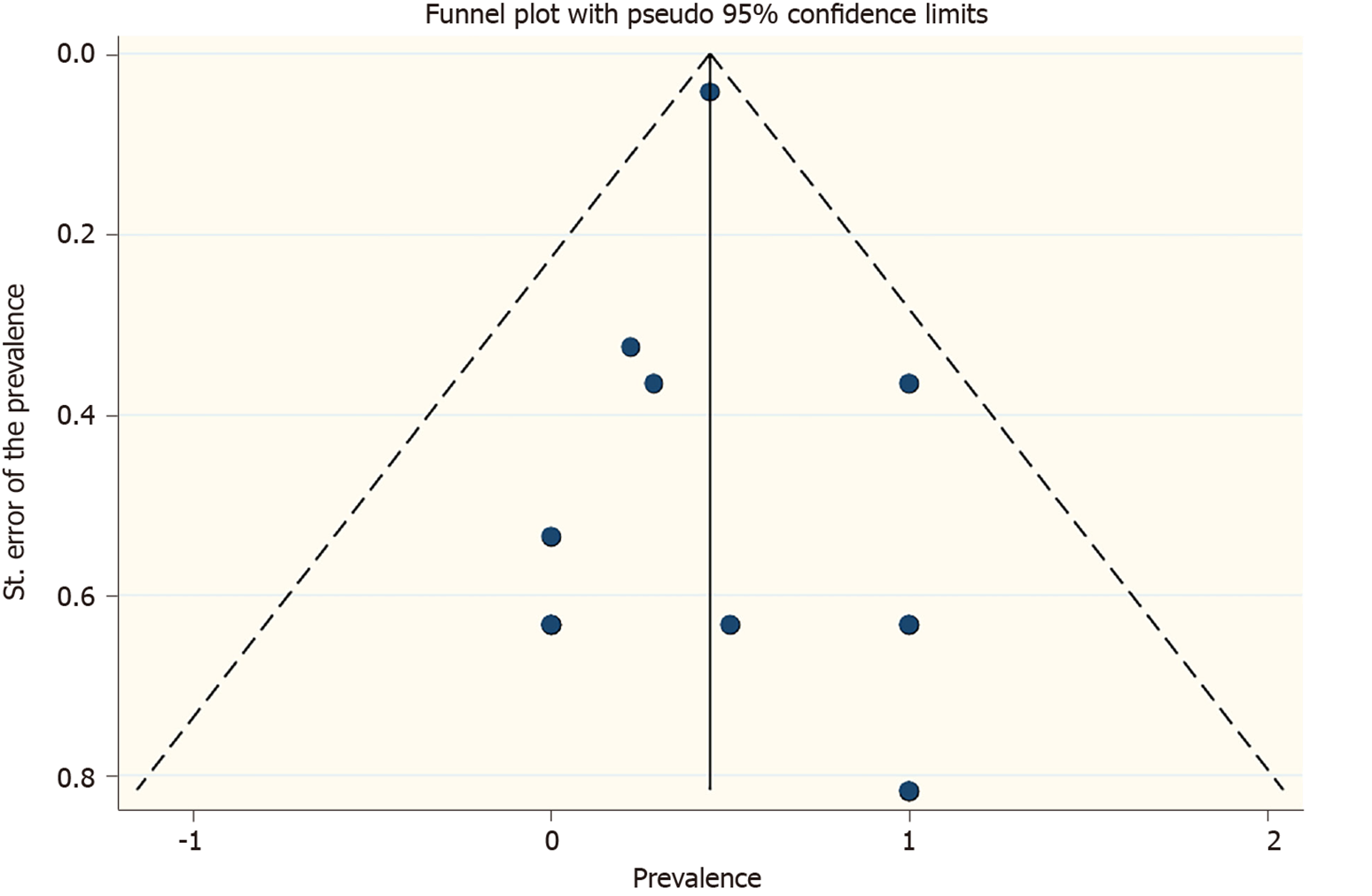
Using the random-effect (DerSimonian and Laird) meta-analysis (exact binomial method with Freeman-Tukey double arcsine transformation), we estimated the weighted overall and subgroup prevalence of parents being the index case of COVID-19 infected children. Subgrouping was done by continent, country, COVID-19 diagnostic method used in children and their index case, and the index case’s symptom status (symptomatic versus asymptomatic) and death. Heterogeneity was as-sessed by I2 (catego-rized as low, moderate, or high at values of 25%, 50%, and 75%)[14] and P value of Chi2 statistics (statistically significant at P < 0.1). Exploring the reasons for heterogeneity were not necessary as it was moderate. The publication bias judgment included the use of funnel plots and Egger’s test, and sensitivity analysis repeated the meta-analysis while dropping a study each time.
Analytic software Stata (version 16) was used to perform analysis. P < 0.05 and 95% confidence interval (CI) estimate the statistical significance.
