Published online Jun 24, 2016. doi: 10.5500/wjt.v6.i2.331
Peer-review started: January 15, 2016
First decision: February 29, 2016
Revised: May 11, 2016
Accepted: May 31, 2016
Article in press: June 2, 2016
Published online: June 24, 2016
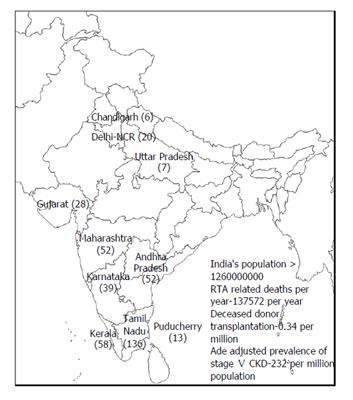
Renal replacement therapy (RRT) resources are scarce in India, with wide urban-rural and interstate disparities. The burden of end-stage renal disease is expected to increase further due to increasing prevalence of risk factors like diabetes mellitus. Renal transplantation, the best RRT modality, is increasing in popularity, due to improvements made in public education, the deceased donor transplantation (DDT) programme and the availability of free and affordable transplant services in government hospitals and certain non-governmental philanthropic organizations. There are about 120000 haemodialysis patients and 10000 chronic peritoneal dialysis patients in India, the majority of them waiting for a donor kidney. Shortage of organs, lack of transplant facilities and high cost of transplant in private facilities are major barriers for renal transplantation in India. The DDT rate in India is now 0.34 per million population, among the lowest in the world. Infrastructural development in its infancy and road traffic rules not being strictly implemented by the authorities, have led to road traffic accidents being very common in urban and rural India. Many patients are declared brain dead on arrival and can serve as potential organ donors. The DDT programme in the state of Tamil Nadu has met with considerable success and has brought down the incidence of organ trade. Government hospitals in Tamil Nadu, with a population of 72 million, provide free transplantation facilities for the underprivileged. Public private partnership has played an important role in improving organ procurement rates, with the help of trained transplant coordinators in government hospitals. The DDT programmes in the southern states of India (Tamil Nadu, Kerala, Pondicherry) are advancing rapidly with mutual sharing due to public private partnership providing vital organs to needy patients. Various health insurance programmes rolled out by the governments in the southern states are effective in alleviating financial burden for the transplantation. Post-transplant immunological and pathological surveillance of recipients remains a challenge due to the scarcity of infrastructure and other facilities.
Core tip: Deceased donor transplantation (DDT) has been increasing in India, especially in the southern states due to proactive policies of the state governments and public private partnership. With the goal of achieving maximum organ harvesting from potential organ donors and universal access to transplant services, small steps of improvement have been made. The DDT program in India has to keep progressively expanding to cater to the end-stage renal disease affected population of India.
- Citation: Abraham G, Vijayan M, Gopalakrishnan N, Shroff S, Amalorpavanathan J, Yuvaraj A, Nair S, Sundarrajan S. State of deceased donor transplantation in India: A model for developing countries around the world. World J Transplant 2016; 6(2): 331-335
- URL: https://www.wjgnet.com/2220-3230/full/v6/i2/331.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i2.331
India is the third largest economy in the world, by purchasing power parity. However, the gross domestic product (GDP) spent on healthcare is only 4%, with merely 1.3% spent by the public sector[1,2]. GDP per capita for India is United States $1630.8[3]. India faces tremendous challenges in providing basic healthcare facilities for its population, as the major percentage of the population lives below the poverty line. There has been a shift in disease epidemiology in India, with non-communicable diseases on the rise. Chronic kidney disease (CKD) is of increasing prevalence in India. CKD which is asymptomatic in early stages, puts greater financial burden on the stakeholders at the later stages. There are urban-rural and interstate disparities in the provision of renal replacement therapy (RRT), due to lack of skilled nephrologists, transplant surgeons and poor government support[4]. The CKD registry of India found that diabetic nephropathy was the commonest cause (31%) of CKD[5]. About 43% of the CKD patients had a monthly family income of < rupees 5000 (United States $78.26) and RRT has an enormous financial impact on these patients. The majority of end-stage renal disease (ESRD) patients die within months of diagnosis as RRT is unaffordable to them. With risk factors like diabetes, hypertension and obesity showing an increasing trend, the financial strain of supporting RRT services is going to be enormous. Healthcare in India is provided by the public and private sector. In the southern states such as Tamil Nadu, Kerala, Puducherry, Karnataka, Andhra Pradesh, government sponsored health insurance schemes have ensured that tertiary care hospitals provide maintenance haemodialysis, transplantation and follow-up either at very subsidized rate or free of cost and hence they cater to the lower socio economic sections of the society. RRT in private sector is unaffordable to the great majority of ESRD patients in India.
Renal transplantation is the best choice of RRT. India is a pluralistic country in terms of religion and no religion opposes saving a fellow human’s life through organ donation. The first successful live renal transplant in India was done at Christian Medical College, Vellore in 1971. The Transplantation of Human Organs Act of 1994 was an initial step in promoting legal organ transplantation in India. Over the past 4 decades, the transplantation rate has shown a steady increase, though still much lower than in developed countries.
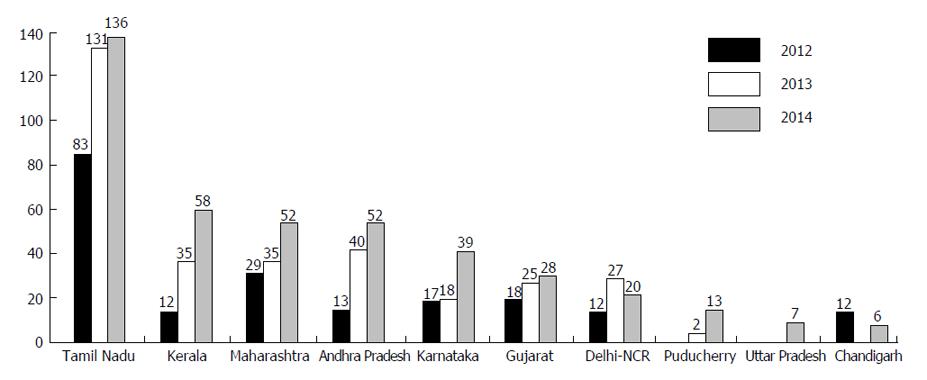
Deceased donor transplantation (DDT) is increasing in India, due to steps taken in both public and private sector, especially in the southern states. Healthcare spending is increasing partly because of revenue generation[6]. Currently the deceased donor transplantation rate is 0.34 per million which was previously 0.08 per million population in 2013[7]. As shown in Figure 1 and Table 1, a total of 1150 organs from 411 donors have been done harvested in India in 2014, comprising of 720 kidneys, 354 livers, 54 hearts, 16 lungs, 5 pancreas and 1 intestine, out of which 417 organs were harvested in Tamil Nadu. Figure 2 shows that the DDT program has steadily increased in 3 years. The generic immunosuppressive medications and induction molecules being manufactured in India have served as cost cutting measures to support multi-organ transplantation. In the government setup, transplantation services are offered at a free or subsidized cost. The cost of DDT could vary enormously in the private sector depending upon whether they are non-profit organizations or run for a profit. The DDT program in Tamil Nadu has brought down the incidence of organ trade[8].
| State | Population | No. of donors | Organ donation rate |
| Tamil Nadu | 72138958 | 136 | 1.9 |
| Kerala | 33387677 | 58 | 1.7 |
| Maharashtra | 112372972 | 52 | 0.5 |
| Andhra Pradesh | 84665533 | 52 | 0.6 |
| Karnataka | 61130704 | 39 | 0.6 |
| Gujarat | 60383626 | 28 | 0.5 |
| Delhi-NCR | 16753235 | 20 | 1.2 |
| Puducherry | 1244464 | 13 | 10.4 |
| Uttar Pradesh | 199581477 | 7 | 0.04 |
| Chandigarh | 1054686 | 6 | 5.7 |
The main barrier to DDT in India is a shortage of harvested organ pool. In India, each year an estimated 137572 people die in road traffic accidents, and about 70% of them are declared brain dead, from whom organs can be harvested[9]. Tamil Nadu state, with a population of 72 million, has developed a model approach to this problem which is being emulated by other states. Rounds of consultation have been held between the involved stakeholders and government officials to tackle the challenges of ensuring a transparent and efficient transplant program which provides practical guidelines for organ harvesting and transplantation. Government orders issued in this regard have greatly benefitted the DDT program in Tamil Nadu. There is a central coordinator for transplantation in the state of Tamil Nadu who is in charge of the donor list for deceased donor transplantation. This list has potential recipients from both public and private hospitals. As per the waiting list, organs are distributed whether it is private or public hospitals.
Public private partnership has been utilized to improve organ harvesting rates from potential organ donors. A total of 2028 transplantations from 677 donors have been done in Tamil Nadu between October 2008 and June 2015, comprising 1201 kidney transplants, 621 liver transplants, 135 heart transplants, 67 lung transplants and 4 pancreas transplants[10]. In addition to the above, 1006 corneal transplants, 616 heart valves, 17 skin donations, 2 small bowel and 1 blood vessels transplant were done in this period. Female donors constituted only 1/5th of the donor pool. Donors comprised from 21 to 50 years of age.
In India, government hospitals provide healthcare free of cost or at a subsidized cost for the underprivileged sections of the society. In Government General Hospital (GGH), Chennai, renal transplantation has been regularly performed since 1987. Pre transplant dialysis, work-up of recipient and donor and transplant surgery are provided free of cost. Life-long post-transplant immunosuppression and follow up is provided free. Initially, only living related donor transplantation was done. Though the first deceased donor renal transplantation was done in 1996,the program picked up momentum only in 2008 when the Government of Tamil Nadu gave an impetus and made it one of its “flagship” programs. So far, 172 deceased donor renal transplantations have been done at GGH.
Successful deceased donor transplant program at GGH has achieved the following. Access to renal transplantation has improved. Economic and social barriers of transplantation have been broken. The problem of shortage of organs has been taken care of, at least to a small extent. Procurement and supply of less expensive generic immuno-suppressive by the government curtails expenditure significantly. Continuous training of nephrologists, urologists, nursing staff and technicians in renal transplantation is creating a trained work force. This program has shown the benefits of “public - private” partnership. Grief counselors at Madras Medical college are provided by Multi Organ Harvesting and Networking (MOHAN) foundation. MOHAN foundation (http://www.mohanfoundation.org/) is a philanthropic non-governmental organization that aims to promote organ donation and transplantation. According to Indian law, a transplant coordinator must be present at every hospital where organ transplantation is being done. The role of the transplant coordinator is to grieve with the family and motivate the family members to get involved in the DDT program, thereby saving lives. MOHAN Foundation, through their educators, has trained 813 transplant coordinators. The MOHAN Foundation signed a memorandum of understanding with the Government General Hospital, Chennai, in 2010 to place its transplant coordinators there. Their presence has made a tremendous difference to the deceased organ donation program in the hospital. When a trained transplant coordinator counsels and spends time with grieving family, conversion figure in getting “yes for donation” is 65% in most hospitals.
In 2013, there were 137572 road traffic accidents in India. If we convert 50% of this figure into a prospective organ donor pool, we will have more than 65000 donors supplying vital organs including 130000 kidneys yearly to be transplanted for the majority of prevalent end stage renal disease patients who require renal transplantation. The authors have also used poisoned organ donors from snake envenomation leading to brain death which also forms a donor pool of tens of thousands of organ donors in the country. With economic growth and increase in transplant centers to 166 in 2013, more centers undertake organ transplantation since last 2 years in India. It is believed that there are 120000 prevalent patients on maintenance haemodialysis and 10000 prevalent patients on chronic peritoneal dialysis in India, majority of them waiting for a deceased organ donation.
There are number of drawbacks in the DDT scenario in India. Ensuring optimal and prolonged function of the graft in the recipients is a great challenge. A complement dependent cytotoxicicity cross matched technique is the predominant test to detect the compatibility between the donor and recipient. Human leukocyte antigen (HLA) matching is not done in DDT as the large majority of the patients waiting for the organ are not typed to look for HLA mismatch. Advanced immunological facilities for screening and matching are available only in the private sector and those available in a few flagship government hospitals charge a fee for the tests. Flow cytometry and luminex based platforms for testing for HLA based antibodies are not utilized in DDT, because of the lack of facilities. Hence immunological risk is not assessed regularly in recipients waiting for transplants and the long term outcome is unknown as there is a lack of dependable registries to capture the data of graft and patient survival. What we need is to find out the immunological risk to stratify the waiting patients into high, intermediate and low immunological categories. In order to augment the results of the transplantation, we require the following immunological platforms: Cell based assays, flow cytometry based assays, solid phase assays-enzyme linked immunosorbent assay, flowcytometry and microparticle based assays.
Scarcity of nephropathological services in many parts of the country in evaluating graft dysfunction on a speedy basis is another limiting factor of the DDT program. There is a lack of knowledge of prior sensitization in the recipient as panel reactive antibodies are not evaluated in the great majority of recipients. Therapeutic drug monitoring of calcineurin inhibitors and mTOR inhibitors are fraught with inaccurate results due to lack of standardization. The prospective transplant programs should take this into consideration as a next step in promoting trouble free survival of the graft by allocation according to sensitization, avoiding HLA mismatches, careful monitoring and follow up with skilled transplant team. This can only be accomplished with robust support from the respective state governments who should set up a central 24 × 7 laboratory facility which can be cost beneficial to the stakeholders in the long run.
The DDT program in India is steadily increasing due to positive steps taken by some state governments. However, organ harvestation rates from potential donors can be further increased. Emphasis must be placed on road safety, less frequent road traffic accidents and higher organ harvestation rates from potential donors. Public awareness on this is on the increasing trend. Public private partnerships have had a positive impact on the DDT program. We foresee in the next 2 decades, India will emerge as the largest deceased donor transplantation in the world. This model of public private partnership in one of the largest developing economies can be emulated by other developing countries in South Asia and African continent.
P- Reviewer: Chkhotua A, Cantarovich F, Sureshkumar KK S- Editor: Kong JX L- Editor: A E- Editor: Liu SQ
| 1. | Healthcare expenditure, public (% of GDP). World Bank data. [Accessed 2015 Aug 3]. Available from: http://data.worldbank.org/indicator/SH.XPD.PUBL.ZS. [Cited in This Article: ] |
| 2. | Healthcare expenditure, total (% of GDP). World Bank data. [Accessed 2015 Aug 3]. Available from: http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS. [Cited in This Article: ] |
| 3. | GDP per capita (current international $). World Bank data. [Accessed 2015 Aug 3]. Available from: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD. [Cited in This Article: ] |
| 4. | Abraham G, Varghese S, Thandavan T, Iyengar A, Mathew M, Naqvi SAJ, Sheriff R, Ur-Rashid H, Gopalakrishnan N, Gupta KL. CKD in South Asia. NDT Newsletter. 2015; Available from: http://www.era-edta.org/newsletter_ndt_southasia_update.html. [Cited in This Article: ] |
| 5. | Rajapurkar MM, John GT, Kirpalani AL, Abraham G, Agarwal SK, Almeida AF, Gang S, Gupta A, Modi G, Pahari D. What do we know about chronic kidney disease in India: first report of the Indian CKD registry. BMC Nephrol. 2012;13:10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 208] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 6. | Liquor sales through TASMAC in Tamil Nadu to touch Rs 29672 crore in 2015-16. 2015;. [Cited in This Article: ] |
| 7. | Saroj Super Speciality Hospital launches CORD and Multi Organ Transplant Centre in association with MOHAN Foundation. MOHAN Foundation, 2015. Available from: http://www.mohanfoundation.org/activities/Saroj-Super-Speciality-Hospital-launches-CORD-and-Multi-Organ-Transplant-Centre-in-association-with-MOHAN-Foundation-3941.htm. [Cited in This Article: ] |
| 8. | Abraham G, Reddy YN, Amalorpavanathan J, Daniel D, Roy-Chaudhury P, Shroff S, Reddy Y. How deceased donor transplantation is impacting a decline in commercial transplantation-the Tamil Nadu experience. Transplantation. 2012;93:757-760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Transplant authority of Tamil Nadu. Cadaver Transplant Programme, Government of Tamil Nadu : Tamil Nadu Network for Organ Sharing. [Accessed 2015 Aug 3]. Available from: http://www.dmrhs.org/tnos/. [Cited in This Article: ] |