Published online Nov 20, 2015. doi: 10.5321/wjs.v4.i4.141
Peer-review started: June 20, 2015
First decision: July 27, 2015
Revised: September 25, 2015
Accepted: October 16, 2015
Article in press: October 19, 2015
Published online: November 20, 2015
Autotransplantation of premolars to anterior region after incisor loss due to trauma is accepted as the best restoration procedure with very long follow-ups. There are two main protocols: Premolars with only two thirds of the root or premolars with complete root development. Premolars with two thirds of the root completed remain vital and show complete pulp obliteration while premolars with closed apex require root canal treatment. The problem arises when the child is very young and the root of the donor premolar is developed for only one third. This case report describes the outcome of an autotransplantation of a lower first premolar with only a third of developed root to the anterior region. The donor tooth was extracted with his follicle and placed instead of tooth No. 21. For the first month esthetics was restored with a glass-fibers ribbon attached to tooth No. 11 and composite material. After a month, the crown erupted and was reshaped to mimic an incisor with composite. Orthodontic movement was performed after 5 mo, in order to alleviate the gingival contour. The final restoration was performed after 15 mo. Follow up showed full root development with normal mobility, continuous periodontal ligament and complete pulp obliteration. A multidisciplinary approach and meticulous preparation are necessary for a positive result in autotransplantation of premolars with only a third of root development to the anterior region and this case report show that this method can be performed in very young children.
Core tip: Autotransplantation of a premolar to the anterior region has a success rate of more than 90% if the donor tooth has a developing root and pulp healing occurs. The only negative outcome is total obliteration of the pulp. This case report describe an autotransplantation of a lower first premolar with only a third of root length to the incisor area after a dental trauma that caused root resorption of a permanent upper left incisor, in a 8-year-old boy. Follow up of 15 mo showed full root growth and periodontal healing with normal mobility and obliteration of the pulp. The crown was restored using composite material to resemble the adjacent incisor. This case report shows that even with very short donor root length, autotransplantation to the anterior region can be performed in young children.
- Citation: Zilberman U, Zagury A. Autotransplantation of a premolar to the maxillary anterior region in young children - how long should the donor root be? A case report. World J Stomatol 2015; 4(4): 141-145
- URL: https://www.wjgnet.com/2218-6263/full/v4/i4/141.htm
- DOI: https://dx.doi.org/10.5321/wjs.v4.i4.141
The method of autotransplantation of premolars to maxillary anterior region in order to replace severely traumatized permanent incisors is known for more than 40 years[1,2]. There are two main protocols regarding the stage of root development of the donor premolars - full root development[3] or half to two thirds root length[1,4]. The survival rate of premolars with complete root formation was 100% after 5 years and 72.7% after 10 years[3] and the survival rate of premolars with half to two-thirds root formation was 100% after 6-78 mo follow-up[5]. and the success rate was 91.3%. Pulp healing of the autotransplanted premolar is related to root development. For premolars with half to two thirds root length pulp healing was observed in 96% of the premolars after 6 mo follow-up[5] while for premolars with complete root length pulp healing was observed in only 15%[5], implicating that root canal treatment is necessary after autotransplantation in premolars with full root length and closed apex. The major sign for pulp healing was obliteration of the pulp and normal periodontal ligament[5]. The problem is that the minimal age for autotransplantation should be between 9-10 years, when the donor premolar has half-two thirds of root length, while for root length of less than half absence of further root development was observed[6]. But sometimes the autotransplantation have to be performed earlier. This case report describe a successful autotransplantation of a lower first premolar with only a third of root length for an upper left incisor in an 8-year-old boy with a follow-up of 15 mo.
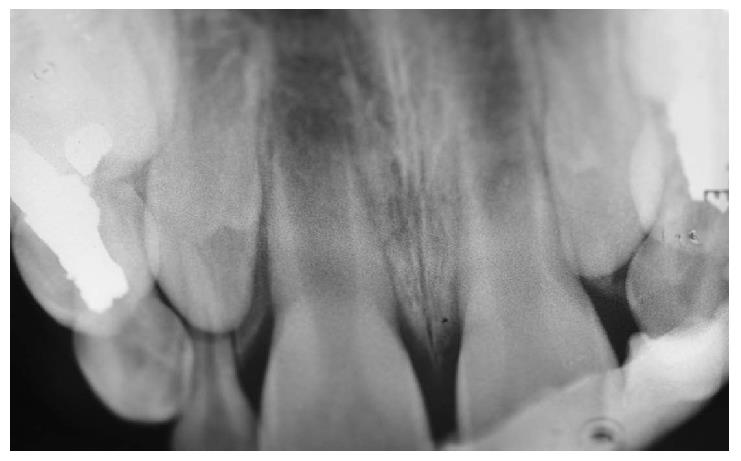
OB, a 7-year-old boy arrived to the pediatric dental unit at Barzilai medical center two days after a head trauma at school. The avulsed upper left central incisor was kept in dry condition and was re-implanted 3 h after the trauma at a different hospital. The tooth was splinted to the adjacent teeth with composite (Figure 1). Two weeks after the trauma, the splint was removed and the pulp canal was filled with calcium hydroxide paste. At follow-up visit after 3 mo the root was resorbed and mobility of 2 mm was observed. A split with glass-fibers ribbon was performed (Figures 2 and 3). After 12 mo and four more traumas to the tooth, the option of autotransplantation was described to the child and the parents. Under general anesthesia, tooth No. 21 was extracted (Figure 4), and germ of tooth No. 34 was exposed from the buccal aspect, without damaging tooth No. 74 (Figure 5). The premolar was extracted with the full follicle and reimplanted rotated and infra-occluded at the site of tooth No. 21, and kept in place with cross-over sutures (Figures 6 and 7). For esthetic reasons tooth No. 21 was restored using fiber-glass ribbon attached to tooth No. 11 and composite material (Figure 8). Ten days after the auto-transplantation, the sutures were removed. A month after the surgery the composite and the glass-fiber ribbon were removed and the crown of tooth No. 21 was reconstructed on top of the erupted premolar and splinted to tooth No. 11 with glass-fibers ribbon (Figure 9). Two months after surgery root development was observed. Five months after surgery, forced eruption of the autotransplanted tooth was performed in order to bring the gingival margin at the same height as tooth No. 11. The brackets were removed 4 mo later (Figure 10). At the last follow-up visit, 15 mo after the surgery, the root was completed, the mobility was similar to tooth No. 11, and the pulp was obliterated completely. A new composite restoration was performed for better esthetic (Figures 11 and 12).
Autotransplantation of premolars to the anterior region subsequent to trauma have several advantages in comparison to other modalities, especially for young children. A tooth transplant keeps the alveolar margin at optimal height and facilitates continuous growth of the maxillary complex. It also keeps the bucco-palatal dimension of the alveolar bone in the very esthetic region. The transplanted tooth allows also orthodontic movements, necessary for gingival margin reconstruction. For premolars with half to three forth root formation, pulp and periodontal healing was reported in 80% of the cases after 14 years[7]. Complete pulp obliteration, followed by continuous root formation was positively related to autotransplant viability. Clinical variables for transplanted premolars were found to be similar to the natural incisors when the mean age of surgery was 11 years[8]. A slight increased mobility was observed but the crown-root ratio and the distance between the CEJ and alveolar bone crest was similar to the adjacent incisor after a mean follow-up period of 4 years[8]. The size of the apical foramen, as long as the apex is not closed, seems not to be a very important factor for successful revascularization and ingrowth of new tissue after transplantation in dogs[9]. Resorption of the root was higher in reimplanted teeth with more than three-quarters or apex-closed stages. The authors described that teeth with root length of less than one-half had a higher probability of having arrested root growth, but no description was given to the type of the donor tooth, and the higher failure rate was observed during the first year after transplantation. Other esthetic and restorative options for missing permanent upper centrals at young age include removable flipper with acrylic tooth or orthodontic device with bands on the molars and acrylic tooth on orthodontic wire, till after the puberty growth is completed and an intra-osseous implant can be placed. The main problems with the removable or orthodontic appliances are the accumulation of plaque, the compliance of the child and his family and the possibility of losing the removable appliance or dislodgement of the orthodontic bands. Moreover, the alveolar bone will be resorbed till the insertion of the implant causing a marked discrepancy in gingival contour between the implant and the adjacent incisor. Auto-transplantation results in favorable growth of the alveolar bone and reconstruction of the gingival contour. Successful tooth transplantation offers almost ideal esthetics, arch form and dentofacial development. A transplanted tooth diminishes the extent of resorption of newly formed alveolar bone and provides functional stimulation. Periodontal healing is usually completed after 8 wk and is affected mainly by infection at the host site due to improper postoperative control of supragingival plaque.
The case report showed that for young patients, premolars with only one third of root length can be considered suitable for autotransplantation in the anterior region after loss of incisors due to trauma. Fifteen months follow-up showed complete root length formation, obliteration of the pulp, favorable crown/root ratio and mobility similar to the adjacent incisor. Orthodontic movement was performed in order to reconstruct a similar gingival margin and the reconstruction of the crown was performed using composite material. The final clinical result was highly accepted by both the patient and the parents. More follow-up is needed, but this case shows that autotransplantation of premolars to the anterior area can be performed even in young children.
An 8-year-old boy with no significant medical history, with an upper left central incisor with total root resorption after avulsion and unsuccessful re-implantation.
Esthetic replacement of the lost upper permanent incisor is needed.
Removable orthodontic appliance with an acrylic tooth, fixed orthodontic appliance with an acrylic tooth, autotransplantation of a premolar, till implant insertion and crown restoration can be performed. Autotransplantation of a lower first premolar with only a third of root length was performed.
Success of autotransplantation of premolars to upper anterior region was related to the length of the donor tooth root. Better success rate were observed with root length of half-two thirds.
Autotransplantation of a premolar to replace a lost upper permanent incisor can be performed very early when the root length is only a third. This method results in a very esthetic and long lasting restoration that can be performed in very young children after dental trauma.
Excellent written, the weaknesses are that the method is common knowledge with very high successful rate but this case report remind the audience of this possibility to restore missing permanent incisor after dental trauma.
P- Reviewer: Chen SS, Cho SY S- Editor: Tian YL L- Editor: A E- Editor: Li D
| 1. | Slagsvold O, Bjercke B. Autotransplantation of premolars with partly formed roots. A radiographic study of root growth. Am J Orthod. 1974;66:355-366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 116] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Slagsvold O, Bjercke B. Indications for autotransplantation in cases of missing premolars. Am J Orthod. 1978;74:241-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 95] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Yoshino K, Kariya N, Namura D, Noji I, Mitsuhashi K, Kimura H, Fukuda A, Kikukawa I, Hayashi T, Yamazaki N. Survival rate in autotransplanted premolars with complete root formation: a retrospective clinical survey. Bull Tokyo Dent Coll. 2013;54:27-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Czochrowska EM, Stenvik A, Bjercke B, Zachrisson BU. Outcome of tooth transplantation: survival and success rates 17-41 years posttreatment. Am J Orthod Dentofacial Orthop. 2002;121:110-119; quiz 193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 237] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 5. | Andreasen JO, Paulsen HU, Yu Z, Bayer T, Schwartz O. A long-term study of 370 autotransplanted premolars. Part II. Tooth survival and pulp healing subsequent to transplantation. Eur J Orthod. 1990;12:14-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 291] [Cited by in F6Publishing: 297] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 6. | Denys D, Shahbazian M, Jacobs R, Laenen A, Wyatt J, Vinckier F, Willems G. Importance of root development in autotransplantations: a retrospective study of 137 teeth with a follow-up period varying from 1 week to 14 years. Eur J Orthod. 2013;35:680-688. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Mendoza-Mendoza A, Solano-Reina E, Iglesias-Linares A, Garcia-Godoy F, Abalos C. Retrospective long-term evaluation of autotransplantation of premolars to the central incisor region. Int Endod J. 2012;45:88-97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 8. | Czochrowska EM, Stenvik A, Album B, Zachrisson BU. Autotransplantation of premolars to replace maxillary incisors: a comparison with natural incisors. Am J Orthod Dentofacial Orthop. 2000;118:592-600. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 110] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Laureys WG, Cuvelier CA, Dermaut LR, De Pauw GA. The critical apical diameter to obtain regeneration of the pulp tissue after tooth transplantation, replantation, or regenerative endodontic treatment. J Endod. 2013;39:759-763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |