Published online May 8, 2016. doi: 10.5409/wjcp.v5.i2.191
Peer-review started: January 30, 2016
First decision: March 1, 2016
Revised: March 22, 2016
Accepted: April 7, 2016
Article in press: April 11, 2016
Published online: May 8, 2016
AIM: To hypothesize a dedicated critical care nurse practitioner (NP) is associated with a decreased length of stay (LOS) from a pediatric chronic ventilator dependent unit (PCVDU).
METHODS: We retrospectively reviewed patients requiring care in the PCVDU from May 2001 through May 2011 comparing the 5 years prior to the 5 years post implementation of the critical care NP in 2005. LOS and room charges were obtained.
RESULTS: The average LOS decreased from a median of 55 d [interquartile range (IQR): 9.8-108.3] to a median of 12 (IQR: 4.0-41.0) with the implementation of a dedicated critical care NP (P < 1.0001). Post implementation of a dedicated NP, a savings of 25738049 in room charges was noted over 5 years.
CONCLUSION: Our data demonstrates a critical care NP coverage model in a PCVDU is associated with a significantly reduced LOS demonstrating that the NP is an efficient and likely cost-effective addition to a medically comprehensive service.
Core tip: This is a retrospective study to review the care of patients requiring care in the pediatric chronic ventilator dependent unit from May 2001 to May 2011 comparing the 5 years prior to the 5 years post implementation of the critical care nurse practitioner (NP) in 2005. The average length of stay decreased from a median of 55 d [interquartile range (IQR): 9.8-108.3] to a median of 12 (IQR: 4.0-41.0) with the implementation of a dedicated critical care NP (P < 0.0001). Post implementation of a dedicated NP, a savings of 25738049 in room charges was noted over 5 years.
- Citation: Rowan CM, Cristea AI, Hamilton JC, Taylor NM, Nitu ME, Ackerman VL. Nurse practitioner coverage is associated with a decrease in length of stay in a pediatric chronic ventilator dependent unit. World J Clin Pediatr 2016; 5(2): 191-197
- URL: https://www.wjgnet.com/2219-2808/full/v5/i2/191.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v5.i2.191
Transitioning children with chronic ventilator dependence delivered through a tracheostomy to their home environment reduces costs, enhances their quality of life, and helps with integration back into their families and communities[1]. Especially for children, the hospital is not an ideal location to aid their physical and psychological development[2,3]. However, children with chronic ventilator dependence present unique challenges to discharge planning. In 1998, the American College of Chest Physicians estimated that 10000 to 20000 people were receiving assisted ventilation at home[1]. This number will most likely continue to grow. One study found that pediatric long term ventilation discharges had increased 55% between 2000 and 2006[4]. As the number of patients with home mechanical ventilation increases, their hospital length of stay (LOS) has a multifactorial impact on healthcare usage. These patients have multiple medical problems making medical discharge progress slow. In fact, this group has been shown to have a significantly longer LOS[4]. Families require considerable education and training, specifically in tracheostomy care and ventilator management. The training process and transition to the home environment can be very overwhelming for families[5,6]. Social, insurance and financial issues can delay discharge. Previous studies have shown the addition of a nurse practitioner (NP) to various types of medical care teams significantly reduced the hospital LOS[7-10]. We hypothesize that a dedicated critical care NP would decrease the LOS in a pediatric chronic ventilator dependent unit (PCVDU), thus significantly impacting hospital costs.
Charts were retrospectively reviewed for all patients who required care in the PCVDU from May 2001 through May 2011 to determine the effect of the critical care NP on LOS. This study was done at a large quaternary care pediatric hospital. In May of 2005, a dedicated pediatric nurse practitioner with critical care services was added to the care team for these patients and in October of 2008, an additional pediatric nurse practitioner was hired enabling daily NP coverage of the PCVDU. The NPs received additional training on managing chronic ventilation from the physician director of the Home Ventilator Program via both lectures and bedside instruction. Prior to the introduction of the NPs, the patients were covered only by the attending physician, who was also responsible for the medical care of an additional pediatric intensive care unit. The NPs were involved in the care of all patients requiring mechanical ventilation. They rounded on the patients, helped to formulate care plans for the day, discussed care plan with consultants, participated in care and discharge conferences, and updated families. Their main responsibility was coverage of the PCVDU. They were first line responders for questions from bedside nurses and respiratory therapists (RTs) throughout the day. They modified the plan and initiated orders as needed. Outside of the PCVDU, the NPs served as members of the rapid response and cardiopulmonary resuscitation teams, as well as provided assistance in the pediatric intensive care unit (PICU) as able. The same two NPs were present throughout the study period offering a better continuity of care and, therefore, facilitating ventilator weaning. The pediatric home ventilator program discharge criteria and training closely follows the American Thoracic Society guidelines. Bedside nurses and RT dedicated to this unit trained the family in the child’s daily care and home ventilation.
Patients in the PCVDU were also co-managed by the developmental pediatrics team. This team was responsible for addressing developmental concerns, rehabilitation therapies, nutrition, and arranging outpatient follow up. The developmental team included a pediatric nurse practitioner during the week and resident coverage overnight and on the weekends. The staffing model for the developmental team was unchanged during the study period.
We compared the five years prior to the implementation of the critical care NPs to the five years post implementation. Also, the time with partial NP coverage was then compared to daily NP coverage. Partial coverage was defined as 5 d (approximately 40 h) per week, with the remaining days covered by the attending physician alone. Full NP coverage had a critical care team NP involved in the patient care every day. The NP coverage was only available during the day throughout the study period. The critical care attending physician managed the children overnight. PCVDU LOS, diagnosis, and disposition at discharge were collected. Diagnoses were grouped into seven categories based on the most common diagnoses admitted to our PCVDU: Bronchopulmonary dysplasia (BPD), neurologic disorders, multiple congenital anomalies, congenital heart disease, congenital diaphragmatic hernia, traumatic injury, and miscellaneous.
The financial data for bed/room charges alone was obtained from hospital accounting and did not include physician fees, therapy charges, medications, radiologic studies, or equipment. Room charges were all adjusted for inflation based on 2011 room charge values. Cost-effectiveness was determined by comparing room charges pre and post implementation of an NP.
Our PCVDU is a six bed unit dedicated to the care of children requiring long term mechanical ventilation. The majority of patients developed chronic respiratory failure within the same hospital admission and subsequently required home mechanical ventilator support through a tracheostomy. It comprises a variety a patients with the majority being neonates with BPD, but older children with neurologic, congenital anomalies, cardiac conditions and traumatic injuries are also admitted to this unit. The majority of the admissions are transfers from the neonatal intensive care unit. As such, the families require a comprehensive home mechanical ventilation and tracheostomy education program. Patients admitted to this unit are patients that have been decided to need chronic ventilation via a tracheostomy and have been determined to be safe outside of the PICU. Active ventilator weaning, adjustments and transitions to a home ventilator occur in this unit. Any form of ventilation, i.e., full mechanical support to CPAP is all via tracheostomy. Seldom, when there is a significant shortage of critical care beds, children that have already undergone the initial training are admitted to this unit for other medical or social concerns. The vast majority of patients that have home ventilation and return to the hospital for any reason are admitted to the general PICU service and not the chronic ventilation unit.
Descriptive statistics are given by medians and interquartile ranges (IQRs) for continuous variables. To determine differences between groups, Mann-Whitney U test and the Kruskal-Wallis test were used for continuous variables. Chi squared analysis was used to determine P values for categorical variables. All analytic assumptions were checked to ensure proper outcome reporting. Associations were considered significant at a P-value of < 0.05. We used Statistical Package of the Social Science (SPSS) Statistical software for Windows, Version 20.0 (SPSS Inc., Chicago, IL, United States) and Microsoft Office Excel (Microsoft Corporation, Redmond, WA).