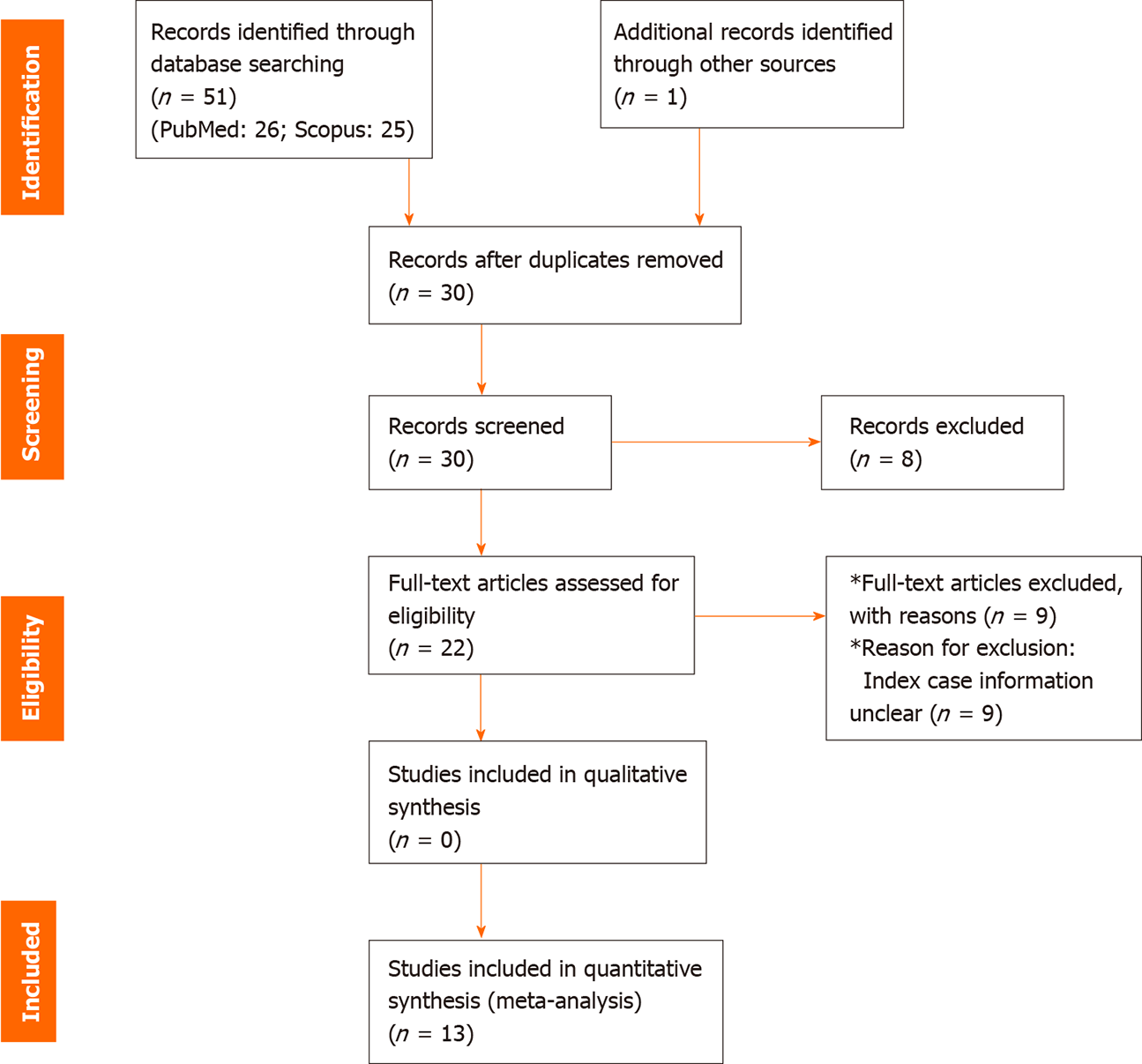
The database search retrieved 51 citations. After eliminating the duplicates, out of the 30 articles skimmed, we read 22 manuscripts in full-text and finally reviewed 13 studies[15-27] published in 2020 (Figure 1). These articles chiefly constituted of descriptive reports (38.4%) and case series (23.1%). Other article variants were cross-sectional study (15.4%), research letter (15.4%), and case report (7.7%). Cumulatively, the studies sourced data of 622 children of 33 nations from four continents (Asia, Europe, North America, and South America).
Primarily the COVID-19 infection in the children was diagnosed by reverse transcription polymerase chain reaction (RT-PCR) (99.7%). The index case was mainly an immediate family member or unknown person (96%) for children whose index case was not their parent (n = 276). Table 1 depicts the salient features of the reviewed articles.
| Ref. | Country | Continent | Study design | Study period (2020) | Inclusion criteria | COVID-19 diagnosis confirmation in children | Age of COVID-19 infected children with index case | No. of COVID-19 infected children with index case | COVID-19 infected index case/s’ | ||||
| Parent | Not-parent1 | Age | COVID-19 diagnosis Ascertainment | Symptoms around the time of contact with children | Death due to COVID-192 | ||||||||
| Götzinger et al[15], 2020 | 21 European nations except France3 | Europe | Case series | 1 Apr-24 Apr | ≤ 18 yr SARS-CoV-2 infected individuals | RT-PCR | Median age 5·yr (IQR 5–12) | 324 | 24 (sibling); 234 (immediate family member or unknown) | Unclear | History | Unclear | Unclear |
| Kim et al[16], 2020 | South Korea | Asia | Cross-sectional | 20 Jan- 6 Apr | ≤ 18 yr SARS-CoV-2 infected individuals | RT-PCR | 15 yr | 0 | 1 (sibling) | 16 yr | RT-PCR | Symptomatic | No |
| 0 | 1 [unknown (not parent or sibling)] | Unclear | Unclear | Unclear | Unclear | ||||||||
| Luo et al[20], 2020 | China | Asia | Case report | NA | NA | RT-PCR | Average 7 yr | 2 | 0 | 39 yr | RT-PCR | Symptomatic | No |
| Merza et al[21], 2020 | Iraq | Asia | Case series | 18 Mar-07 April | Hospitalized conformed COVID-19 cases | RT-PCR | Average 11 yr | 3 | 0 | 45 yr | RT-PCR | Symptomatic | No |
| Silva et al[22], 2020 | Brazil | South America | Descriptive report | NA | NA | Rapid test | Average 10.5 yr | 2 | 0 | 2 index cases: Male: 51 yr; female: 42 yr | RT-PCR | Symptomatic (both) | No |
| Song et al[23], 2020 | China | Asia | Descriptive report | NA | NA | RT-PCR | Average 3.94 yr | 5 | 0 | Parents (n = 3): Average age 40.33 yr | RT-PCR | Symptomatic | No |
| 0 | 2 (grandparent) | Grandparent (n = 1): 60 yr | Symptomatic | No | |||||||||
| Torres et al[24], 2020 | Chile | South America | Cross-sectional | NA | All school staff and randomly selected students | RT-PCR | Unclear | 0 | 7 (school staff) | Unclear | RT-PCR | Unclear | Unclear |
| Yang et al[25], 2020 | Taiwan | Asia | Descriptive report | NA | NA | RT-PCR | 11 yr | 0 | 1 (grandparent) | 85 yr | RT-PCR | Symptomatic | Yes |
| Yung et al[26], 2020 | Singapore | Asia | Case series | 5 Mar–30 Apr | Paediatric household contacts of confirmed COVID-19 cases | RT-PCR | Unclear | 74 | 2 (grandparent or another adult except parent)5 | Unclear | RT-PCR | Unclear | Unclear |
| Zhang et al[27], 2020 | China | Asia | Research letter | 28 Jan–15 Mar | Secondary COVID-19 cases | RT-PCR | Average 3 yr | 2 | 0 | Unclear | RT-PCR | One case: Mild symptoms. Other case: Moderate symptom | Unclear |
| Danis et al[17], 2020 | France | Asia | Descriptive report | NA | NA | RT-PCR | 9 yr | 0 | 1 (a visitor/tourist) | Unclear | RT-PCR | Yes | No |
| James et al[18], 2020 | United States | North America | Descriptive report | NA | NA | RT-PCR | ≤ 18 yr | 0 | 2 (a pastor and his wife) | Two index cases aged 56 and 57 yr | RT-PCR | During contact: Initially asymptomatic, then symptomatic | No |
| Jung et al[19], 2020 | South Korea | Asia | Research letter | NA | NA | RT-PCR | Average 5.5 yr | 1 | 0 | The mother: 40 yr | RT-PCR | During contact asymptomatic (symptomatic after RT-PCR diagnosis) | No |
| 0 | 1 (another patient who stayed in the same room) | For 9 years old: Unclear | Unclear | Unclear | Unclear | ||||||||
The cross-sectional and case-series studies were of fair quality (Table 2).
| Study design: Case series | |||||||||||||||||||||||
| Ref. | 1. Was the study question or objective clearly stated? | 2. Was the study population clearly and fully described, including a case definition? | 3. Were the cases consecutive? | 4. Were the subjects comparable? | 5. Was the intervention clearly described? | 6. Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants? | 7. Was the length of follow-up adequate? | 8. Were the statistical methods well-described? | 9. Were the results well-described? | Quality rating (Good, fair, or poor) | |||||||||||||
| Götzinger et al[15], 2020 | Yes | Yes | CD | Yes | NA | Yes | NA | Yes | Yes | Fair | |||||||||||||
