Published online Aug 29, 2022. doi: 10.5410/wjcu.v11.i1.1
Peer-review started: February 23, 2022
First decision: May 12, 2022
Revised: May 23, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: August 29, 2022
Acute scrotal pain and swelling are common presentations in the emergency department. Urgent surgical intervention is justified in up to one-third of cases, whereas two-thirds of them should be treated conservatively.
We report a case of scrotal only strangulation in a child and review the available literature.
Due to its rarity, scrotal strangulation can be a diagnostic challenge. Skin ulceration and edema may well indicate the presence of a strangulation object. A high index of suspicion and appropriate physical examination, especially in patients with a mental disability or behavioral disorder, are key to early diagnosis and treatment.
Core Tip: An extremely rare etiology of painful scrotal swelling, which emphasizes the paramount importance of the basic physical examination, especially in patients with a mental disability or behavioral disorder.
- Citation: Frumer M, Ben-Meir D. Scrotal strangulation in the differential diagnosis of acute scrotum: A case report. World J Clin Urol 2022; 11(1): 1-5
- URL: https://www.wjgnet.com/2219-2816/full/v11/i1/1.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v11.i1.1
Acute scrotal pain and swelling are common presentations in the emergency department (ED). Urgent surgical intervention is justified in up to one-third of cases, whereas two-thirds of them should be treated conservatively. Common causes of acute scrotal pain in children and adolescents include torsion of the appendix testis, epididymitis, and testicular torsion. Scrotal strangulation by external pressure is an extremely rare cause. We report a case of scrotal only strangulation in a child and review the available literature.