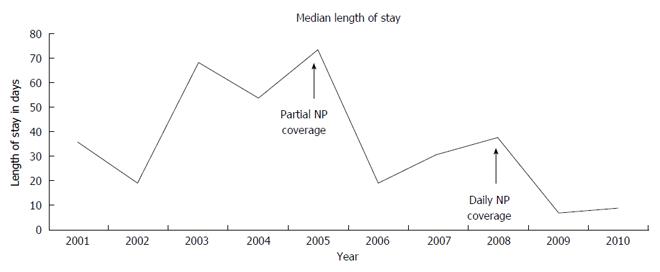
There were 469 admissions identified over the 10 year study period. The admissions’ characteristics before and after beginning of NP coverage are described in Table 1. Demographics for these patients are as follows: The pre-NP coverage group was 38.6% female compared with 46.3% in the post-NP coverage group (P = NS). The pre-NP coverage group had a median age of 6 mo (IQR: 4-12) while the post-NP coverage group had a median age of 12 mo (IQR: 5-30) (P < 0.001). The decrease in the average LOS pre- and post-NP was significant with a P value < 0.0001 (Figure 1).
| Pre NP coverage | Post NP coverage | |
| Total number of admission | 158 | 311 |
| Average annual patient days | 10493 | 8812 |
| Median length of stay | 55 d | 12 d |
| (IQR: 9.8-108.3) | (IQR: 4.0-41.0) |
Daily NP coverage was provided for 200 of the 311 admissions with dedicated critical care NP involvement. The remaining 111 patients had NP coverage 5 d a week. When comparing partial NP coverage to daily NP coverage, there was once again a statistically significant decrease (P < 0.0001) from median 27.5 d (IQR: 7.75-75.25) to median 8 d (IQR: 3.0-28.0) (Figure 2).
There were seven diagnosis groups: BPD, neurologic disorders, multiple congenital anomalies, congenital heart disease, congenital diaphragmatic hernia, traumatic injury, and miscellaneous. BPD was the most common. Table 2 displays the total number of patients admitted with each diagnoses over the 10 year study period.
| Diagnosis | Total admissions | Admissions pre-NP | Admissions post-NP | Length of stay (d) pre-NP | Length of stay (d) post-NP | P value for length of stay |
| Bronchopulmonary dysplasia | 140 | 61 | 79 | 68.0 (11.0-111.0) | 18.0 (3.0-67.0) | P < 0.001 |
| Neurologic disorder | 119 | 35 | 84 | 19.0 (4.0-50.0) | 12.0 (4.0-28.5) | P = 0.246 |
| Multiple congenital anomalies | 94 | 28 | 66 | 62.5 (16.0-126.5) | 10.5 (5-32.8) | P = 0.005 |
| Congenital heart disease | 50 | 18 | 32 | 72.0 (47.5-138.8) | 9.0 (2.3-18) | P < 0.001 |
| Congenital diaphragmatic hernia | 15 | 5 | 10 | 3.0 (1.0-107.0) | 22.5 (8.5-37.8) | P = 0.902 |
| Trauma | 10 | 1 | 9 | 2.0 (2.0-2.0) | 23.0 (4.0-40.0) | Could not be assessed |
| Miscellaneous | 41 | 10 | 31 | 45.5 (13.8-98.3) | 11.0 (5.0-39.0) | P = 0.017 |
When comparing the LOS pre- and post-implementation of the critical care NP by diagnosis, we found a statistically significant decrease in several categories including BPD, congenital anomalies, congenital heart disease, and the miscellaneous group (Table 2).
We also investigated the disposition at discharge and compared the LOS pre- and post-NP. The dispositions at discharge were either to home, general pediatric ward (if the patient no longer required chronic ventilator support), an extended care facility, a rehabilitation facility, an outside hospital (a local community hospital closer to the family’s home), the pediatric intensive care unit, or death. Table 3 illustrates the number of admissions and their disposition at discharge.
| Disposition | Total number of admissions | No. of admissions pre-NP | No. of admissions post-NP | Length of stay (d) pre-NP | Length of stay (d)post-NP | P value |
| Home | 339 | 105 | 234 | 68 (14.0-112.5) | 14 (4.0-48.0) | P < 0.0001 |
| General ward | 32 | 14 | 18 | 13.5 (2.5-124.3) | 4 (1.8-7.3) | P = 0.05 |
| Extended care facility | 19 | 4 | 15 | 37.5 (2.0-148.0) | 5 (3.0-24.0) | P = 0.84 |
| General rehabilitation facility | 3 | 1 | 2 | 27 (27.0-27.0) | 29 (25.0-29.0) | Could not be assessed |
| Outside hospital | 6 | 4 | 2 | 74 (15.0-105.3) | 19 (16.0-19.0) | P = 0.36 |
| PICU | 60 | 25 | 35 | 19 (9.5-49.5) | 12 (5.0-43.0) | P = 0.35 |
| Death | 10 | 5 | 5 | 35 (22.0-62.0) | 13 (2.0-23.0) | P = 0.05 |
The majority of patients were discharged to home. Readmission to this unit is exceedingly low. When chronic ventilation patients return to the hospital, they are admitted to the PICU for acute issues to be resolved. Comparing LOS for these patients discharged home pre- and post-NPs, we found a significant decrease. Table 3 compares LOS pre- and post-NPs for each disposition at discharge.
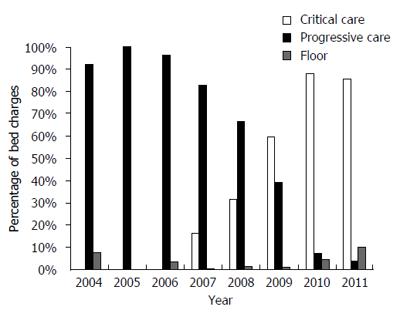
The average room charge per patient stay prior to the NPs was approximately 188437. This charge decreased to approximately 105678 post implementation of the dedicated critical care NP. This is a savings of 82759 for room charges alone per patient per stay. Taking this average savings per patient, 25738049 were saved in room charges over the 5 year period since the start of a dedicated NP to the PCVDU (Figure 2). The NP did not add specific charges to the care of these patients as their services are bundled within the hospital and physician charges.
This study demonstrates a decrease in LOS in a PCVDU with the addition of dedicated critical care NP coverage. The mean LOS was reduced by over 75% (median 55 d compared to 12 d). Our results are similar to other studies showing that that the addition of a NP reduces LOS in trauma patients[8-10]. Our most recent LOS with daily NP coverage (mean 19.82 d) is now below the reported mean LOS of 26.1 d obtained from a multicenter database[4]. The addition of NPs to the medical team has also been linked to shorter emergency department LOS and improved patient flow[11,12]. Adult literature shows a one day reduction in LOS with the addition of a NP to the team[13]. Our study provides one of the first accounts of the association of a NP on LOS in a PCVDU.
A limitation of this study is that it is difficult to retrospectively determine other factors affecting LOS. The pre-NP median patient age and post-NP median patient age are significantly different. This could have affected LOS in the post-NP group. One may consider that discharging an older ventilator dependent child may be easier. An older patient may reach acceptable ventilator settings for home more expediently and/or be generally more stable. These factors may have contributed to shorter LOS.
Some factors that may have affected LOS were minimized. There were no changes in physician groups or physician staffing that provided care for these patients except for the addition of the dedicated NP. We are reporting one institution’s experience and practices may be different at other institutions. The same medical director and clinical nurse specialist of the home ventilator program were involved with the program for the entire study period.
It also would have been beneficial to have family surveys to describe their experience in the PCVDU before and after the implementation of the NPs to describe improved family satisfaction. While we speculate the acuity of illness was increasing throughout the study period and feel this is supported with the increasing amount of critical care charges noted in our PCVDU, we do not have acuity scores to further confirm this speculation.
Another limitation relates to the lack of description of total hospital LOS. Changing admission criteria or longer neonatal or pediatric intensive care unit stays prior to PCVDU may affect LOS. The total hospital LOS in our institution would likely be skewed by the prolonged variable neonatal course many of these patients have prior to being admitted to the PCVDU. A trend toward higher acuity in this unit, supported by the increasing number of critical care charges, may imply that we are admitting patients sooner to the unit. One would expect this to increase LOS, but we actually found a reduction.
The decrease in LOS by the addition of the NPs is likely multifactorial. The addition of a dedicated practitioner allowed for closer monitoring and prompt implementation of necessary ventilator and medication adjustments. This facilitated faster adjustments, allow the patient to more rapidly reach a medically stable state suitable for home. This is evident when examining the LOS pre- and post-NPs for patients discharged to an extended care facility where family education is not imperative. The dedicated NPs also improved coordination of care within our unit, especially with plans surrounding discharge. The NPs could ensure that the proper inter-professional staff, such as social work, nursing, and home care, had all been contacted in a timely fashion when the patient was nearing discharge. This dedicated coordination of care is essential in the successful discharge of ventilator dependent patients[14]. The NP had dedicated time to address concerns regarding family education and training and could be a sounding board for families in stressful situations. They also provided a consistency of care that likely contributed to the reduction in LOS. This is illustrated in our dramatic reduction in LOS for patients who are discharged to home.
This impact on LOS was consistent across diagnoses with the most impressive reduction noted in children with BPD. This is important in our particular population where BPD was the most common underlying diagnosis. While there have been advances in the care of BPD, the most significant advance was the use of surfactant. Our study period takes place after surfactant became a standard of care. Nevertheless, it is likely that advances in modern medicine have contributed to the reduction in LOS that we found in this study. However, the significant drop in LOS despite underlying diagnosis makes it unlikely that this is due to advances in medical care alone. Undoubtedly, we have made some medical progress for many of the underlying diseases seen in our population. Also, with the advancements in technology and increased insurance/hospital costs, the general trend has led to parents caring for sicker children at home[15]. These factors alone are unlikely to be a cause of the significant reduction in LOS. Examining Figure 1, it is noticeable that there has been a trend toward decreasing LOS through the study time period; however, there is a sharp decline around the time of the introduction of partial NP coverage, and another sharp decline around the time of full NP coverage. However, from 2001 to 2003, there seems to be a trend toward increasing LOS. We venture this is secondary to increasing patient acuity. This is supported by a shift in bed charges from floor charges to progressive care charges to critical care charges. This trend toward higher acuity continued even throughout the implementation of the NPs.
We also noted a decrease in LOS across dispositions at discharge, with the most notable being disposition to home. Since the majority of our patients are discharged to home, this has the greatest overall effect on our LOS. We did not find a change in the LOS in those patients that went to the PICU or those that died. This is not surprising. We would not expect a change in the LOS of either of these dispositions. If the child is going to need a higher level of care, this will happen regardless of the presence of an additional member to the team. The latter half of the study period noted an increase in the disposition to a general rehab unit. This correlates with the accreditation of our hospital as a level 1 trauma center causing our patient population to slightly change. The small number of deaths in the unit is generally parental decisions to withdraw support and are probably unaffected by the presence of a dedicated NP.
Our cost savings data is striking. By the addition of full NP coverage for this chronic ventilation unit, we found an estimated reduction in hospital charges over a 5 year period of almost $26 million dollars. This has been accomplished despite an increase in acuity of illness that has led to a shift from progressive care charge to critical care charge, as is illustrated in Figure 2. The above mentioned reduction reflects room charges alone. This financial analysis does not include physician fees, therapy charges, medications, or equipment, which may significantly increase cost savings. There may also be other cost savings advantages by reducing LOS. We speculate that a shorter LOS correlates with decrease in the risk of hospital acquired infections. In addition to patient morbidity and mortality, catheter associated blood stream infections, catheter associated urinary tract infections, and hospital acquired pneumonia all have a significant cost burden on the healthcare system. It is also likely that a shorter LOS improves patient satisfaction. These findings would be important to validate at other pediatric chronic ventilation units.
As the hospital is not the ideal location to aid in the physical and psychological development of children, it is greatly important to transition the child with chronic ventilator dependence delivered via a tracheostomy to their home environment. While the transition reduces costs, enhances the quality of life and places the child with their loving support network, the discharge of this population from the hospital requires advanced planning due to the unique challenges they present. In this study, the authors hypothesized that a dedicated critical care nurse practitioner (NP) would decrease the length of stay (LOS) in a pediatric chronic ventilator dependent unit.
Prior to the introduction of the dedicated NP in the pediatric chronic ventilator dependent unit (PCVDU), each patient was covered only by the attending physician who was also responsible for the medical care of an additional pediatric critical care unit, limiting the time the physician could dedicate to the successful transition of these patients from the hospital to home. The results of this study suggest the success of the dedicated NP in decreasing the LOS for the authors’ chronic ventilator dependent patients.
The dedicated NPs served as the front line staff for the authors’ chronic ventilator dependent patients. The NP for each patient rounded with the medical team, helped to formulate the care plan for the day, discussed the patient’s care with consultants, participated in care conferences, and updated the families. They responded to questions from the respiratory therapists and bedside nurses and had the ability to modify the plan and initiate orders as needed. The dedicated NP served as a key member of the patient’s developmental team during the hospital stay with a focus on discharging the patient to home. The study shows that the addition of the dedicated NP reduced the LOS for the authors’ chronic ventilator patients.
The success of the dedicated NP in the PCVDU at reducing LOS could translate to other units of the hospital, reducing LOS as well as hospital costs.
NP: A nurse practitioner with advanced nursing education; PCVDU: The pediatric chronic ventilator dependent unit; LOS: Length of stay; RT: Respiratory therapist; PICU: Pediatric intensive care unit.
The manuscript is an inspiring work depicting success in implementing nurse practitioners in a discharge process from PCVDU.
P- Reviewer: Mostafa BE, Sangkhathat S, Wang R S- Editor: Ji FF L- Editor: A E- Editor: Wang CH
| 1. | AARC (American Association for Respiratory Care) clinical practice guideline. Discharge planning for the respiratory care patient. Respir Care. 1995;40:1308-1312. [PubMed] [Cited in This Article: ] |
| 2. | Carnevale FA, Alexander E, Davis M, Rennick J, Troini R. Daily living with distress and enrichment: the moral experience of families with ventilator-assisted children at home. Pediatrics. 2006;117:e48-e60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 279] [Cited by in F6Publishing: 257] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 3. | Christmas AB, Reynolds J, Hodges S, Franklin GA, Miller FB, Richardson JD, Rodriguez JL. Physician extenders impact trauma systems. J Trauma. 2005;58:917-920. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 81] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Considine J, Martin R, Smit D, Winter C, Jenkins J. Emergency nurse practitioner care and emergency department patient flow: case-control study. Emerg Med Australas. 2006;18:385-390. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Cowan MJ, Shapiro M, Hays RD, Afifi A, Vazirani S, Ward CR, Ettner SL. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nurs Adm. 2006;36:79-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 109] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Fanta K, Cook B, Falcone RA, Rickets C, Schweer L, Brown RL, Garcia VF. Pediatric trauma nurse practitioners provide excellent care with superior patient satisfaction for injured children. J Pediatr Surg. 2006;41:277-281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Jarrett LA, Emmett M. Utilizing trauma nurse practitioners to decrease length of stay. J Trauma Nurs. 2009;16:68-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Kamm M, Burger R, Rimensberger P, Knoblauch A, Hammer J. Survey of children supported by long-term mechanical ventilation in Switzerland. Swiss Med Wkly. 2001;131:261-266. [PubMed] [Cited in This Article: ] |
| 9. | Make BJ, Hill NS, Goldberg AI, Bach JR, Criner GJ, Dunne PE, Gilmartin ME, Heffner JE, Kacmarek R, Keens TG. Mechanical ventilation beyond the intensive care unit. Report of a consensus conference of the American College of Chest Physicians. Chest. 1998;113:289S-344S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 151] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Margolan H, Fraser J, Lenton S. Parental experience of services when their child requires long-term ventilation. Implications for commissioning and providing services. Child Care Health Dev. 2004;30:257-264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | McManaway C, Drewes B. The role of the nurse practitioner in level II trauma at Nationwide Children’s Hospital. J Trauma Nurs. 2010;17:82-84. [PubMed] [Cited in This Article: ] |
| 12. | Meyer SC, Miers LJ. Cardiovascular surgeon and acute care nurse practitioner: collaboration on postoperative outcomes. AACN Clin Issues. 2005;16:149-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Montagnino BA, Mauricio RV. The child with a tracheostomy and gastrostomy: parental stress and coping in the home--a pilot study. Pediatr Nurs. 2004;30:373-380, 401. [PubMed] [Cited in This Article: ] |
| 14. | Nowotny ML. Life on a ventilator. Home Healthc Nurse. 1999;17:691-694. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Wang KW, Barnard A. Technology-dependent children and their families: a review. J Adv Nurs. 2004;45:36-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 114] [Article Influence: 5.7] [Reference Citation Analysis (0)] |