Published online Jun 22, 2013. doi: 10.5498/wjp.v3.i2.34
Revised: May 13, 2013
Accepted: May 16, 2013
Published online: June 22, 2013
AIM: To investigate the treatment priority given to self-harmers presenting to a hospital emergency department (ED) in Queensland, Australia, over the period 2005-2010.
METHODS: The main outcome measure of this study was the treatment priority given to persons presenting with suicide ideation and communication (SIC) or self-harming behaviour. Treatment priority was measured using the Australasian Triage Scale, which ranks patients from 1 (in need of immediate treatment) to 5 (assessment and treatment to start within 120 min). Ordered logistic regression was used to assess the broad demographic and treatment-related factors associated with more urgent triage categories and to investigate which methods of non-fatal suicidal behaviour (NFSB) were prioritised as most urgent.
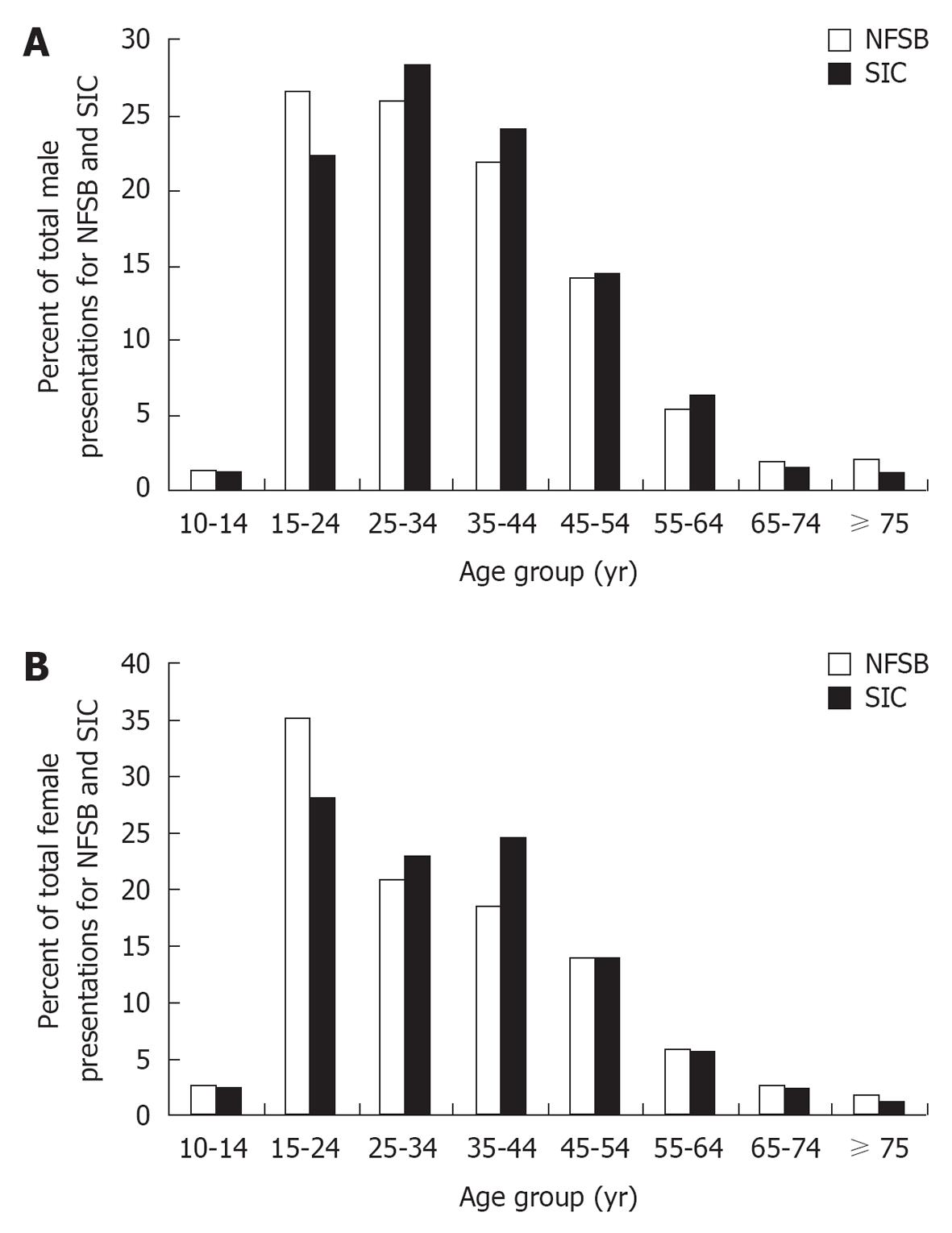
RESULTS: Most cases of NFSB were between 15 and 34 years. A larger proportion of persons presenting for SIC were aged 35 to 44 years. Over 50% of male presentations and 38% of female presentations were for SIC. Those cases prioritised as being more urgent had significantly greater odds of being older, presented after an act of self-harm rather than SIC, and had used multiple methods of NFSB. These individuals also had greater odds of being male and having made past presentations for SIC or NFSB. Among males, those presenting after ingestion of drugs had the greatest odds of receiving immediate attention compared to SIC. “Cutters” were considered as the least “urgent” subjects, and had a greatest risk of waiting 60 to 120 min for treatment compared to suicide ideators. Among females, those presenting with chemicals, poisons and gases had the greatest odds of receiving immediate attention compared to SIC. Females who presenting after cutting themselves had lower odds of receiving immediate treatment than those who presented with SIC.
CONCLUSION: ED staff seems to judge the urgency of cases based on demographic factors such as age and gender, as well as method of NFSB.
Core tip: Emergency department (ED) staff judge the urgency of cases based on demographic factors such as age and gender, as well as method of non-fatal suicidal behaviour. Those who overdose on drugs are often prioritised for treatment sooner than those who presented after self-cutting or suicide ideation. These results highlight the need for specialised interventions for persons presenting to an ED for suicidality.
- Citation: Milner A, Kõlves K, Kõlves K, Gladman B, De Leo D. Treatment priority for suicide ideation and behaviours at an Australian emergency department. World J Psychiatr 2013; 3(2): 34-40
- URL: https://www.wjgnet.com/2220-3206/full/v3/i2/34.htm
- DOI: https://dx.doi.org/10.5498/wjp.v3.i2.34
A large number of persons who have died or attempted suicide sought help from hospital emergency departments (EDs)[1-4]. Many of these persons have attended an ED more than once, often for various reasons including repeated self-harm, mental disorders, substance abuse, unintentional injuries, assault, headache pain, and other complaints[5]. Thus, hospital EDs could play an important role in identifying those at acute risk of suicide.
Despite the frequency of attendance, few countries in the world have established reporting systems for recording non-fatal behaviours in EDs[6]. The lack of regular surveillance of non-fatal suicidal behaviours (NFSB) means that there is limited opportunity to gain insights into important topics such the length of time before suicidal persons receive treatment in EDs. Recognising the importance of this issue, several international studies endorsed by the World Health Organization (WHO)[7,8] have implemented the use of standardised and consistent recording practices. These studies advocate for consistent nomenclatures and standardised reporting methods in hospital EDs. Following past recommendations of WHO collaborating studies, we used the term “NFSB” to refer to all cases where “the individual, expecting to, or taking the risk to die or to inflict bodily harm, initiated and carried out with the purpose of bringing about wanted changes”[9]. This approach is in line with the current version of the International Classification of Disease (10th revision), which codes all self-injurious and harmful behaviours under the category “intentional self-harm” (X60-X84)[10].
The present paper describes a retrospective study based on the monitoring component of the latest WHO study on suicide; the suicide trends in at-risk territories (START) study in Australia[11]. This particular branch of the large international effort entails the implementation of a recording system for suicidal behaviours [either suicide ideation and communication (SIC) or NFSB] in an ED of one Queensland hospital.
The first aim of the study was to assess the demographic characteristics and reason for presentation (either SIC or NFSB) for persons based on triage category. This provided information on possible variation in the demographic and treatment-related factors associated with receiving different broad triage scores. Secondly, we aimed to study the differences in treatment priority based on the specific method of suicidal behaviour. There have been past publications on the negative attitudes of hospital staff towards persons who present with suicide methods such as “cutting”[12-15], but limited investigation into the treatment priority given to suicide attempters. This research therefore constitutes a new topic of investigation in suicide research.
The Emergency Department Information System (EDIS) of the Gold Coast Hospital, Queensland, Australia, constituted the primary source of information. EDIS is an electronic database completed by administrative staff and treating doctors and nurses. Administrative staff record information including: unit record number (individually assigned number), name, age, gender and date/time of presentation. Nurses and doctors assign triage score (explained below), reason for presentation, date/time of arrival and departure, and location of discharge. Nurses and doctors also provide a text description (narrative) of the reason for presentation and final diagnosis.
The nature of the EDIS database makes it impossible to conduct a reliable analysis of suicide ideation, especially for what concerns intent to die. Because of this, we took a broad approach to classification based on earlier work by Silverman and colleagues[16]. This classification aims to capture information on all suicide-related ideations and communications, inclusive of both threats and plans. Suicide ideation may be transient, passive, active or persistent and is inclusive of thoughts with no suicide intent, undetermined intent, and (at least some degree of) suicide intent.
Records of presentations for SIC or NFSB were obtained through a daily key word search of EDIS utilising a wide array of terms, such as self-harm, suicide, attempt, attempted suicide, parasuicide, and self-injury. We also searched for possible cases using descriptions of methods included under the International Classification of Diseases (ICD)-10 codes for intentional self-harm (X60-X84) such as laceration, cutting, overdosing, ingesting, gassing, hanging, poisoning, jumping, and drowning, etc. All cases were independently checked and coded by two researchers, who closely examined both the clinical notes made under the categories “presenting problem” and “final diagnosis upon departure from the ED”. Cases presenting with an overdose of alcohol and/or illicit drugs were not considered as NFSB, unless SIC was stated.
The ICD-10 codes were used to classify up to three methods. The first method mentioned in the case was considered as the primary method. For the purpose of this paper, ICD codes were aggregated into the following broad categories: poisoning by analgesics (X60), poisoning by antidepressants and sedatives (X61), poisoning by other drugs (X62-X64), poisoning by chemicals, other poisons, gases (X66-X69), other methods (all those methods with a low frequency in the EDIS system) (X70-X77, X79-X84), and cutting with a sharp object (X78). As explained above, cases of SIC were defined using the guidelines provided by Silverman and colleagues (2007).
The Human Research Ethics Committee of Griffith University and the Gold Coast Health Service District granted ethical clearance for the study.
We used the triage scores on the Australasian Triage Scale (implemented in Australian hospitals since 2001) to gain understanding of treatment prioritisation. Triage is predominantly a nursing assessment that begins when the patient presents to the ED and is used to rank patient from 1 to 5 in terms of treatment priority[17,18]. The five-tiered system used in the ATS is: (1) immediate (cases judged to be immediately life-threatening); (2) assessment and treatment to occur within 10 min; (3) assessment and treatment to start within 30 min; (4) assessment and treatment to start within 60 min; and (5) assessment and treatment to start within 120 min.
The analyses presented in the paper are specific to “events” (number of presentations) rather than “persons”. Ordered logistic regression was applied to assess the broad demographic and treatment-related factors associated with more urgent triage categories. This technique of data analysis was chosen as the outcome variable was the categorical and ordinal five-tiered ATS scale, which was re-ordered so that “5” represented immediate treatment and “1” represented a wait of between 60 and 120 min. Independent variables included sex, age (10 to 24 years, 25 to 44 years, 45 to 64 years, and 65 years and older), reason for presentation (SIC vs NFSB), number of past presentations to the ED for NFSB or SIC (multiple vs none), and how many methods were associated with the presentation of NFSB (one vs multiple methods).
Following this, we sought to investigate which methods of NFSB were received the most urgent triage category. Aggregate methods of NFSB was the primary independent variable of interest; SIC was used as the reference category based on the rationale that it was qualified differently from all other presentations, which involved a behavioural act of intentional harm or injury. Analysis was stratified for males and females and controlled for age, number of methods (one vs multiple methods), and number of past presentations to the ED for NFSB or SIC (multiple vs none).
Figure 1 displays presentations (events) for both NFSB and SIC by sex. Over the time period 2005-2010, 2229 males attended the ED for NFSB and 2349 attended for SIC. There were 3602 female presentations for NFSB and 2231 for SIC. Most presentations were by those aged between 15 and 44 years. However, a χ2 test showed that a significantly greater proportion of males presented with SIC rather than NFSB between the ages of 15-24 years [χ2(1) = 10.8, P < 0.001]. The majority of female presentations between 15-24 years were for NFSB rather than SIC [χ2(1) = 29.6, P < 0.001] and there was a greater proportion of presentations for SIC than NFSB among females aged 35-44 years [χ2(1) = 31.3, P < 0.001].
The ordered logistic regression shown in Table 1 demonstrates factors associated with receiving more urgent triage categories. After controlling for factors related to the presentation (i.e., reason for presentation, number of past presentations, number of methods of NFSB used), those prioritised as more urgent had significantly greater odds of being male (OR: 1.12, 95%CI: 1.04-1.22, P = 0.004) and being of over the age of 25 years. For example, persons over 65 years had over 2.37 times the odds of being prioritised as more urgent than those aged under 24 years (OR: 2.37, 95%CI: 1.90-2.96, P < 0.001). Further, those who were prioritised as more urgent had nearly four times the odds of presenting after NFSB, rather than SIC (OR: 3.93, 95%CI: 3.57-4.34, P < 0.001). These cases also had greater odds of having received past treatment (OR: 1.15, 95%CI: 1.05-1.27, P = 0.003) and having used multiple methods of NFSB (OR: 1.63, 95%CI: 1.46-1.82, P < 0.001).
| Variables | OR | 95%CI | P value |
| Sex (ref. = female ) | 1.12 | 1.04-1.22 | 0.004 |
| Age (yr) | |||
| 10-24 | 1.00 | ||
| 25-44 | 1.39 | 1.27-1.52 | < 0.001 |
| 45-64 | 1.75 | 1.56-1.96 | < 0.001 |
| ≥ 65 | 2.37 | 1.90-2.96 | < 0.001 |
| Attempt (ref. = SIC) | 3.93 | 3.57-4.34 | < 0.001 |
| Present (ref. = 1 only) | 1.15 | 1.05-1.27 | 0.003 |
| Multiple method (ref. = 1 only) | 1.63 | 1.46-1.82 | < 0.001 |
Table 2 shows the relationship between treatment priority and aggregated method of NFSB for males and females. Over 50% of presentations by males (Table 2) were for SIC, while close to 20% of presentations were for overdosing on antidepressants or sedatives, and 11% were for self-cutting. Results of the ordered logistic regression indicated that, compared to SIC, males presenting with ingestion of “other drugs” (ICD codes X62-X64) (OR: 23.21, 95%CI: 17.46-30.86, P < 0.001) had the highest odds of receiving the “most urgent” treatment priority. This was followed by ingestion of chemicals, poisons and gases (OR: 17.77, 95%CI: 11.55-27.35, P < 0.001), antidepressant and sedative overdose (OR: 9.99, 95%CI: 8.12-12.28, P < 0.001), analgesics (OR: 8.90, 95%CI: 6.54-12.11, P < 0.001), and “other methods” (OR: 3.17, 95%CI: 2.34-4.28, P < 0.001). There was a smaller significant differences in the odds of receiving a higher treatment priority for males who presented after cutting and those who presented for SIC (OR: 1.44, 95%CI: 1.16-1.77, P = 0.001).
| Variables | Male (n = 4578) | OR | 95%CI | P value | Female(n = 5833) | OR | 95%CI | P value |
| SIC | 51.31 | 1.00 | 38.25 | 1.00 | ||||
| Analgesic | 5.83 | 8.90 | 6.54-12.11 | < 0.001 | 10.34 | 7.75 | 6.16-9.76 | < 0.001 |
| Antidepressant/sedatives | 18.89 | 9.99 | 8.12-12.28 | < 0.001 | 26.85 | 8.28 | 6.94-9.89 | < 0.001 |
| Other drugs | 5.79 | 23.21 | 17.46-30.86 | < 0.001 | 5.88 | 17.10 | 13.22-22.12 | < 0.001 |
| Chemicals, poisons, gases | 1.90 | 17.77 | 11.55-27.35 | < 0.001 | 0.98 | 10.16 | 5.84-17.67 | < 0.001 |
| Other methods | 5.48 | 3.17 | 2.34-4.28 | < 0.001 | 4.80 | 2.10 | 1.58-2.80 | < 0.001 |
| Cutting | 10.79 | 1.44 | 1.16-1.77 | 0.001 | 12.91 | 0.83 | 0.70-0.99 | 0.034 |
As can be seen in Table 2, approximately 38% of female presentations were for SIC. This was followed by overdose on antidepressants (26.9%), cutting (12.9%), and overdose on analgesics (10.3%). Similar to males, female presentations for ingestion of chemicals, poisons, and gases (OR: 10.16, 95%CI: 5.84-17.67, P < 0.001), ingestion of other drugs (OR: 17.10, 95%CI: 13.22-22.12, P < 0.001), antidepressants and sedatives (OR: 8.28, 95%CI: 6.94-9.89, P < 0.001), or analgesics (OR: 7.75, 95%CI: 6.16-9.76, P < 0.001) were prioritised as more urgent than SIC. Females who attended an ED after “other” methods (OR: 2.1, 95%CI: 1.58-2.80, P < 0.001) had significantly greater odds receiving an urgent triage score, but the significance of this result was less than that for men. Females who presented after cutting (nearly 13% of the sample) had lower odds of receiving treatment sooner than those who presented with SIC (OR: 0.83, 95%CI: 0.70-0.99, P = 0.034).
Those prioritised as most in need of urgent treatment more often have engaged in NFSB than presented with SIC. A likely explanation for this result is that staff at EDs seek to first address injuries that cause pain and potentially lead to other health complications. This also may reflect attitudes among hospital staff that the pain brought about by physical harm is more important than mental or emotional pain[9,18]. This view is in direct contrast to the views expressed by suicidal persons, who often report mental pain as being significantly more distressing than physical pain[13]. While persons who present with SIC are recognised to be at risk of suicidal behaviours, their needs are generally under-rated in hospitals[19].
The results of this study also indicate that males and older persons were given higher treatment priority than females or younger persons. While recent literature on this topic suggests that the effect of age and gender is “unclear”[13], earlier research (published in the 1980s and 1990s) indicates that staff of EDs perceives females[20] and younger persons[21] as at lower risk of completing suicide. Gender and age influences on triage decisions have also been reported for physical problems, such as myocardial infarction[22], which suggests that the lower priority given to females and younger persons may be a general issue in EDs, rather than being a problem specific to suicide.
A gender-based explanation of these finding might suggest that female instances of suicidal behaviours in EDs could be seen as “attention seeking”, “manipulative behaviour” or a “cry for help”, and as such less worthy of treatment than presentations made by males[12,23]. Differences in method of NFSB could also be of relevance, with men using more lethal means [such as lying in front of a moving vehicle, jumping from a height, and hanging (“classified as other”)] in greater need of medical attention than women. Older persons more often overdosed on drugs classified as X61 by ICD-10, which also received a higher treatment priority than other methods of self-harm. However, in general, cases of drug overdose were seen relatively quickly. This could be connected to difficulties in assessing the potential lethality of ingested drugs based on the patient’s own recollections of type(s) and quantity of substance ingested.
Those who engaged in self-cutting may have had to wait between 60 and 120 min for treatment. Results for females indicated that self-cutters had to wait longer for treatment than those who presented with SIC. There is evidence that hospital staff generally have negative attitudes and greater stigma towards those who present after engaging in self-cutting, particularly for repeaters[12-15,20]. These attitudes may be also associated with a lack of training and perceived competence in the management of self-cutters[24,25].
Aside from those considered in this study, there are a number of other factors influencing triage decisions that could be explored in further research. These include a nurse’s level of clinical experience, existing information and knowledge about the patient, “intuition”, time pressures and interruptions, and lack of formal training[26]. These problems may become more complex in presentations requiring consideration of both the mental and physical state of the patient, as well as future risk of suicide. It is also worth noting that immediate treatment priority may be given to those persons displaying more disruptive and/or aggressive behaviours in the ED. These maladaptive behaviours are common in persons engaging in self-harming behaviour, and are particularly apparent during times of extreme emotional distress[27]. Environmental and design factors of the ED may also determine treatment priority. For example, the perception of disruption may be greater in an ED that is smaller and less well-equipped to deal with emotionally charged patients than a larger ED, where it is possible to separate these patients from others.
In this study, the use of triage scores allowed us to examine the management of persons presented to an ED for SIC or NFSB. However, it is important to note that these scores are relatively “crude” and are unable to confirm when treatment was actually provided. More importantly, triage scores tell us nothing about treatment quality; a person prioritised for immediate attention may be treated badly and, in some cases, it may be preferable to wait a longer time if this results in better treatment. Similarly, the data from EDIS provides no information on the severity of the injuries. Presumably, some proportion of those presenting after medically-serious self-laceration were seen immediately, while those with relatively less serious acts may have waited for a longer time.
Further, the approach we used to identify cases was reliant on the data obtained from the EDIS reporting system, which included an evaluation of both preliminary ICD-10 codes and “text field” sections. This approach is likely to have missed a number of cases that were coded or described ambiguously (particularly cases of overdose on alcohol or illicit drugs where there was no presence of suicide intent). In addition, the reporting system can only provide information on people who attended the ED, rather than those who were immediately transferred to other departments. The sample used in this study was obtained from one hospital; despite its rather large size (750 beds), we are unsure about the generalisability of results to other Hospitals.
This study made no attempt to separate cases of “non-suicidal self-injury”[28] from attempted suicide. Instead, we chose to follow the conventions of past WHO collaborating studies by including both groups in the definition of “NFSB”[9]. We chose this approach because it is relatively free of cultural bias in classification of suicide intent and is therefore comparable across different locations of the START study. Aside from this, the definition seeks to provide a practical, internationally standardised and easily understandable approach to suicide epidemiology[9]. We also acknowledge issues in the data related to SIC, which undoubtedly failed to capture all relevant cases.
In conclusion, the establishment of a system to record cases of NFSB in an Australian ED is an important step in developing evidence-based suicide intervention and prevention. This study presented a database specifically developed for this purpose and found substantial differences in the treatment priority and management given to persons seeking help for NFSB, communication and ideation. This is not the first research to shed light on this topic, as several investigators have highlighted issues in the management of persons with mental health concerns in the ED[18,29,30]. However, none of previous studies specifically focused on presentations of suicidality. While we agree with past recommendations that the overall management of NFSB in EDs needs to be improved[18,29,30], our research suggests that particular attention is needed for females, younger persons and those presenting with SIC or after engaging in self-cutting. This may indicate the need for investment into alternative treatments to reduce the burden of these presentations on the ED; for example, the development of collaborative relationships between providers such as general practitioners, hospital psychiatric teams, psychiatrists, psychologists and outpatient services would undoubtedly obtain positive outcomes.
In developed countries, a large number of persons attend hospital emergency departments (EDs) following suicidal behaviours. Many of these persons have attended an ED more than once, often for various reasons including further self-harm, mental disorders, substance abuse, unintentional injuries, assault, headache, and other complaints. Thus, the treatment provided in hospital EDs could play an important role in suicide prevention. Despite this, there is a lack of research on the priority suicidal persons are given by ED staff.
There have been numerous studies documenting the frequency at which suicidal people attend EDs. There are been a smaller number of qualitative studies on staff attitudes towards patients who have attempted suicide. There has been a lack of quantitative information on treatment priority given to suicidal persons in hospitals. Information on treatment priority is necessary in order to understand the timeliness of treatment, and how urgent ED staff perceive suicidal behaviours to be in hospital settings.
ED staff judge the urgency of cases based on demographic factors such as age and gender, as well as method of “non-fatal suicidal behaviours”. Those who overdose on drugs are often prioritised for treatment sooner than those who presented after self-cutting or suicide ideation.
The findings of this study can be used to develop training procedures for the treatment of suicidal persons in EDs. Their results also highlight the need for investment into alternative treatments to reduce the burden of suicidal presentations on EDs. These could include the development of collaborative relationships between providers such as general practitioners, hospital psychiatric teams, psychiatrists, psychologists and outpatient services.
This study uses a surveillance database to evaluate determinants of triage decisions in the ED of a Queensland hospital. The data reported are part of a larger international initiative having the objective of improving clinical care. As with many studies that utilize existing databases, the study design provides access to a large number of patient records, but the level of detail in the data collection is not great. The paper is clearly written and is easy to read. The idea is to compare triage decisions (entered on a 5-point scale) across difference clinical and demographic subgroups in order to identify differences. As the goal is to differentiate between various potentially confounded determinants of more rapid triage, multivariable regression methods are employed.
P- Reviewers Brazil IA, Patten SB, Wong KC S- Editor Gou SX L- Editor A E- Editor Zheng XM
| 1. | Kudo K, Otsuka K, Endo J, Yoshida T, Isono H, Yambe T, Nakamura H, Kawamura S, Koeda A, Yagi J. Study of the outcome of suicide attempts: characteristics of hospitalization in a psychiatric ward group, critical care center group, and non-hospitalized group. BMC Psychiatry. 2010;10:4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo CA. National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997-2001. Ann Emerg Med. 2005;46:369-375. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 174] [Cited by in F6Publishing: 185] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Dennis M, Beach M, Evans PA, Winston A, Friedman T. An examination of the accident and emergency management of deliberate self harm. J Accid Emerg Med. 1997;14:311-315. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Da Cruz D, Pearson A, Saini P, Miles C, While D, Swinson N, Williams A, Shaw J, Appleby L, Kapur N. Emergency department contact prior to suicide in mental health patients. Emerg Med J. 2011;28:467-471. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Colman I, Dryden DM, Thompson AH, Chahal AM, Borden K, Rowe BH, Voaklander DC. Utilization of the emergency department after self-inflicted injury. Acad Emerg Med. 2004;11:136-142. [PubMed] [Cited in This Article: ] |
| 6. | Mehlum L, Mork E. After the suicide attempt: The need for continuity and quality of care. International Handbook of Suicide Prevention: Research, Policy and Practice. West Sussex: Wiley-Blackwell 2011; 353-367. [Cited in This Article: ] |
| 7. | Schmidtke A, Bille-Brahe U, DeLeo D, Kerkhof A, Bjerke T, Crepet P, Haring C, Hawton K, Lönnqvist J, Michel K. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989-1992. Results of the WHO/EURO Multicentre Study on Parasuicide. Acta Psychiatr Scand. 1996;93:327-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 475] [Cited by in F6Publishing: 430] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 8. | Bertolote JM, Fleischmann A, De Leo D, Bolhari J, Botega N, De Silva D, Tran Thi Thanh H, Phillips M, Schlebusch L, Värnik A. Suicide attempts, plans, and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med. 2005;35:1457-1465. [PubMed] [Cited in This Article: ] |
| 9. | De Leo D, Burgis S, Bertolote JM, Kerkhof AJ, Bille-Brahe U. Definitions of suicidal behavior: lessons learned from the WHo/EURO multicentre Study. Crisis. 2006;27:4-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 151] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | World Health Organization. International Classification of Diseases (ICD) - version 10. Retrived August 30, 2011. Available from: http://apps.who.int/classifications/icd10/browse/2010/en. [Cited in This Article: ] |
| 11. | De Leo D, Milner A. The WHO/START Study: Promoting suicide prevention for a diverse range of cultural contexts. Suicide Life Threat Behav. 2010;40:99-106. [PubMed] [Cited in This Article: ] |
| 12. | Shaw SN. Shifting Conversations on Girls’ and Women’s Self-Injury: An Analysis of the Clinical Literature in Historical Context. Feminism & Psychology. 2002;12:191-219. [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | Hawton K, Taylor TL, Saunders KEA, Mahadevan S. Clinical care of deliberate self-harm patients: an evidence-based approach. International Handbook of Suicide Prevention: Research, Policy and Practice. West Sussex: Wiley-Blackwell 2011; 329-351. [DOI] [Cited in This Article: ] |
| 14. | Haq SU, Subramanyam D, Agius M. Assessment of self harm in an accident and emergency service - the development of a proforma to assess suicide intent and mental state in those presenting to the emergency department with self harm. Psychiatr Danub. 2010;22 Suppl 1:S26-S32. [PubMed] [Cited in This Article: ] |
| 15. | Hadfield J, Brown D, Pembroke L, Hayward M. Analysis of accident and emergency doctors’ responses to treating people who self-harm. Qual Health Res. 2009;19:755-765. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Silverman MM, Berman AL, Sanddal ND, O’carroll PW, Joiner TE. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: Suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37:264-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 595] [Cited by in F6Publishing: 603] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 17. | Considine J, Ung L, Thomas S. Clinical decisions using the National Triage Scale: how important is postgraduate education. Accid Emerg Nurs. 2001;9:101-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Broadbent M, Creaton A, Moxham L, Dwyer T. Review of triage reform: the case for national consensus on a single triage scale for clients with a mental illness in Australian emergency departments. J Clin Nurs. 2010;19:712-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Kemball RS, Gasgarth R, Johnson B, Patil M, Houry D. Unrecognized suicidal ideation in ED patients: are we missing an opportunity. Am J Emerg Med. 2008;26:701-705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Bailey S. Critical care nurses’ and doctors’ attitudes to parasuicide patients. Aust J Adv Nurs. 1994;11:11-17. [PubMed] [Cited in This Article: ] |
| 21. | Suokas J, Lonnqvist J. Staff’s attitudes towards patients who attempt suicide. Suicide and its prevention: the role of attitude and imitation. Leiden: E.J. Brill 1989; 227-248. [Cited in This Article: ] |
| 22. | Arslanian-Engoren C. Gender and age bias in triage decisions. J Emerg Nurs. 2000;26:117-124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Canetto SS. She died for love and he for glory: Gender myths of suicidal behavior. Omega 1992-. 1993;26:1-17. [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Suokas J, Suominen K, Lönnqvist J. The attitudes of emergency staff toward attempted suicide patients: a comparative study before and after establishment of a psychiatric consultation service. Crisis. 2009;30:161-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Friedman T, Newton C, Coggan C, Hooley S, Patel R, Pickard M, Mitchell AJ. Predictors of A& amp; E staff attitudes to self-harm patients who use self-laceration: influence of previous training and experience. J Psychosom Res. 2006;60:273-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Chung JY. An exploration of accident and emergency nurse experiences of triage decision making in Hong Kong. Accid Emerg Nurs. 2005;13:206-213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Fliege H, Lee JR, Grimm A, Klapp BF. Risk factors and correlates of deliberate self-harm behavior: a systematic review. J Psychosom Res. 2009;66:477-493. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 263] [Cited by in F6Publishing: 240] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 28. | Wilkinson P, Goodyer I. Non-suicidal self-injury. Eur Child Adolesc Psychiatry. 2011;20:103-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 103] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 29. | Pardey TGM. The clinical practice of Emergency Department Triage: Application of the Australasian Triage Scale--An extended literature review: Part I: Evolution of the ATS. Australas Emerg Nurs J. 2006;9:155-162. [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | McDonough S, Wynaden D, Finn M, McGowan S, Chapman R, Hood S. Emergency department mental health triage consultancy service: an evaluation of the first year of the service. Accid Emerg Nurs. 2004;12:31-38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |