Copyright
©The Author(s) 2016.
World J Transplant. Dec 24, 2016; 6(4): 719-728
Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.719
Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.719
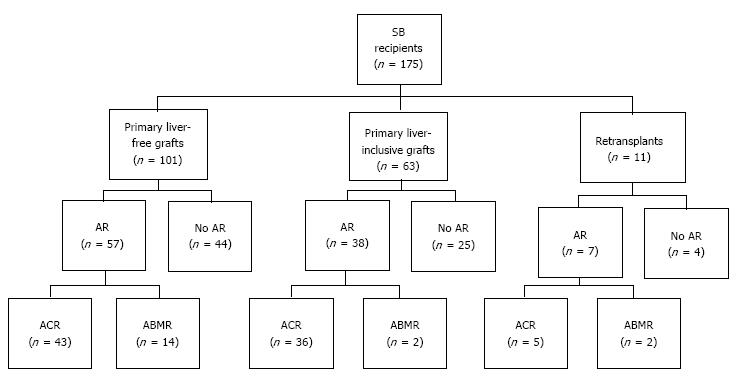
Figure 1 Patient distribution according to graft type and acute rejection type.
SB: Small bowel; AR: Acute rejection; ACR: Acute cellular rejection; ABMR: Acute antibody-mediated rejection.
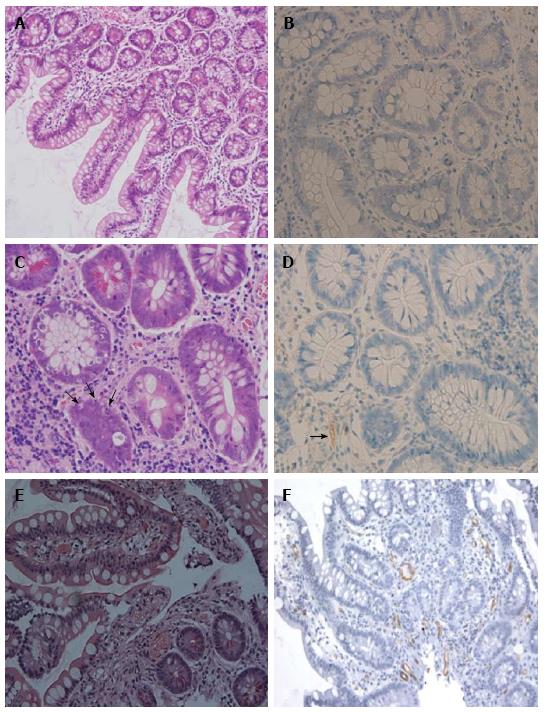
Figure 2 Histopatholgy of intestinal allograft.
A and B: No rejection: normal mucosal architecture of small bowel biopsy after transplantation. No staining for C4d is seen in the capillaries of the lamina propria; C and D: Acute cellular rejection (ACR): There is mononuclear infiltration, crypt epithelial injury, and apoptotic bodies (arrows) in the lamina propria. Weak and focal staining for C4d (arrows) is sometimes present in a patient with ACR; E and F: Acute antibody-mediated rejection (ABMR): There is prominent hemorrhage and congestion with scattered fibrin thrombin in the lamina propria. Widespread and bright staining for C4d is present in the capillaries of the lamina propria. Magnifications: × 200 in A, E and F; × 400 in B, C and D. A, C, E: H and E; B, D, F: C4d.
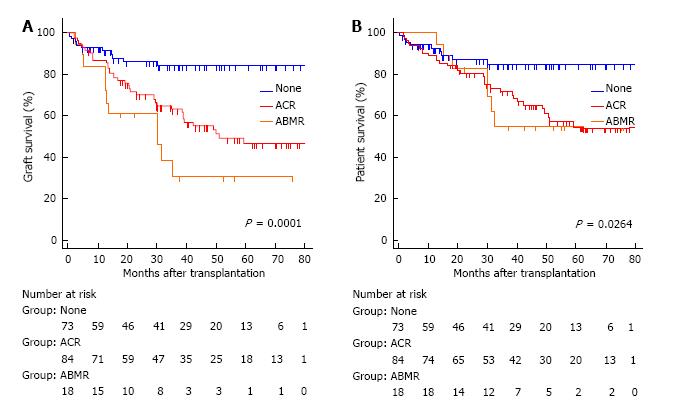
Figure 3 The Kaplan-Meier graft (A) and patient (B) survival for no acute rejection (none) (solid line), acute cellular rejection (dotted heavy line), and acute antibody-mediated rejection (dotted light line).
The overall comparison was significantly different in graft (log-rank P = 0.0001) and patient survival (log-rank P = 0.0264). The patients with antibody-mediated rejection (ABMR) or acute cellular rejection (ACR) had significantly lower graft and patient survival than those without rejection. The graft survival was worse in ABMR than in ACR but the differences between them did not reach statistical significance (P = 0.088).
- Citation: Wu GS, Cruz Jr RJ, Cai JC. Acute antibody-mediated rejection after intestinal transplantation. World J Transplant 2016; 6(4): 719-728
- URL: https://www.wjgnet.com/2220-3230/full/v6/i4/719.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i4.719