| Merza et al[21], 2020 | Yes | Yes | CD | Yes | NA | Yes | NA | Yes | Yes | Fair | |||||||||||||
| Yung et al[26], 2020 | Yes | Yes | Yes | Yes | NA | Yes | NA | Yes | Yes | Fair | |||||||||||||
| Study design: Cross-sectional study | |||||||||||||||||||||||
| Ref. | 1. Was the research question or objective in this paper clearly stated? | 2. Was the study population clearly specified and defined? | 3. Was the participation rate of eligible persons at least 50%? | 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | 5. Was a sample size justification, power description, or variance and effect estimates provided? | 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? | 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | 10. Was the exposure(s) assessed more than once over time? | 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | 12. Were the outcome assessors blinded to the exposure status of participants? | 13. Was loss to follow-up after baseline 20% or less? | 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | Quality rating (Good, fair, or poor) | ||||||||
| Kim et al[16], 2020 | Yes | Yes | NA | Yes | No | No | No | NA | Yes | NA | CD | NA | NA | No | Fair | ||||||||
| Torres et al[24], 2020 | Yes | Yes | NA | Yes | Yes | No | No | NA | Yes | NA | CD | NA | NA | No | Fair | ||||||||
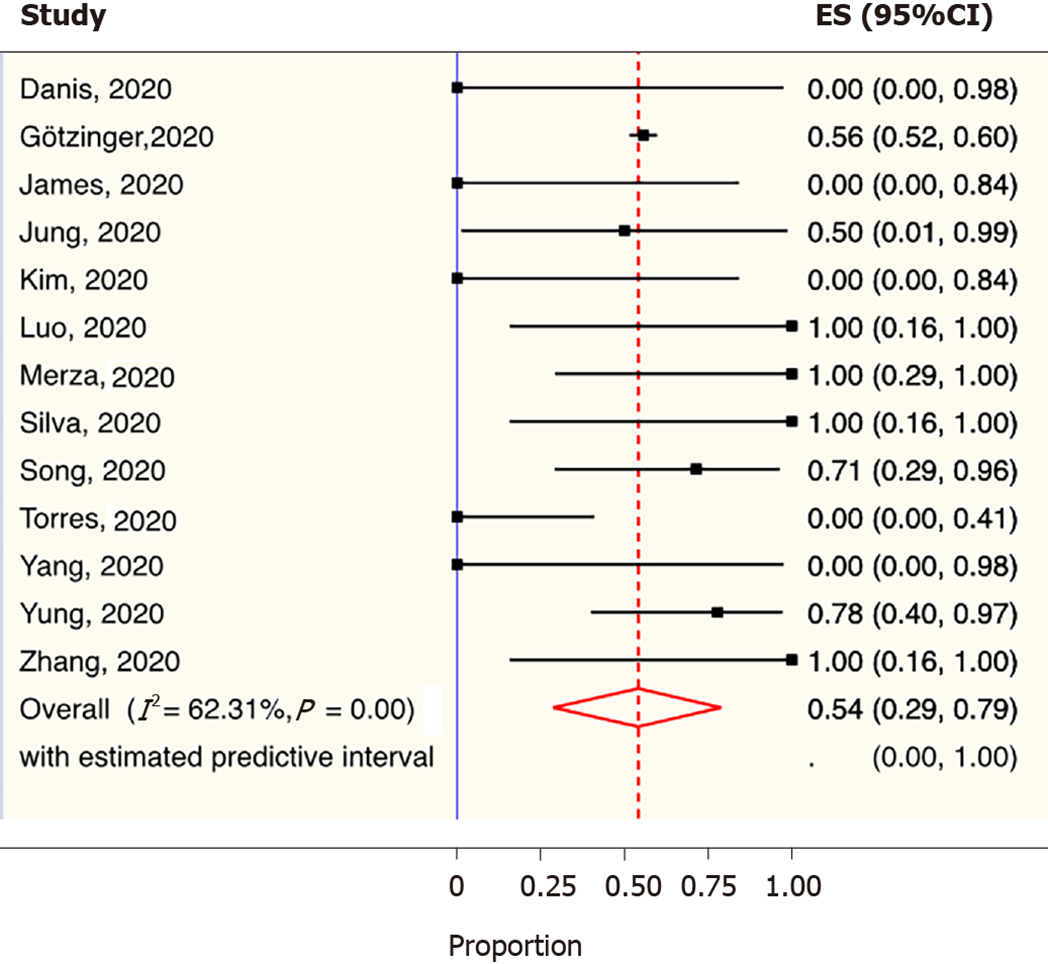
The overall weighted prevalence of parents being the index case of COVID-19 in children was 54% (95%CI: 0.29-0.79; I2: 62.3%, Chi2 P < 0.001) (Figure 2). Continent-wise this was highest in Asia (75%; 95%CI: 0.45-0.97), followed by Europe (58%; 95%CI: 0.52-0.63). The index cases’ RT-PCR-based COVID-19 diagnosis (60%; 95%CI: 0.20-0.94) was four percentage point higher than a history-based diagnosis (56%; 95%CI: 0.52-0.60). The prevalence of parent-index-case being symptomatic or not dying due to COVID-19 was about 73% each at the time of disease transmission to their children (Table 3).
| Prevalence of COVID-19 infected children with parents being the index case | |||||||||
| Subgroup | Category | Number of studies | Number of COVID-19 positive children | Number of COVID-19 positive children with parent being the index case | Weighted prevalence of COVID-19 positive children with parent being the index case | 95% prediction interval | Heterogeneity measures | ||
| % | 95%CI | I2 (%) | Q (P value) | ||||||
| Continent | Asia | 8 | 28 | 20 | 75.0 | 0.45-0.97 | 0.1-1.0 | 31.8 | 0.17 |
| Europe | 2 | 583 | 324 | 58.0 | 0.52-0.63 | Inestimable | - | - | |
| North America | 1 | 2 | 0 | 0.0 | 0.00-0.84 | Inestimable | - | - | |
| South America | 2 | 9 | 2 | 11.0 | 0.00- 0.47 | Inestimable | - | - | |
| Country | 21 European nations except France1 | 1 | 582 | 324 | 56.0 | 0.52-0.60 | Inestimable | - | - |
| France | 1 | 1 | 0 | 0.0 | 0.00-0.98 | Inestimable | - | - | |
| Brazil | 1 | 2 | 2 | 100.0 | 0.16-1.00 | Inestimable | - | - | |
| Chile | 1 | 7 | 0 | 0.0 | 0.00-0.41 | Inestimable | - | - | |
| China | 3 | 11 | 9 | 87.0 | 0.54-1.00 | Inestimable | - | - | |
| Iraq | 1 | 3 | 3 | 100.0 | 0.29-1.00 | Inestimable | - | - | |
| Singapore | 1 | 9 | 7 | 78.0 | 0.40-0.97 | Inestimable | - | - | |
| South Korea | 2 | 4 | 1 | 18.0 | 0.00-0.77 | Inestimable | - | - | |
| Taiwan | 1 | 1 | 0 | 0.0 | 0.00-0.98 | Inestimable | - | - | |
| United States | 1 | 2 | 0 | 0.0 | 0.00-0.84 | Inestimable | - | - | |
| COVID-19 diagnosis in children | RT-PCR | 12 | 620 | 344 | 50.0 | 0.24-0.76 | 0.0-1.0 | 63.4 | 0 |
| Rapid Method | 1 | 2 | 2 | 100.0 | 0.16-1.00 | Inestimable | - | - | |
| COVID-19 diagnosis in the index case | RT-PCR | 10 | 36 | 21 | 60.0 | 0.20-0.94 | 0.0-1.0 | 69.0 | 0.00 |
| History | 1 | 582 | 324 | 56.0 | 0.52-0.60 | Inestimable | - | - | |
| Unclear | 2 | 4 | 1 | 18.0 | 0.00-0.77 | Inestimable | - | - | |
| COVID-19 index patient clinical presentation | Symptomatic | 8 | 20 | 14 | 73.0 | 0.33-1.00 | 0.0-1.0 | 44.2 | 0.08 |
| Unclear | 5 | 602 | 332 | 36.0 | 0.06-0.72 | 0.0-1.0 | 77.2 | 0.00 | |
| COVID-19 index patient mortality | Died | 1 | 1 | 0 | 0.0 | 0.00-0.98 | Inestimable | - | - |
| Not died | 6 | 17 | 12 | 74.0 | 0.29-1.00 | 0.0-1.0 | 48.5 | 0.08 | |
| Unclear | 6 | 604 | 334 | 44.0 | 0.13-0.78 | 0.0-1.0 | 74.1 | 0.00 | |
| Overall | NA | 13 | 622 | 346 | 54.0 | 0.29-0.79 | 0.0-1.0 | 62.3 | 0.00 |
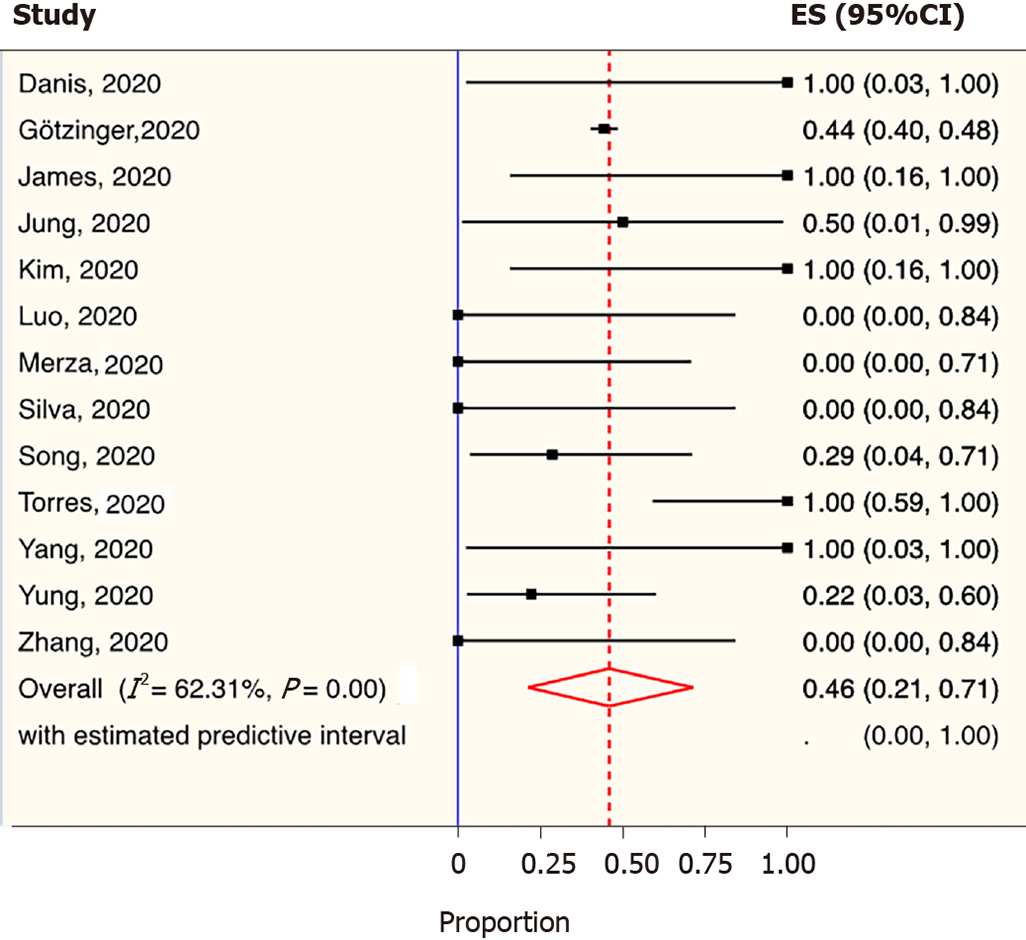
The crude prevalence of parents not being the index case was 46% (95%CI: 0.21-0.71; I2: 62.3%; Chi2 P < 0.01) (Figure 3). It was substantial in the North (100%) and South (89%) United States. Only 27.0% (95%CI: 0.00-0.67; I2: 44.3%) of these cases were symptomatic (Table 4).
| Prevalence of COVID-19 infected children with parents not being the index case | |||||||||
| Subgroup | Category | Number of studies | Number of COVID-19 positive children | Number of COVID-19 positive children with parent not being the index case | Weighted prevalence of COVID-19 positive children with parent not being the index case | 95% prediction interval | Heterogeneity measures | ||
| % | 95% CI | I2 (%) | Q (P value) | ||||||
| Continent | Asia | 8 | 28 | 8 | 25.0 | 0.03-0.55 | 0.0-0.9 | 31.8 | 0.17 |
| Europe | 2 | 583 | 259 | 42.0 | 0.37-0.48 | Inestimable | - | - | |
| North America | 1 | 2 | 2 | 100.0 | 0.16-1.00 | Inestimable | - | - | |
| South America | 2 | 9 | 7 | 89.0 | 0.53-1.00 | Inestimable | - | - | |
| Country | 21 European nations except France1 | 1 | 582 | 258 | 44.0 | 0.40-0.48 | Inestimable | - | - |
| France | 1 | 1 | 1 | 100.0 | 0.03-1.00 | Inestimable | - | - | |
| Brazil | 1 | 2 | 0 | 0.0 | 0.00-0.84 | Inestimable | - | - | |
| Chile | 1 | 7 | 7 | 100.0 | 0.59-1.00 | Inestimable | - | - | |
| China | 3 | 11 | 2 | 13.0 | 0.00-0.46 | Inestimable | - | - | |
| Iraq | 1 | 3 | 0 | 0.0 | 0.00-0.71 | Inestimable | - | - | |
| Singapore | 1 | 9 | 2 | 22.0 | 0.03-0.60 | Inestimable | - | - | |
| South Korea | 2 | 4 | 3 | 82.0 | 0.23-1.00 | Inestimable | - | - | |
| Taiwan | 1 | 1 | 1 | 100.0 | 0.03-1.00 | Inestimable | - | - | |
| United States | 1 | 2 | 2 | 100.0 | 0.16-1.00 | Inestimable | - | - | |
| COVID-19 diagnosis in children | RT-PCR | 12 | 620 | 276 | 50.0 | 0.24-0.76 | 0..0-1.0 | 63.4 | 0.00 |
| Rapid method | 1 | 2 | 0 | 0.0 | 0.00-0.84 | Inestimable | - | - | |
| COVID-19 diagnosis in the index case | RT-PCR | 10 | 36 | 15 | 40.0 | 0.06-0.80 | 0.0-1.0 | 68.9 | 0.00 |
| History | 1 | 582 | 258 | 44.0 | 0.40-0.48 | Inestimable | - | - | |
| Unclear | 2 | 4 | 3 | 82.0 | 0.23-1.00 | Inestimable | - | - | |
| COVID-19 index patient clinical presentation | Symptomatic | 8 | 20 | 6 | 27.0 | 0.00-0.67 | 0.0-1.0 | 44.3 | 0.08 |
| Unclear | 5 | 602 | 270 | 64.0 | 0.28-0.94 | 0.0-1.0 | 77.2 | 0.00 | |
| Overall | NA | 13 | 622 | 276 | 46.0 | 0.21-0.71 | 0.0-1.0 | 62.3 | 0.00 |
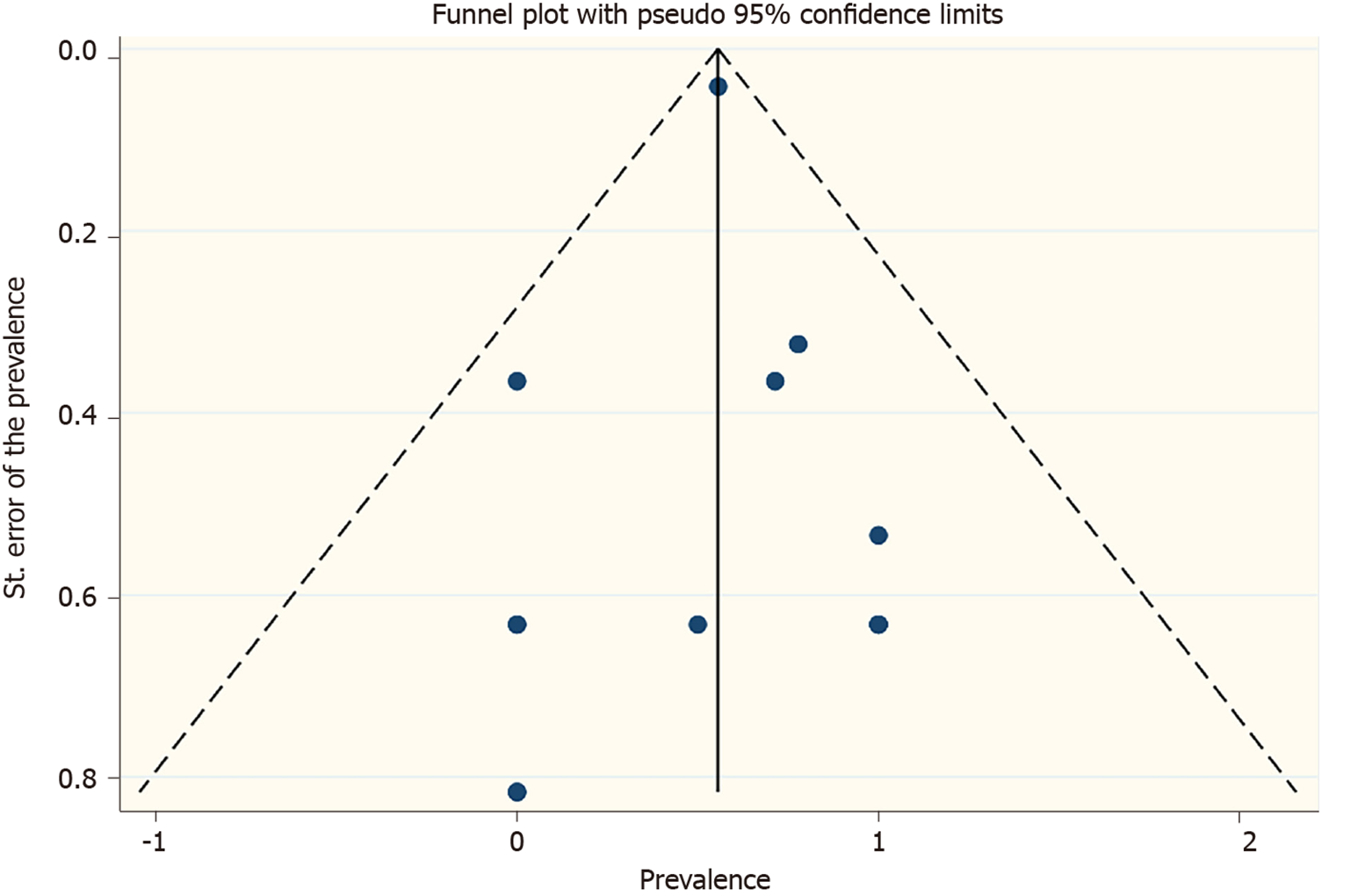
Overall, the heterogeneity was moderate. The funnel plots (Figures 4 and 5) and the Egger’s test (index case parent: P = 0.198; index case non-parent: P = 0.488) were not suggestive of any small study effect.
On dropping a study each time and repeating the meta-analysis, the prevalence estimates of the parent being the index case ranged between 49%-65%.
Altogether, we reviewed the data of 622 children from four different continents. The parents were the index cases in a substantial proportion of COVID-19 infected children and were highest in Asia. In seven out of ten COVID-19 infected children, the index parent case was symptomatic at the time of disease acquiring.
During this COVID-19 pandemic, schools remain closed in several nations, presuming that it would minimize the risk of transmission of the severe acute respiratory syndrome coronavirus 2 from children to adults[8]. Henceforth, children across the globe primarily remain at home, which increases their odds of getting COVID-19 from their parent/s since the latter are at risk of acquiring the disease from the community due to their required outdoor activities. As our findings suggest that a considerable proportion of the parents were the index cases of COVID-19 transmission to their children, their early detection and isolation is crucial to ensure early intervention. However, as we observed the highest global burden of parents being the index cases of COVID-19 in children in Asian nations, isolation of infected parents may not be unchallenging in these countries since many households lack an adequate number of rooms. Notably, the cities are more population-dense in Asia than those in the rest of the globe[28].
The chief rigor of this study is its novelty to review an unexplored area of COVID-19 literature. Besides, the evidence synthesized in this paper is likely to be comprehensive as the database search criteria did not restrict to any geographic boundary or date range. Additionally, as we did not exclude from meta-analysis the studies with zero numerators, our estimates plausibly did not compromise with the sample size and power of the analysis. However, there are a few weaknesses in our paper. Mostly the reviewed articles were not of any particular study design to allow a proper risk of bias assessment. Furthermore, distinguishing index-parents by gender or biological origin (i.e., blood relation or stepparent) was impossible due to the lack of reporting of this information in the reviewed articles. Finally, for deaths among index cases, as we made estimates depending on the period for which the articles reported their data, we could not account for COVID-19-related deaths in them that might have happened beyond this period.
At present, while we are still learning about the transmission dynamics of COVID-19 in children, this study provides a preliminary estimate of the epidemiological burden of the parents being their index case. Our findings emphasize the importance of isolating COVID-19 positive parents when they are living with their children in the same household to break the chain of transmission. Moreover, as most index case parents were symptomatic, early COVID-19 testing in adults, particularly in those residing with their wards is mandated, to ensure early diagnosis and isolation.
In COVID-19 infected children, parents are frequently the index cases than any other individual. A considerable proportion of these parents are expected to be symptomatic when they transmit the disease to their wards. In this context, early detection of COVID-19 infected parents is likely to be a chief public health initiative.
Presently little is known about the global epidemiological burden of parent-to-child coronavirus disease 2019 (COVID-19) disease transmissibility.
As children primarily remain at home with their parents due to the closure of schools across the globe (presumably to prevent community transmission of COVID-19 by children), it is crucial to know their domestic vulnerability to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection from their parents.
This study chiefly aimed to determine the pooled weighted prevalence of COVID-19 infection among children when the parent/s were their index cases.
This meta-analysis incorporated articles reporting about the index case of COVID-19 infected ≤ 18 years old children by searching electronic databases. Besides data abstraction and critical appraisal of these studies, using random-effects meta-analysis, the weighted pooled prevalence of parents being and not-being the index case of the COVID-19 infected children was estimated.
This review included 13 studies published in 2020, reporting about 622 children from Asia, Europe, North America, and South America. Appraisable studies were fair in quality. The crude prevalence of parents being and not being the index cases of COVID-19 infected children were 54% (95%CI: 0.29-0.79; I2: 62.3%, Chi2 P < 0.001) and 46% (95%CI: 0.21-0.71; I2: 62.3%; Chi2 P < 0.01), respectively. For the former, on subgrouping by continent, the greatest burden was observed in Asia (75%), and most parents were symptomatic (73%).
During the ongoing COVID-19 pandemic, a substantial proportion of the COVID-19 infected children acquired the disease from their parents, and the majority of these parents were symptomatic from SARS-CoV-2 infection.
This research depicts a substantial global burden of parents being the index cases of COVID-19 infected children. It highlights the critical importance of early detection of these index cases.
Manuscript source: Invited manuscript
Specialty type: Medical laboratory technology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Carnevale S, Konakci G, Pan SL S-Editor: Fan JR L-Editor: A P-Editor: Yuan YY
| 1. | World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. 2020 [cited 2020 Sep 20]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. [Cited in This Article: ] |
| 2. | Coronavirus Update (Live): 25, 229,932 Cases and 847,706 Deaths from COVID-19 Virus Pandemic - Worldometer [Internet]. [cited 2020 Aug 30]. Available from: https://www.worldometers.info/coronavirus/#countries. [Cited in This Article: ] |
| 3. | Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088-1095. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1297] [Cited by in F6Publishing: 1399] [Article Influence: 349.8] [Reference Citation Analysis (0)] |
| 4. | Ludvigsson JF. Children are unlikely to be the main drivers of the COVID-19 pandemic - A systematic review. Acta Paediatr. 2020;109:1525-1530. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 149] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 5. | Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang ZJ. Novel Coronavirus Infection in Hospitalized Infants Under 1 Year of Age in China. JAMA. 2020;323:1313-1314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 429] [Cited by in F6Publishing: 415] [Article Influence: 103.8] [Reference Citation Analysis (0)] |
| 6. | Jiang Y, Lu XX, Jin RM, Zheng YJ, Xu BP, Xie ZD, Liu ZS, Lin LK, Shang YX, Shu SN, Bai Y, Lu M, Lu G, Deng JY, Luo WJ, Xiong LJ, Liu M, Cui XX, Ye LP, Gao LW, Wang YY, Wang XF, Li JF, Wang TY, Jiang RM, Li XW, Zhao DC, Shao JB, Yang YH, Shen KL. Novel coronavirus infections: standard/protocol/guideline recommendations for the diagnosis, prevention and control of the 2019 novel coronavirus infection in children (the second edition). Zhongguo Shiyong Erke Linchuang Zazhi. 2020;35:143-150. [DOI] [Cited in This Article: ] |
| 7. | Lifen Y, Dai Zhenyuan DM, Yang Z, Wanqiu D, Li P, Yating L, Zhuanggui C. Suggestions for medical staff from department of pediatrics during the treatment of 2019-nCoV infection/pneumonia. J NEW Med. 2020;51:77. [DOI] [Cited in This Article: ] |
| 8. | Munro APS, Faust SN. Children are not COVID-19 super spreaders: time to go back to school. Arch Dis Child. 2020;105:618-619. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 118] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 9. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6253] [Cited by in F6Publishing: 7022] [Article Influence: 468.1] [Reference Citation Analysis (0)] |
| 10. | Saha S, Saha S. The prevalence of parents being the index case of COVID-19 infection in children and adolescents. [Internet]. PROSPERO 2020 CRD42020209006 [cited 2020 Oct 2]. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020209006. [Cited in This Article: ] |
| 11. | Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5711] [Cited by in F6Publishing: 7637] [Article Influence: 954.6] [Reference Citation Analysis (0)] |
| 12. | Study Quality Assessment Tools | National Heart, Lung, and Blood Institute (NHLBI) [Internet]. [cited 2020 Jun 14]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. [Cited in This Article: ] |
| 13. | Higgins JPT GS (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. [Internet]. Cochrane Collab.2011 [cited 2020 Aug 27]. Available from: https://training.cochrane.org/handbook/archive/v5.1/. [Cited in This Article: ] |
| 14. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39087] [Cited by in F6Publishing: 41695] [Article Influence: 1985.5] [Reference Citation Analysis (1)] |
| 15. | Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, Gabrovska N, Velizarova S, Prunk P, Osterman V, Krivec U, Lo Vecchio A, Shingadia D, Soriano-Arandes A, Melendo S, Lanari M, Pierantoni L, Wagner N, L'Huillier AG, Heininger U, Ritz N, Bandi S, Krajcar N, Roglić S, Santos M, Christiaens C, Creuven M, Buonsenso D, Welch SB, Bogyi M, Brinkmann F, Tebruegge M; ptbnet COVID-19 Study Group. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653-661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 692] [Cited by in F6Publishing: 779] [Article Influence: 194.8] [Reference Citation Analysis (0)] |
| 16. | Kim J, Choe YJ, Lee J, Park YJ, Park O, Han MS, Kim JH, Choi EH. Role of children in household transmission of COVID-19. Arch Dis Child. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 79] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 17. | Danis K, Epaulard O, Bénet T, Gaymard A, Campoy S, Botelho-Nevers E, Bouscambert-Duchamp M, Spaccaferri G, Ader F, Mailles A, Boudalaa Z, Tolsma V, Berra J, Vaux S, Forestier E, Landelle C, Fougere E, Thabuis A, Berthelot P, Veil R, Levy-Bruhl D, Chidiac C, Lina B, Coignard B, Saura C; Investigation Team. Cluster of Coronavirus Disease 2019 (COVID-19) in the French Alps, February 2020. Clin Infect Dis. 2020;71:825-832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 186] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 18. | James A, Eagle L, Phillips C, Hedges DS, Bodenhamer C, Brown R, Wheeler JG, Kirking H. High COVID-19 Attack Rate Among Attendees at Events at a Church - Arkansas, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:632-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 88] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 19. | Jung J, Hong MJ, Kim EO, Lee J, Kim MN, Kim SH. Investigation of a nosocomial outbreak of coronavirus disease 2019 in a paediatric ward in South Korea: successful control by early detection and extensive contact tracing with testing. Clin Microbiol Infect. 2020;26:1574-1575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Luo Y, Trevathan E, Qian Z, Li Y, Li J, Xiao W, Tu N, Zeng Z, Mo P, Xiong Y, Ye G. Asymptomatic SARS-CoV-2 Infection in Household Contacts of a Healthcare Provider, Wuhan, China. Emerg Infect Dis. 2020;26:1930-1933. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 21. | Merza MA, Haleem Al Mezori AA, Mohammed HM, Abdulah DM. COVID-19 outbreak in Iraqi Kurdistan: The first report characterizing epidemiological, clinical, laboratory, and radiological findings of the disease. Diabetes Metab Syndr. 2020;14:547-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 22. | Silva JHD, Oliveira EC, Hattori TY, Lemos ERS, Terças-Trettel ACP. Description of COVID-19 cluster: isolation and testing in asymptomatic individuals as strategies to prevent local dissemination in Mato Grosso state, Brazil, 2020. Epidemiol Serv Saude. 2020;29:e2020264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Song R, Han B, Song M, Wang L, Conlon CP, Dong T, Tian D, Zhang W, Chen Z, Zhang F, Shi M, Li X. Clinical and epidemiological features of COVID-19 family clusters in Beijing, China. J Infect. 2020;81:e26-e30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 24. | Torres JP, Piñera C, De La Maza V, Lagomarcino AJ, Simian D, Torres B, Urquidi C, Valenzuela MT, O'Ryan M. SARS-CoV-2 antibody prevalence in blood in a large school community subject to a Covid-19 outbreak: a cross-sectional study. Clin Infect Dis. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 61] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 25. | Yang MC, Hung PP, Wu YK, Peng MY, Chao YC, Su WL. A three-generation family cluster with COVID-19 infection: should quarantine be prolonged? Public Health. 2020;185:31-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Yung CF, Kam KQ, Chong CY, Nadua KD, Li J, Tan NWH, Ganapathy S, Lee KP, Ng KC, Chan YH, Thoon KC. Household Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 from Adults to Children. J Pediatr. 2020;225:249-251. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 27. | Zhang W, Cheng W, Luo L, Ma Y, Xu C, Qin P, Zhang Z. Secondary Transmission of Coronavirus Disease from Presymptomatic Persons, China. Emerg Infect Dis. 2020;26:1924-1926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 28. | Un-Habitat. Planning and design for sustainable urban mobility: Global report on human settlements 2013 [Internet]. 2013. Available from: http://mirror.unhabitat.org/pmss/getElectronicVersion.aspx?nr=3503&alt=1. [DOI] [Cited in This Article: ] |