The patient demonstrated bilateral scrotal redness, pain, swelling, and tenderness.
An 11-year-old child was brought to the ED by his parents due to a 5-d history of pain, bilateral scrotal redness, swelling, and tenderness. The child refused to cooperate, and a physical examination was impossible, beyond looking at the scrotum (Figure 1).
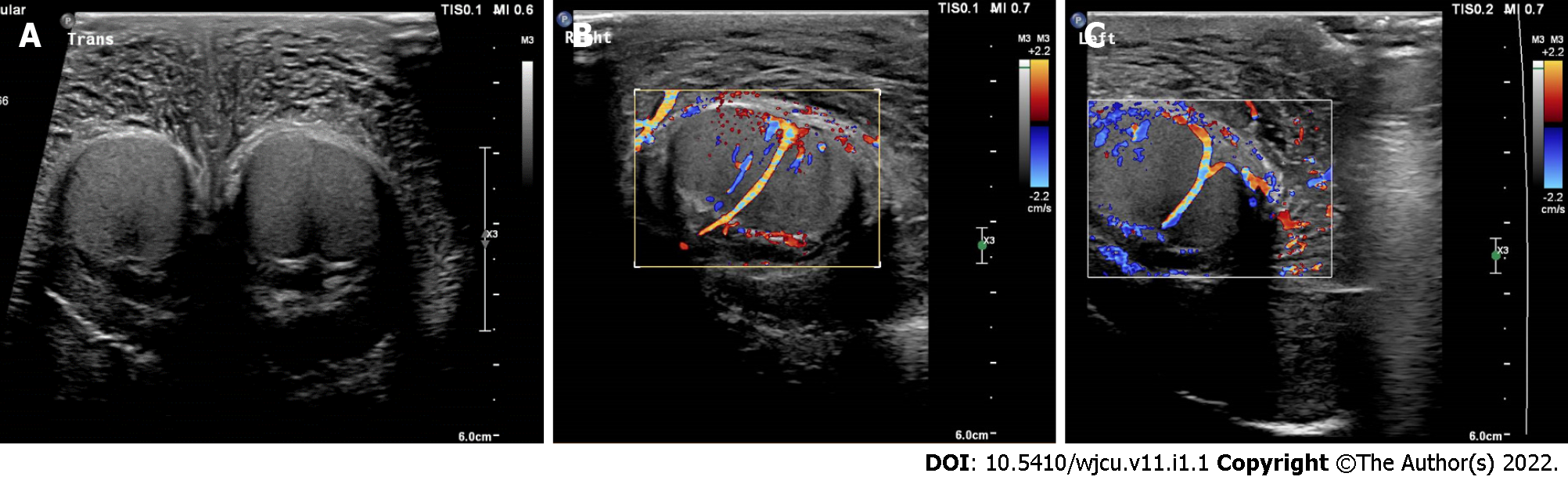
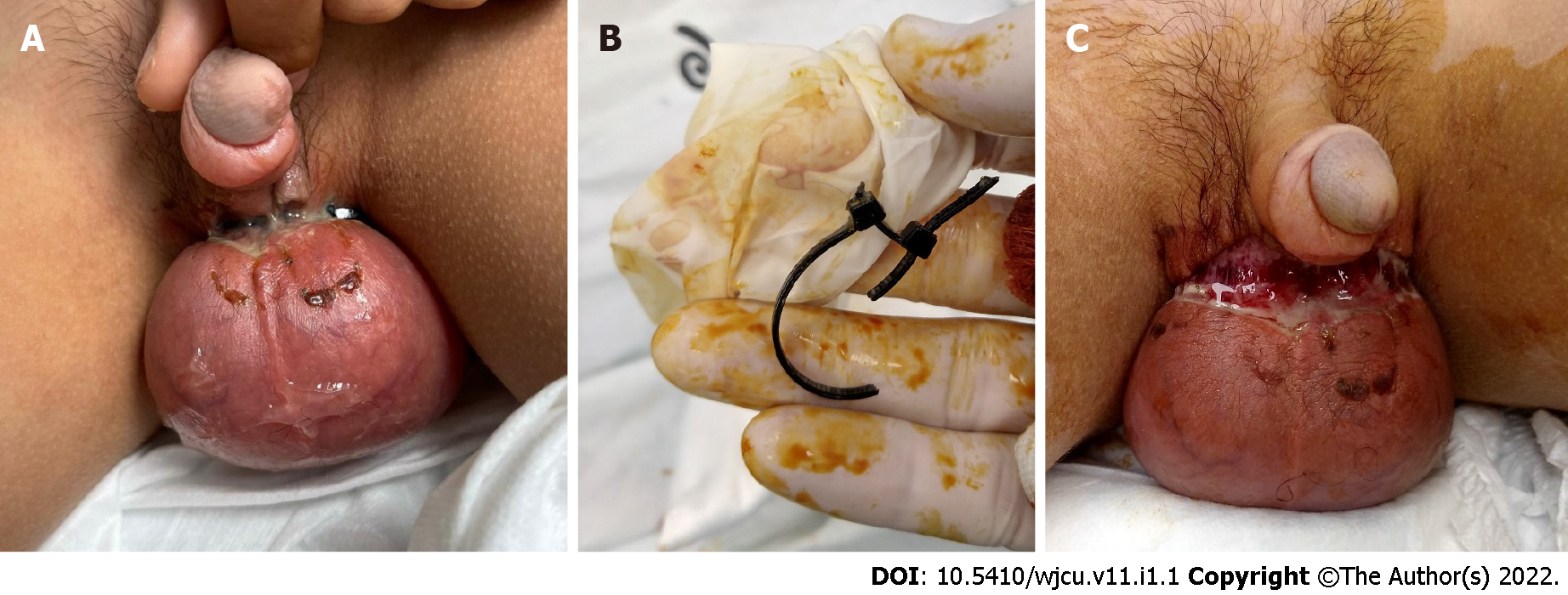
A scrotal Doppler ultrasound was performed, demonstrating normal size and symmetrical testicles with homogeneous echogenicity, bilateral hydrocele, and increased scrotal skin thickness (Figure 2). The child was discharged from the hospital with a diagnosis of idiopathic scrotal edema. His scrotal pain and swelling worsened under treatment with non-steroidal anti-inflammatory drugs, Mebendazole, and antihistamine. After 3 days he revisited the ED, where he refused to undergo a physical examination. The parents agreed to sedate him, and finally a physical examination was carried out using Midazolam. Scrotal strangulation by nylon zip-tie was found (Figure 3).
The child had an intellectual disability.
Physical examination showed bilateral scrotal redness, swelling, and tenderness.
Scrotal Doppler ultrasound demonstrated normal size and symmetrical testicles with homogeneous echogenicity, bilateral hydrocele, and increased scrotal skin thickness (Figure 2).
Scrotal strangulation by a nylon zip-tie.
The zip-tie was removed using regular scissors, relieving the pain within a few minutes.
The scrotal swelling reduced in the following 10 d, and the incision underwent secondary healing in the following month. Psychological evaluation and subsequent assistance by a psychologist and social worker were given to the patient and his parents.
A systematic literature search was performed in PubMed and the Cochrane Library databases up to December 2021. The search key terms included “scrotal entrapment”, "scrotal strangulation", "penoscrotal strangulation", "genital incarceration", and "scrotal incarceration". Inclusion criteria were a diagnosis of scrotal or penoscrotal strangulation. The search yielded 232 articles. Excluded were “penile only strangulation” and “incarcerated scrotal hernias” cases. References in the included papers were checked for relevant cases, and any germane paper found was reviewed in the present study. All demographic and clinical data were recorded.
The key terms retrieved 17 relevant papers from 1994 to 2020 that reported on 19 cases: 16 cases of penoscrotal strangulation and three of scrotal strangulation, including the present case (Supple
The median patient age was 46 years (IQR 55, 34), and the current case is the first report of pediatric scrotal strangulation in the literature. The median time to presentation was 2 d (IQR 1, 3), and 16 (84%) patients did not pose a diagnostic challenge and were diagnosed at the first clinical examination. The other three patients were diagnosed by repeated physical examinations, or by computed tomography and open surgery. The most common constricting device was a metallic ring (74%). Mental illness or drug addiction were present in 5/19 (26.5%) patients and of these, 4/5 (80%) presented with a more severe clinical course or worse outcomes.
Scrotal strangulation is a surgical emergency and an extremely rare etiology of acute scrotum. The rarity is verified in the present study, as only 18 cases of penoscrotal or scrotal strangulation in adults were found in the literature. The current case is the first reported in children.
Patients often present with local pain, swelling, paresthesia, and urinary symptoms[1]. In most cases, medical history was the most useful element in making an accurate diagnosis. Depending on the duration of incarceration, there can also be ulceration and necrosis of the skin, more frequently associated with the use of sharp plastic rather than smooth metal constricting devices. Severe complications such as sepsis or penile amputation and bilateral orchiectomy were reported in three cases, and one of them was fatal[2].
In the present case of an 11-year old boy with limited medical history and poor cooperation, scrotal entrapment by a nylon zip-tie was diagnosed 8 days after the onset of symptoms. The normal appearance of the uninvolved penis and the scrotal swelling obscured the zip-tie, challenging the diagnosis. According to the literature, delay in diagnosis and treatment (including the need for various imaging tests, examination under anesthesia, or surgical exploration) are more frequent in patients with mental illness or drug addiction, causing severe long-term consequences[2-4].
In adults, a wide variety of strangulating objects have been described. In most reported cases, the constrictive devices were used intentionally by the patient, mainly for sexual pleasure. Penile strangulations in children are well reported, with accidental hair-tie strangulation as the most common mechanism[5], although some authors question the rate of accidental cases[6]. Scrotal entrapment is unlikely to occur by accident. Child abuse, violence by peers and siblings, and attention-seeking behavior are all possible causes. Therefore, any penoscrotal or scrotal strangulation in children requires an in-depth investigation.
Due to its rarity, scrotal strangulation can be a diagnostic challenge. Skin ulceration and edema may well indicate the presence of a strangulation object. A high index of suspicion and appropriate physical examination, especially in patients with a mental disability or behavioral disorder, are key to early diagnosis and treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Urological Association. European Society for Paediatric Urology.
Specialty type: Urology and nephrology
Country/Territory of origin: Israel
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bains L, India; Markic D, Croatia; Moralioglu S, Turkey S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | Lu Y, Tan TW, Lau KW. Successful removal of a penoscrotal constricting ring in a 49-year-old male. Asian J Urol. 2017;4:262-264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Patel NH, Schulman A, Bloom J, Uppaluri N, Iorga M, Parikh S, Phillips J, Choudhury M. Penile and Scrotal Strangulation due to Metal Rings: Case Reports and a Review of the Literature. Case Rep Surg. 2018;2018:5216826. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Bart S, Culty T, Pizzoferrato AC, Thibault F, Girault N, Chartier-Kastler E, Richard F. [Complete necrosis of the penis and testes by strangulation in a psychotic patient]. Prog Urol. 2008;18:483-485. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Harris E, Llompart D, Izquierdo G, Aziz MA. Patient With Penile and Scrotal Strangulation Due to Prolonged Use of a Metal Ring Device. Cureus. 2020;12:e11928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | El-Bahnasawy MS, El-Sherbiny MT. Paediatric penile trauma. BJU Int. 2002;90:92-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Saiad MO. Penile injuries in children. Turk J Urol. 2018;44:351-356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |