Published online Sep 29, 2022. doi: 10.5495/wjcid.v12.i2.69
Peer-review started: April 22, 2022
First decision: June 16, 2022
Revised: July 1, 2022
Accepted: August 22, 2022
Article in press: August 22, 2022
Published online: September 29, 2022
Intestinal spirochetosis (IS) is caused by Brachyspira colonization of the gastr
A 73-year-old male with peptic ulcer disease and gastroesophageal reflux was evaluated for elevated liver enzymes. He was diagnosed with chronic hepatitis B virus and prescribed entecavir. Additionally, he was leukopenic and had stage 4 liver fibrosis on transient elastography. After 5 mo, the patient returned for esophagogastroduodenoscopy and screening colonoscopy. He denied any gastrointestinal symptoms at that time. Findings included grade I distal esophageal varices, mild portal hypertensive gastropathy, and patchy nodular gastric antral mucosa. On colonoscopy, several polyps were removed. Hem
This case reports the finding of incidental, asymptomatic IS in a leukopenic patient with hepatitis B virus. Conservative management was appropriate.
Core Tip: Intestinal spirochetosis is caused by Brachyspira colonization of the gastrointestinal tract. Some patients are asymptomatic, while others present with gastrointestinal complaints such as abdominal pain, diarrhea, or gastrointestinal bleeding. However, the clinical significance of asymptomatic intestinal spirochetosis is unclear, and guidelines are lacking regarding decision to treat. We report the case of an asymptomatic 73-year-old male with chronic hepatitis B and leukopenia who was incidentally diagnosed with intestinal spirochetosis on pathology of polyps resected during routine screening colonoscopy. He was managed conservatively with careful observation and without antibiotic therapy via a multidisciplinary approach between gastroenterology and infectious disease.
- Citation: Novotny S, Mizrahi J, Yee EU, Clores MJ. Incidental diagnosis of intestinal spirochetosis in a patient with chronic hepatitis B: A case report. World J Clin Infect Dis 2022; 12(2): 69-75
- URL: https://www.wjgnet.com/2220-3176/full/v12/i2/69.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v12.i2.69
Intestinal spirochetosis (IS) is a condition of intestinal colonization with Brachyspira species, typically Brachyspira aalborgi or Brachyspira pilosicoli[1]. The prevalence of IS varies with geographic location. Estimates suggest a prevalence of 11%-64% in developing countries and 1%-5% in North America and Europe[2]. Colonization is more common in people with HIV and men who have sex with men[1]. Patients with IS are more often male, and the mean age at diagnosis is 51[3]. The mode of transmission is not clear; however colonization may result from exposure to infected water, animals, birds, or feces[4]. A literature review was performed focusing on asymptomatic or incidental IS with the following search terms: Intestinal spirochetosis, intestinal spirochaetosis, colonic spirochetosis, colonic spir
A 73-year-old male presented to our gastroenterology practice for follow-up esophagogastroduodenoscopy (EGD) 5 mo after an initial EGD. He simultaneously underwent screening colonoscopy as his last colonoscopy was more than 10 years prior. He was feeling well and reported no gastrointestinal symptoms.
This patient initially underwent EGD 5 mo prior to this visit due to melena and symptomatic anemia. EGD findings were notable for Los Angeles Grade A esophagitis and a large, cratered gastric antral ulcer with pigmented spots. He was diagnosed with peptic ulcer disease and gastroesophageal reflux and was discharged on pantoprazole 40 mg twice daily. At that time, a workup for abnormal liver enzymes revealed a new diagnosis of chronic hepatitis B virus (HBV). He tested negative for HIV, and entecavir was eventually initiated. Transient elastography showed stage 4 liver fibrosis. He was also leukopenic with a white blood cell count ranging from 2700 to 3900.
Additional medical history was notable for hypertension. He denied previously undergoing diagnostic workup for congenital immunodeficiencies. Medications included vitamin D3 50000 units oral daily and folic acid 1 mg oral daily.
Pertinent social history included a history of military service with international travel to Guantanamo Bay, Cuba, and Greece, and remote alcohol and tobacco use. He had one tattoo that was obtained 50 years prior. He denied recent or remote history of unprotected sexual intercourse and denied history of sexually transmitted diseases. Family history was non-contributory.
The patient was evaluated 1 wk prior to his EGD and colonoscopy, at which time he was afebrile and mildly hypertensive to 148/80. Body mass index was 28.6. The patient’s exam was benign, with a soft, non-tender, and non-distended abdomen. Bowel sounds were present and normal.
Laboratory results are shown in Table 1. Notably, ALT was 72 and AST was 57, recorded 5 mo prior to this visit. Prothrombin time and activated partial thromboplastin time were within normal limits at that time. ALT and AST decreased to 41 and 39, respectively, 1 wk prior to this visit. Alkaline phosphatase, bilirubin, total protein, and albumin levels remained within normal limits. He was leukopenic, thrombocytopenic, and had a normocytic anemia 1 wk prior. Infectious disease workup 5 mo prior revealed a positive HBV DNA, positive HBV surface antigen, and negative HBV E Antigen. The patient was retested 1 wk prior to this visit, revealing positive HBV DNA, positive HBV total core antibody, positive HBV E antibody, and negative HBV core IgM.
| Parameter | 5 mo prior | 1 wk prior |
| ALT | 72 | 41 |
| AST | 57 | 39 |
| Alkaline phosphatase | 77 | 88 |
| Total bilirubin | 0.9 | 0.5 |
| Direct bilirubin | Not obtained | 0.2 |
| PT/INR | 12.9/1.2 | Not obtained |
| aPTT | 29.1 | Not obtained |
| Total protein | 7.2 | 7.0 |
| Albumin | 3.7 | 3.8 |
| WBC count | 3.9 | 3.1 |
| Hemoglobin | 9.4 | 10.2 |
| Hematocrit | 27.3 | 30.6 |
| Mean corpuscular volume | 96 | 85 |
| Platelet count | 111 | 104 |
| HBV DNA quantitative viral load | 8.22 log IU/mL | 8.14 log IU/mL |
| HBV surface antigen | Positive | Not obtained |
| HBV core total antibody | Not obtained | Positive |
| HBV core IgM antibody | Not obtained | Negative |
| HBV E antigen | Negative | Not obtained |
| HBV E antibody | Not obtained | Positive |
EGD revealed grade I varices in the distal esophagus, irregular Z-line, mild portal hypertensive gastropathy, and patchy nodular mucosa in the gastric antrum. No ulcers were seen. Colonoscopy revealed multiple small polyps that were resected, diffuse diverticulosis, and non-bleeding hemorrhoids (Figure 1).
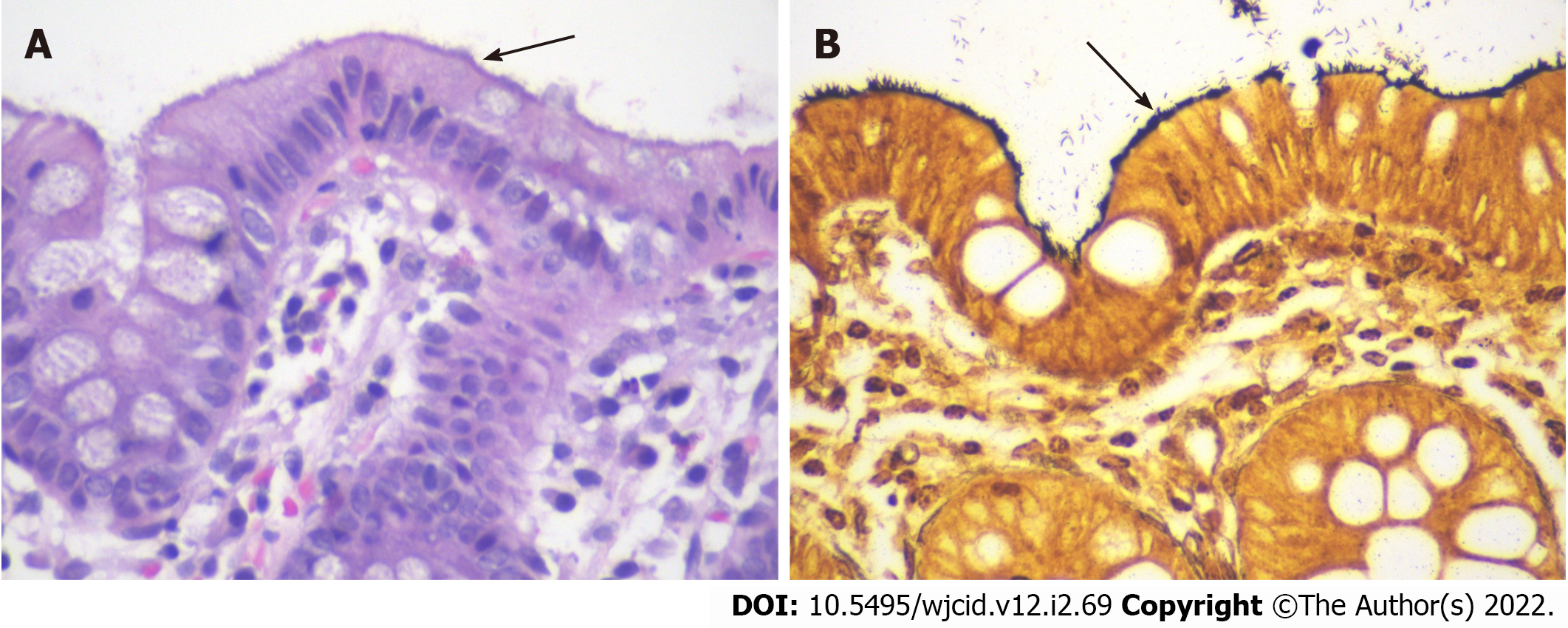
Pathology results of the resected colon polyps showed tubular adenomas, a sessile serrated lesion, and a hyperplastic polyp. Incidentally, a hematoxylin and eosin stain of the colonic mucosa adjacent to the polyps identified intestinal spirochetosis appearing as a “false brush border” (Figure 2A), with a Steiner stain confirming the presence of spirochetes (Figure 2B).
The final diagnosis in this case is asymptomatic IS.
In this case of asymptomatic IS, the patient was managed conservatively without antibiotics.
The patient followed up with both gastroenterology and infectious disease specialists. He remained asymptomatic at the 7-wk follow-up, and a repeat HIV screen at that time was negative. Thus, he was not prescribed antibiotics and was closely followed for development of any gastrointestinal symptoms.
We describe an asymptomatic case of IS diagnosed via histology of tissue obtained during routine colonoscopy. Histologic findings in IS classically include a “brush-like” appearance of organisms oriented perpendicular to the epithelial surface of the intestine[5]. This is consistent with the findings seen on stains of our patient’s colonic tissue. A large study found that 90% of IS biopsies showed no changes on histology other than the presence of spirochetes[6]. However, there have been several reports of histologic changes, notably inflammation with macrophages, neutrophils, eosinophils, and lymphoid follicles on biopsy[6-8]. Our patient represents a case of isolated IS, with identification of spirochetes without any changes on the cellular level.
Additionally, this report describes a case of IS associated with a hyperplastic polyp, tubular adenomas, and a sessile serrated lesion. On colonoscopy, some patients with IS have no remarkable findings, while others have had polyps, mucosal erosions, or ulcerations[5,9]. Several case reports describe findings of IS in patients with colon polyps of varying histology (including adenomatous, hyperplastic, sessile serrated lesions, and other polyps)[10-14].
IS is often an incidental finding, and its clinical implications are unclear. Several reports describe asymptomatic patients found to have spirochete colonization[11,15-18]. However, other reports have described the presence of various gastrointestinal symptoms including diarrhea, changes in bowel habits, abdominal pain, and overt or occult gastrointestinal bleeding[12,17,19-21]. A study of 209 patients with IS found 46% of patients reported abdominal pain, 51% diarrhea, and 13% alternating constipation and diarrhea[3].
Notably, IS has been frequently reported in immunocompromised patients, such as those with HIV or taking immunosuppressive drugs[22-24]. There are additional case reports of IS in patients with chronic HBV[5] and hepatitis C[8,25]. In the present case, leukopenia in the setting of chronic liver disease secondary to HBV may have played a role in the development of spirochete colonization. The origin of this patient’s HBV infection is not certain. His history is notable for having one tattoo, but he denied sexual or military exposures that would otherwise suggest a source for his HBV infection.
As the clinical significance of IS is controversial, need for treatment has been debated. Recommendations from the 2021 European Academy of Dermatology and Venereology Guidelines support treatment for IS with metronidazole 500 mg twice daily or 250 mg three times daily for a 14-d course[1]. However, this recommendation does not differentiate between symptomatic and asymptomatic patients. A large study found that 40% of IS patients received treatment, and of these 86% were treated with metronidazole. However, only 52% of treated patients reported improvements in symptoms[3]. In an earlier study, 17 patients were treated with metronidazole 500 mg three times daily for 10 d, and 15 patients had resolution of symptoms[9]. Evidence is lacking for treatment guidelines in the asymptomatic population. A comprehensive literature search identified a limited number of publications reporting decision to treat in 5 cases of asymptomatic adults with IS. Of these cases, 4 patients were not treated[5,11,16,18]. The fifth patient was treated with metronidazole and experienced resolution of the IS infection[15]. Due to our patient’s continued lack of symptoms, he was not treated with antibiotics and is being managed with close follow-up.
IS is a condition that has not been well-studied. Clinical implications are not clear, and thus treatment guidelines are lacking. Particularly in patients who are asymptomatic, the need for treatment is controversial. This report describes an incidental finding of IS in an asymptomatic patient with a history of HBV and leukopenia. This patient was managed without antibiotics and was followed carefully. He remained asymptomatic 7 wk after diagnosis. When evaluating immunocompromised patients, including those with HIV or viral hepatitis, one should consider the possibility of IS colonization, particularly in patients with gastrointestinal symptoms. This case highlights the feasibility and success of conservative management without use of antibiotic therapy in asymptomatic IS. Additionally, close monitoring with collaboration and shared decision-making between gastroenterologists and infectious disease specialists for asymptomatic IS was beneficial. Future research is needed to evaluate the impact of Brachyspira colonization of the gastrointestinal tract and to establish recommendations for treatment and follow-up, specifically in asymptomatic patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bieńkowski C, Poland; Elshimi E, Egypt S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | de Vries HJC, Nori AV, Kiellberg Larsen H, Kreuter A, Padovese V, Pallawela S, Vall-Mayans M, Ross J. 2021 European Guideline on the management of proctitis, proctocolitis and enteritis caused by sexually transmissible pathogens. J Eur Acad Dermatol Venereol. 2021;35:1434-1443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | Körner M, Gebbers JO. Clinical significance of human intestinal spirochetosis--a morphologic approach. Infection. 2003;31:341-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Weisheit B, Bethke B, Stolte M. Human intestinal spirochetosis: analysis of the symptoms of 209 patients. Scand J Gastroenterol. 2007;42:1422-1427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 4. | Hampson DJ, Oxberry SL, La T. Potential for zoonotic transmission of Brachyspira pilosicoli. Emerg Infect Dis. 2006;12:869-870. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Tong YT, Younes M. Intestinal Spirochetosis: Case Series and Review of the Literature. Ann Clin Lab Sci. 2020;50:386-390. [PubMed] [Cited in This Article: ] |
| 6. | Carr NJ, Mahajan H, Tan KL, Sharma R. The histological features of intestinal spirochetosis in a series of 113 patients. Int J Surg Pathol. 2010;18:144-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Guccion JG, Benator DA, Zeller J, Termanini B, Saini N. Intestinal spirochetosis and acquired immunodeficiency syndrome: ultrastructural studies of two cases. Ultrastruct Pathol. 1995;19:15-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Walker MM, Talley NJ, Inganäs L, Engstrand L, Jones MP, Nyhlin H, Agréus L, Kjellstrom L, Öst Å, Andreasson A. Colonic spirochetosis is associated with colonic eosinophilia and irritable bowel syndrome in a general population in Sweden. Hum Pathol. 2015;46:277-283. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Calderaro A, Bommezzadri S, Gorrini C, Piccolo G, Peruzzi S, Villanacci V, Zambelli C, Dettori G, Chezzi C. Infective colitis associated with human intestinal spirochetosis. J Gastroenterol Hepatol. 2007;22:1772-1779. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Calderaro A, Gorrini C, Montecchini S, Villanacci V, Bassotti G, Dettori G, Chezzi C. Intestinal spirochaetosis associated with hyperplastic and adenomatous colonic polyps. Pathol Res Pract. 2012;208:177-180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Alnimer L, Zakaria A, Warren B. A Case of Human Intestinal Spirochetosis Diagnosed During Screening Colonoscopy. Cureus. 2021;13:e14829. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Lindboe CF, Tostrup NE, Nersund R, Rekkavik G. Human intestinal spirochaetosis in mid-Norway. A retrospective histopathological study with clinical correlations. APMIS. 1993;101:858-864. [PubMed] [Cited in This Article: ] |
| 13. | Omori S, Mabe K, Hatanaka K, Ono M, Matsumoto M, Takahashi M, Yoshida T, Ono S, Shimizu Y, Sugai N, Suzuki A, Katsuki S, Fujii T, Kato M, Asaka M, Sakamoto N. Human intestinal spirochetosis is significantly associated with sessile serrated adenomas/polyps. Pathol Res Pract. 2014;210:440-443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Ngwa T, Peng JL, Choi E, Tayarachakul S, Liangpunsakul S. Colonic Spirochetosis in a 60-Year-Old Immunocompetent Patient: Case Report and Review. J Investig Med High Impact Case Rep. 2016;4:2324709616662671. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Khashab M, Wilson S, Cho WK. Image of the month. Intestinal spirochetosis: an unusual cause of asymptomatic colonic ulceration. Clin Gastroenterol Hepatol. 2010;8:A22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Guzman Rojas P, Catania J, Parikh J, Phung TC, Speth G. Intestinal Spirochetosis in an Immunocompetent Patient. Cureus. 2018;10:e2328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Tanahashi J, Daa T, Gamachi A, Kashima K, Kondoh Y, Yada N, Yokoyama S. Human intestinal spirochetosis in Japan; its incidence, clinicopathologic features, and genotypic identification. Mod Pathol. 2008;21:76-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Esteve M, Salas A, Fernández-Bañares F, Lloreta J, Mariné M, Gonzalez CI, Forné M, Casalots J, Santaolalla R, Espinós JC, Munshi MA, Hampson DJ, Viver JM. Intestinal spirochetosis and chronic watery diarrhea: clinical and histological response to treatment and long-term follow up. J Gastroenterol Hepatol. 2006;21:1326-1333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Alsaigh N, Fogt F. Intestinal spirochetosis: clinicopathological features with review of the literature. Colorectal Dis. 2002;4:97-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Anthony NE, Blackwell J, Ahrens W, Lovell R, Scobey MW. Intestinal spirochetosis: an enigmatic disease. Dig Dis Sci. 2013;58:202-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Green KR, Harris C, Shuja A, Malespin M, De Melo SW Jr. Intestinal Spirochetosis: An Obscure Cause of Lower Gastrointestinal Bleeding. Cureus. 2018;10:e2970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Takezawa T, Hayashi S, Adachi Y, Sunada K, Hayashi Y, Nishimura N, Yano T, Miyata T, Yamamoto H, Hirai Y, Sugano K. Human intestinal spirochetosis in an immunocompromised host: evaluation of eradication therapy by endoscopy, histopathology and bacteriology. Clin J Gastroenterol. 2012;5:69-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Tateishi Y, Takahashi M, Horiguchi S, Funata N, Koizumi K, Okudela K, Hishima T, Ohashi K. Clinicopathologic study of intestinal spirochetosis in Japan with special reference to human immunodeficiency virus infection status and species types: analysis of 5265 consecutive colorectal biopsies. BMC Infect Dis. 2015;15:13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Martinez MW, Petre S, Wisinger D, Temesgen Z. Intestinal spirochetosis and diarrhea, commensal or causal. AIDS. 2004;18:2441-2442. [PubMed] [Cited in This Article: ] |
| 25. | Kantekure K, Tischler A. Intestinal spirochetosis. Int J Surg Pathol. 2014;22:709-710. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |