Revised: September 8, 2014
Accepted: October 14, 2014
Published online: November 2, 2014
Psoriasis comprises severe skin problems affects on quality of patient’s life. It affects 2% of the general population with age before 35 years old. Most potent and cheap psoriatic drugs are still largely unavailable. Recently, as aresult of the apparent side effects of chemical drugs, treatments of herbal origin gains the popularity among patients with skin disorders especially those for psoriasis. In this review, the uses of complementary and alternative medications of various topical herbal formulae with different potency against psoriasis was greatly assessed. Modified Psoriasis scoring systems were performed as evident of improvement when various topical herbal formula including traditional chinese medicine ingredients such as Camptotheca acuminate, Oleum horwathiensis, Capsaicin, furocoumarins, Curcumin, and Tars were used against psoriasis. Also, plant extracts of Aleo Vera, and green tea were reported in topical form for the treatment of psoriasis. Most studies indicated a variety of biological activities of used herbs depending on their chemical constituents. This versatile range of biological activities explaining, the apparent benefits of these herbs in monitoring of psoriasis.
Core tip: Herbal medicine plays a significant role in the treatment of psoriasis; this review gives a shed of light on some herbal medicine formulae and extracts including Aleo Vera, and green tea. These plants extracts and its formulae exhibited efficiency as anti-psoriasis agents. This may relate to the varying biological activities especially tissue repair actions.
- Citation: Gabr SA, Alghadir AH. Phytotherapy and psoriasis: Complementary and alternative medications. World J Dermatol 2014; 3(4): 86-91
- URL: https://www.wjgnet.com/2218-6190/full/v3/i4/86.htm
- DOI: https://dx.doi.org/10.5314/wjd.v3.i4.86
Psoriasis occurs in most populations with a range of 1%-3%[1,2]. As usual, synthesized drugs are more potent in psoriases, however severe unexpected binary effects will appeare with long period of drug use. Under advice of dermatologists, about 50% of psoriatic patients around the world used complementary interventions[3-8]. These include herbal medicine[9,10]; which applied to psoriatic patients with different formulae, topically[11]; internally[12]; and in combination with other forms like acitretin[13]. The biological activities of these constituents were discussed in most literatures[14,15]. Whereas these interventions were prescribed to patients alone or in combinations with different forms[16,17], to perform the targeted therapeutic effect with limited side effects.
Due to the beneficial prospects of traditional chinese medicine (TCM), it was applied in management of various dermatological conditions[18]. However, much concerns should performed regarding the safety of Chinese herbal treatment. Whereas, a bnormal actions as liver toxicity was reported during treatment[19-21]. So, the biological activities of some plant extracts used alone or in different combination forms against psoriasis were greatly reported in this review.
According to the type of diagnosis, it was reported as dermal disorders with varying shapes and severe lesions. This disease prevails a mong people with age ranges from 15-45 years. The extant of disease usually appears with chronic symptoms[22]. Many factors ranged between genetic, apoptotic, cellular, and immunological parameters were attributed with the pathological severity of the disease[23-25]. The diagnosis of the disease depends manily up on the type, location, and area of lesions or plaques. These parameters were included in many disease scoring systems. The most useful one is psoriasis area and severity index score which evaluated to measure disease severity especially during treatment trials[26-32].
For most dermatologic disorders, TCM with different formulations were used as an alternative method of therapy[33]. Each part of the palnt can be used as source for herbal remedies to words many diseases[34,35]. The diversity of both function and plant parts used, promotes specialists developing new forms of biologically active constituents with minimum hazards[7,36]. Whereas, natural plants provide the essential requirements for human safty. It was reported that TCM is special good choice for many patients which in turn requires a well experienced dermatologists to select the more convenient TCM[37]. So, with TCM patients can be treated safely with little side effects[38]. The use of TCM in various forms to treat psoriasis depend mainly on the type of disease. Whereas each type has the recommended and definite mixture of herbs for treatment[39].
Local formulae of indigo plant was efficiently used to treat patients with severe psoriasis. However, recent ideas were discussed to enhance the potency of this crude herb by preparing extracts with better convenience and absorption[40]. Camptotheca acuminata decne is another example of active topical agents in china[41]. The biological activities of this herb mainly due to its alkaloids content with antineoplastic activities[42]. In open clinical trials, the efficiency of this topical agent was applied for many cases with psoriasis. The data showed that Camptotheca acuminate decne was significantly more effective with noticed possible enhancement of post inflammatory hyper- pigmentation[43]. Whereas, in another study a hazard effect like dermal allergy was reported against camptotheca acuminate decne which depends mainly on the type and disease intinisty[44-47]. Besides of local trials, some injectable forms of TCMs like Radix macrotomiae seu Lithospermi was used with better potent and minimum side effects against psoriasis compared to other forms of therapeutic modalities[7]. Similar to Western medications, another type of TCMs were used in capsules or tablets forms for monotherapies or in groups of herbs with higher safty and efficiency. It was found that, three years follow-up of psoriatic cases treated orally with TCM showed convenient results with no hematological or biochemical abnormalities compared to chemotherapeutic agents[19,48].
Extensive growing evidence was reported for using natural plant forms to treat psoriatic patients. Complementary and alternative medicine (CAM) was used by most patients as a complementary treatment along with conventional treatment. So, teaching of CAM should be integrated into the dermatology residency curriculum, and dermatologists need to increase their awareness of CAM use by their patients in order to improve therapeutic communication[49].
Aloe vera extract: The plant characterized by its succulent pulpy leaves which contain clear gel. This plant was used since ancient times as potent remedy for many diseases[47,48]. The versatile range of its active constituents as analgesic, antipruritic, wound healing and anti-inflammatory promotes its use as good anti-psoriatic agent[50].
In double-blind, placebo-controlled study, 0.5% of local forms of Aloe vera extract were subjected for the treatment of psoriasis with diagnostic scores between 4.8 and 16.7 (mean 9.3). The data concluded that 0.5% of the extract has higher efficiency with no hazards, and could be used as successful herbal treatment against psoriasis[51]. However, in other study a commercial Aloe vera gel form showed modest effective treatment against psoriasis[52].
Oleum horwathiensis formula: Oleum horwathiensis formula contains many herbal constituents which showed higher potency in local forms against psoriasis. These constituents are; Achillaea herba, allium sativum, Calendula flos, Taraxaci radix, Urtica folium and Veronica officinalis. This herb was applied locally to treat psoriasis with varying severity. The results showed a promising effect against disease severity after 12 wk[53].
Capsaicin formula: It is the most popular active constituent present in cayenne pepper (C. frutescens) showed a probable activity towords psoriasis[54], through activation of cellular apoptotic factors[55]. Zero point zero two five percent of this formula was applied as local cream to enhance the psoriatic status of patients with varying disease intinisty. The data obtained showed an obvious decrease in disease severity within short period of time, however a minimum hazard effect like local site burning was reported, so the formulae was advised to be applied for only 2 successive days[56,57].
Furocoumarins formula: This formula contains many active agents obtained from different herbal plants including Ammi majus. The anti psoriatic activity of this formula depends mainly on photoactivation of furocoumarins via ultraviolet A (UV-A, 320-400 nm) when applied either locally or in oral forms. The activity mainly depend up on activation of skin cell apoptosis via photochemical linkage with DNA strands and in turn DNA fragmentation. Consequently, a reduction in overexpression of inflammatory and proliferative proteins was reported within psoriatic lesions[58]. These activity was further investigated in relation to standard therapy, the data obtained showed similar enhancement of disease profile with minimum side effects[59,60].
Curcumin formula of turmeric (Curcuma longa): This active formula is extracted from the rhizome of Curcuma longa plant, it is the most potent polyphenolic compound present as fumaric acid[61]. The extract is characterized by its versatile activities ranged between anti-inflammatory, antioxidant, antitumor, and anti microbial activities[33], the mode of action against tumor is through regulation of the role of some cellular and immunological parameters during cell cycle and apoptosis[62]. For centuries, it was reported that Turmeric was applied to heal wounds and reduce scare formation[63]. Similary, curcumin showed a significant enhancement of psoriatic lesions when applied locally on diseased skin or orally through capsules. The extract worked via induction of skin cell apoptosis[64-67].
Tars formula: It is one of the most efficient herbal formula applied since past times to treat skin disorders. This active ingredient was extracted from many herbal plants like birch (Betula spp.), beech (Fagus spp.), or juniper (Juniperus spp.) trees. The extract was applied as anti-psoriatic agent in different forms with 5%-10% concentration. The improvement capacity of extract depends on photoactivation mechanism using UV-B with varying light intinisty[68].
Green tea potential benefits for psoriasis: Tea considered the second worldwide beverage next to water. It consumed as green, black, or Oolong tea. It was reported that green tea is the most important agent targeting human health[69]. This may be related to its higher content of polyphenolic compounds, like flavanols and catechins, whereas dried green tea leaves produce more than 30% of these active constituents. Most studies indicated that green tea constituents have awide range of medical uses as antioxidant, antimicrobial, anti-tumor, anti-inflammatory, and thermogenic agents[70,71]. The vriable actions of green tea constituents along with its photo suppression action promotes dermatologists to use it as conventional treatment for skin diseases, especially psoriasis[72-75].
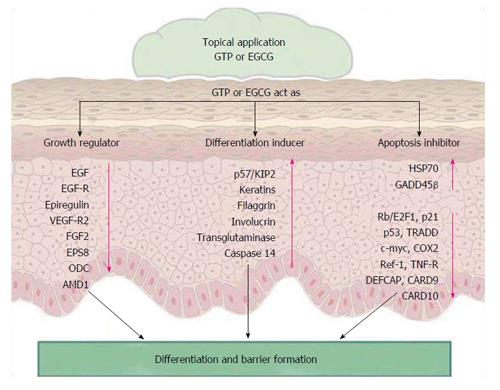
The treatment of skin with green tea extracts protect the skin from developing skin cancer through damaging DNA via photochemical action of ultraviolet A radiation[76]. It was reported that green tea or its active constituents when applied in psoriatic skin, promotes the formation of skin cell apoptosis via activation of certain apoptotic biological enzymes included in epidermal differentiation, cornification of the epidermal keratinocytes and skin barrier formation[77-82]. Finally, the activity of green tea against psoriasis summarized in, activation of a set of apoptotic genes which promotes epidermal differentiation and skin barrier formation along with enhancement of the healing process as in Figure 1[83-87].
Clinical trials proved a significant potential benefits of herbs against psoriasis which appeared relatively safe. The varied biological activities of these topical herbal formulae may relate to its apparent benefits in psoriasis. Most advanced trials like molecular screening were needed for discovering new leads and drug safe candidates from plant natural products against psoriasis.
P- Reviewer: Manolache L, Naldi L S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Christophers E. Psoriasis--epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 577] [Cited by in F6Publishing: 548] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 2. | Langley RG, Krueger GG, Griffiths CE. Psoriasis: epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005;64 Suppl 2:ii18-ii23; discussion ii24-ii25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 319] [Cited by in F6Publishing: 438] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 3. | Baron SE, Goodwin RG, Nicolau N, Blackford S, Goulden V. Use of complementary medicine among outpatients with dermatologic conditions within Yorkshire and South Wales, United Kingdom. J Am Acad Dermatol. 2005;52:589-594. [PubMed] [Cited in This Article: ] |
| 4. | Fuhrmann T, Smith N, Tausk F. Use of complementary and alternative medicine among adults with skin disease: updated results from a national survey. J Am Acad Dermatol. 2010;63:1000-1005. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Jensen P. Use of alternative medicine by patients with atopic dermatitis and psoriasis. Acta Derm Venereol. 1990;70:421-424. [PubMed] [Cited in This Article: ] |
| 6. | Smith N, Weymann A, Tausk FA, Gelfand JM. Complementary and alternative medicine for psoriasis: a qualitative review of the clinical trial literature. J Am Acad Dermatol. 2009;61:841-856. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Lin XR. Psoriasis in China. J Dermatol. 1993;20:746-755. [PubMed] [Cited in This Article: ] |
| 8. | Ouyang H. Progress in the treatment of psoriasis with TCM or western medicine. Guid J Tradit Chin Med Pharm. 2007;13:1-8. [Cited in This Article: ] |
| 9. | Steele T, Rogers CJ, Jacob SE. Herbal remedies for psoriasis: what are our patients taking? Dermatol Nurs. 2007;19:448-450, 457-463. [PubMed] [Cited in This Article: ] |
| 10. | Traub M, Marshall K. Psoriasis--pathophysiology, conventional, and alternative approaches to treatment. Altern Med Rev. 2007;12:319-330. [PubMed] [Cited in This Article: ] |
| 11. | Li N, Li YQ, Li HY, Guo W, Bai YP. Efficacy of externally applied Chinese herbal drugs in treating psoriasis: a systematic review. Chin J Integr Med. 2012;18:222-229. [PubMed] [Cited in This Article: ] |
| 12. | May BH, Zhang AL, Zhou W, Lu CJ, Deng S, Xue CC. Oral herbal medicines for psoriasis: a review of clinical studies. Chin J Integr Med. 2012;18:172-178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Feng X, Xu L. Traditional Chinese medicine plus a citretin for psoriasis: a Meta-analysis on randomized controlled trials. J Tianjin Med Univ. 2008;14:487-491. [Cited in This Article: ] |
| 14. | Reuter J, Wölfle U, Weckesser S, Schempp C. Which plant for which skin disease? Part 1: Atopic dermatitis, psoriasis, acne, condyloma and herpes simplex. J Dtsch Dermatol Ges. 2010;8:788-796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Tse TW. Use of common Chinese herbs in the treatment of psoriasis. Clin Exp Dermatol. 2003;28:469-475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Chan BC, Hon KL, Leung PC, Sam SW, Fung KP, Lee MY, Lau HY. Traditional Chinese medicine for atopic eczema: PentaHerbs formula suppresses inflammatory mediators release from mast cells. J Ethnopharmacol. 2008;120:85-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Sucher NJ. The application of Chinese medicine to novel drug discovery. Expert Opin Drug Discov. 2013;8:21-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 18. | Bedi MK, Shenefelt PD. Herbal therapy in dermatology. Arch Dermatol. 2002;138:232-242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 122] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Sheehan MP, Atherton DJ. A controlled trial of traditional Chinese medicinal plants in widespread non-exudative atopic eczema. Br J Dermatol. 1992;126:179-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 204] [Cited by in F6Publishing: 214] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Armstrong NC, Ernst E. The treatment of eczema with Chinese herbs: a systematic review of randomized clinical trials. Br J Clin Pharmacol. 1999;48:262-264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 21. | Boneberger S, Rupec RA, Ruzicka T. Complementary therapy for atopic dermatitis and other allergic skin diseases: facts and controversies. Clin Dermatol. 2010;28:57-61. [PubMed] [Cited in This Article: ] |
| 22. | von de Kerkof P, Schalkwijk J. Psoriasis. Dermatology. 2nd ed. Mosby Elsevier: Spain 2008; 125-149. [Cited in This Article: ] |
| 23. | Farber EM, Bright RD, Nall ML. Psoriasis. A questionnaire survey of 2,144 patients. Arch Dermatol. 1968;98:248-259. [PubMed] [Cited in This Article: ] |
| 24. | Coimbra S, Figueiredo A, Castro E, Rocha-Pereira P, Santos-Silva A. The roles of cells and cytokines in the pathogenesis of psoriasis. Int J Dermatol. 2012;51:389-395; quiz 395-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 25. | Raychaudhuri SP. A cutting edge overview: psoriatic disease. Clin Rev Allergy Immunol. 2013;44:109-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Louden BA, Pearce DJ, Lang W, Feldman SR. A Simplified Psoriasis Area Severity Index (SPASI) for rating psoriasis severity in clinic patients. Dermatol Online J. 2004;10:7. [PubMed] [Cited in This Article: ] |
| 27. | Fleischer AB, Rapp SR, Reboussin DM, Vanarthos JC, Feldman SR. Patient measurement of psoriasis disease severity with a structured instrument. J Invest Dermatol. 1994;102:967-969. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 68] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Faust HB, Gonin R, Chuang TY, Lewis CW, Melfi CA, Farmer ER. Reliability testing of the dermatology index of disease severity (DIDS). An index for staging the severity of cutaneous inflammatory disease. Arch Dermatol. 1997;133:1443-1448. [PubMed] [Cited in This Article: ] |
| 29. | Sugai J, Ozawa A, Kawakubo Y, Iizuka M, Miyahara M, Ohkido M. New method for determining prognosis of patients with psoriasis (E-PAP). J Dermatol Sci. 1998;16:165-169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Kirby B, Fortune DG, Bhushan M, Chalmers RJ, Griffiths CE. The Salford Psoriasis Index: an holistic measure of psoriasis severity. Br J Dermatol. 2000;142:728-732. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 116] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 31. | Harari M, Shani J, Hristakieva E, Stanimirovic A, Seidl W, Burdo A. Clinical evaluation of a more rapid and sensitive Psoriasis Assessment Severity Score (PASS), and its comparison with the classic method of Psoriasis Area and Severity Index (PASI), before and after climatotherapy at the Dead-Sea. Int J Dermatol. 2000;39:913-918. [PubMed] [Cited in This Article: ] |
| 32. | Callen JP, Krueger GG, Lebwohl M, McBurney EI, Mease P, Menter A, Paller AS, Pariser DM, Weinblatt M, Zimmerman G. AAD consensus statement on psoriasis therapies. J Am Acad Dermatol. 2003;49:897-899. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 84] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Koo J, Arain S. Traditional Chinese medicine for the treatment of dermatologic disorders. Arch Dermatol. 1998;134:1388-1393. [PubMed] [Cited in This Article: ] |
| 34. | Fleischer AB, Feldman SR, Rapp SR, Reboussin DM, Exum ML, Clark AR. Alternative therapies commonly used within a population of patients with psoriasis. Cutis. 1996;58:216-220. [PubMed] [Cited in This Article: ] |
| 35. | Li FQ, Fang FY, Jian ZY. Cases suffering from psoriasis treated with traditional Chinese medicine and long wave ultraviolet. Chin J Phys Ther. 1983;6:144-145. [Cited in This Article: ] |
| 36. | Chen LZ. Treating 23 cases of psoriasis with indirubin tablets. J Clin Dermatol. 1981;10:157-158. [Cited in This Article: ] |
| 37. | Jerner B, Skogh M, Vahlquist A. A controlled trial of acupuncture in psoriasis: no convincing effect. Acta Derm Venereol (Stockh). 1997;77:154-156. [Cited in This Article: ] |
| 38. | Rosted P. Treatment of skin diseases with acupuncture: a review. J Dermatol Treat. 1995;6:241-242. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Zhao F, Wang P, Hua S. Treatment of psoriasis with acupuncture and cupping therapy. Chin Acupunct Moxibust. 1991;11:16-19. [Cited in This Article: ] |
| 40. | Lin YK, Chang CJ, Chang YC, Wong WR, Chang SC, Pang JH. Clinical assessment of patients with recalcitrant psoriasis in a randomized, observer-blind, vehicle-controlled trial using indigo naturalis. Arch Dermatol. 2008;144:1457-1464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 41. | Institute of Dermatology, Sichuan Province. An observation of treating 33 cases of psoriasis with camtothecin. Sichuan Bull Chn Herb. 1973;2:7. [Cited in This Article: ] |
| 42. | Horwitz SB. Camptothecin. Antineoplastic and Immunosuppressive Agents, Part II. New York, NY: Springer-Verlag NY Inc 1976; 649-656. [Cited in This Article: ] |
| 43. | Xarin L. Clinical observation and experimental study on the effect of camptotheca acuminate tincture in treating psoriasis. Chinese Journal of Dermatology. 1982;15:210-212. [Cited in This Article: ] |
| 44. | Ng SK. Topical traditional Chinese medicine. A report from Singapore. Arch Dermatol. 1998;134:1395-1396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Zhang H, Gu J. Progress of experimental study on treatment of psoriasis by Chinese medicinal monomer and single or compound recipe in Chinese materia medica. Chin J Integr Med. 2007;13:312-316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 46. | Xu Y. Dermatology in Traditional Chinese Medicine. St. Albans, UK: Donica Publishing Ltd 2004; . [Cited in This Article: ] |
| 47. | Shishodia S, Sethi G, Aggarwal BB. Curcumin: getting back to the roots. Ann N Y Acad Sci. 2005;1056:206-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 448] [Cited by in F6Publishing: 430] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 48. | Zeng QT. Camptotheca acuminata decne. The Pharmacology and Application of Chinese Traditional Medicine. Beijing, China: Peoples Health Publishing 1983; 142-1151. [Cited in This Article: ] |
| 49. | Zhao WP. Clinical observation of 206 cases of psoriasis treated with Bian Zheng Shi Zhi of traditional Chinese medicine. J Trad Chin Med. 1989;30:31-32. [Cited in This Article: ] |
| 50. | Ben-Arye E, Ziv M, Frenkel M, Lavi I, Rosenman D. Complementary medicine and psoriasis: linking the patient’s outlook with evidence-based medicine. Dermatology. 2003;207:302-307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 41] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 51. | Klein AD, Penneys NS. Aloe vera. J AM Acad Dermatol. 1988;18:714-720. [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 129] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 52. | Shelton RM. Aloe vera. Its chemical and therapeutic properties. Int J Dermatol. 1991;30:679-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 136] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 53. | Duke JA. CRC Handbook of Medicina1 Herbs. Boca Raton, FL: CRC Press 1985; 31-32. [Cited in This Article: ] |
| 54. | Syed TA, Ahmad SA, Holt AH, Ahmad SA, Ahmad SH, Afzal M. Management of psoriasis with Aloe vera extract in a hydrophilic cream: a placebo-controlled, double-blind study. Trop Med Int Health. 1996;1:505-509. [PubMed] [Cited in This Article: ] |
| 55. | Paulsen E, Korsholm L, Brandrup F. A double-blind, placebo-controlled study of a commercial Aloe vera gel in the treatment of slight to moderate psoriasis vulgaris. J Eur Acad Dermatol Venereol. 2005;19:326-331. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 56. | Lassus A, Forsström S. A double-blind study comparing oleum horwathiensis with placebo in the treatment of psoriasis. J Int Med Res. 1991;19:137-146. [PubMed] [Cited in This Article: ] |
| 57. | McGuffin M, Hobbs C, Upton R, Goldberg A, editors . Botanical Safety Handbook. Boca Raton, FL: CRC Press 1997; . [Cited in This Article: ] |
| 58. | Surh YJ, Han SS, Keum YS, Seo HJ, Lee SS. Inhibitory effects of curcumin and capsaicin on phorbol ester-induced activation of eukaryotic transcription factors, NF-kappaB and AP-1. Biofactors. 2000;12:107-112. [PubMed] [Cited in This Article: ] |
| 59. | Bernstein JE, Parish LC, Rapaport M, Rosenbaum MM, Roenigk HH. Effects of topically applied capsaicin on moderate and severe psoriasis vulgaris. J Am Acad Dermatol. 1986;15:504-507. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 125] [Cited by in F6Publishing: 129] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 60. | Ellis CN, Berberian B, Sulica VI, Dodd WA, Jarratt MT, Katz HI, Prawer S, Krueger G, Rex IH, Wolf JE. A double-blind evaluation of topical capsaicin in pruritic psoriasis. J Am Acad Dermatol. 1993;29:438-442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 128] [Cited by in F6Publishing: 134] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 61. | Van Wyk B, Wink M. Medicinal Plants of the World. Portland, OR: Timber Press 2004; . [Cited in This Article: ] |
| 62. | Huang MT, Smart RC, Wong CQ, Conney AH. Inhibitory effect of curcumin, chlorogenic acid, caffeic acid, and ferulic acid on tumor promotion in mouse skin by 12-O-tetradecanoylphorbol-13-acetate. Cancer Res. 1988;48:5941-5946. [PubMed] [Cited in This Article: ] |
| 63. | Chaturvedi TP. Uses of turmeric in dentistry: an update. Indian J Dent Res. 2009;20:107-109. [PubMed] [Cited in This Article: ] |
| 64. | Heng MC, Song MK, Harker J, Heng MK. Drug-induced suppression of phosphorylase kinase activity correlates with resolution of psoriasis as assessed by clinical, histological and immunohistochemical parameters. Br J Dermatol. 2000;143:937-949. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 127] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 65. | Aziz HA, Peh KK, Tan YT. Solubility of core materials in aqueous polymeric solution effect on microencapsulation of curcumin. Drug Dev Ind Pharm. 2007;33:1263-1272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 66. | Kuroda Y, Hara Y. Antimutagenic and anticarcinogenic activity of tea polyphenols. Mutat Res. 1999;436:69-97. [DOI] [Cited in This Article: ] [Cited by in Crossref: 357] [Cited by in F6Publishing: 361] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 67. | Alschuler L. Green Tea: Healing tonic. Am J Natur Med. 1998;5:28-31. [Cited in This Article: ] |
| 68. | Graham HN. Green tea composition, consumption, and polyphenol chemistry. Prev Med. 1992;21:334-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1281] [Cited by in F6Publishing: 1072] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 69. | Ichihashi M, Ahmed NU, Budiyanto A, Wu A, Bito T, Ueda M, Osawa T. Preventive effect of antioxidant on ultraviolet-induced skin cancer in mice. J Dermatol Sci. 2000;23 Suppl 1:S45-S50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 70. | Balasubramanian S, Efimova T, Eckert RL. Green tea polyphenol stimulates a Ras, MEKK1, MEK3, and p38 cascade to increase activator protein 1 factor-dependent involucrin gene expression in normal human keratinocytes. J Biol Chem. 2002;277:1828-1836. [PubMed] [Cited in This Article: ] |
| 71. | Bikle DD, Ng D, Tu CL, Oda Y, Xie Z. Calcium- and vitamin D-regulated keratinocyte differentiation. Mol Cell Endocrinol. 2001;177:161-171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 147] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 72. | Bollinger Bollag W, Bollag RJ. 1,25-Dihydroxyvitamin D(3), phospholipase D and protein kinase C in keratinocyte differentiation. Mol Cell Endocrinol. 2001;177:173-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 73. | Nickoloff BJ, Qin JZ, Chaturvedi V, Bacon P, Panella J, Denning MF. Life and death signaling pathways contributing to skin cancer. J Investig Dermatol Symp Proc. 2002;7:27-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 63] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 74. | Lippens S, Kockx M, Knaapen M, Mortier L, Polakowska R, Verheyen A, Garmyn M, Zwijsen A, Formstecher P, Huylebroeck D. Epidermal differentiation does not involve the pro-apoptotic executioner caspases, but is associated with caspase-14 induction and processing. Cell Death Differ. 2000;7:1218-1224. [PubMed] [Cited in This Article: ] |
| 75. | Madison KC. Barrier function of the skin: “la raison d’être” of the epidermis. J Invest Dermatol. 2003;121:231-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 788] [Cited by in F6Publishing: 674] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 76. | Zhao JF, Zhang YJ, Jin XH, Athar M, Santella RM, Bickers DR, Wang ZY. Green tea protects against psoralen plus ultraviolet A-induced photochemical damage to skin. J Invest Dermatol. 1999;113:1070-1075. [PubMed] [Cited in This Article: ] |
| 77. | Ahmad M, Srinivasula SM, Hegde R, Mukattash R, Fernandes-Alnemri T, Alnemri ES. Identification and characterization of murine caspase-14, a new member of the caspase family. Cancer Res. 1998;58:5201-5205. [PubMed] [Cited in This Article: ] |
| 78. | Pistritto G, Jost M, Srinivasula SM, Baffa R, Poyet JL, Kari C, Lazebnik Y, Rodeck U, Alnemri ES. Expression and transcriptional regulation of caspase-14 in simple and complex epithelia. Cell Death Differ. 2002;9:995-1006. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 79. | Eckhart L, Ban J, Fischer H, Tschachler E. Caspase-14: analysis of gene structure and mRNA expression during keratinocyte differentiation. Biochem Biophys Res Commun. 2000;277:655-659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 80. | Rendl M, Ban J, Mrass P, Mayer C, Lengauer B, Eckhart L, Declerq W, Tschachler E. Caspase-14 expression by epidermal keratinocytes is regulated by retinoids in a differentiation-associated manner. J Invest Dermatol. 2002;119:1150-1155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 81. | Lippens S, VandenBroecke C, Van Damme E, Tschachler E, Vandenabeele P, Declercq W. Caspase-14 is expressed in the epidermis, the choroid plexus, the retinal pigment epithelium and thymic Hassall’s bodies. Cell Death Differ. 2003;10:257-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 82. | Hsu S, Yamamoto T, Borke J, Walsh DS, Singh B, Rao S, Takaaki K, Nah-Do N, Lapp C, Lapp D. Green tea polyphenol-induced epidermal keratinocyte differentiation is associated with coordinated expression of p57/KIP2 and caspase 14. J Pharmacol Exp Ther. 2005;312:884-890. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 83. | Walsh DS, Borke JL, Singh BB, Do NN, Hsu SD, Balagon MV, Abalos RM. Psoriasis is characterized by altered epidermal expression of caspase 14, a novel regulator of keratinocyte terminal differentiation and barrier formation. J Dermatol Sci. 2005;37:61-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 84. | Hsu S, Lewis JB, Borke JL, Singh B, Dickinson DP, Caughman GB, Athar M, Drake L, Aiken AC, Huynh CT. Chemopreventive effects of green tea polyphenols correlate with reversible induction of p57 expression. Anticancer Res. 2003;21:3743-3748. [PubMed] [Cited in This Article: ] |
| 85. | Hsu S, Bollag WB, Lewis J, Huang Q, Singh B, Sharawy M, Yamamoto T, Schuster G. Green tea polyphenols induce differentiation and proliferation in epidermal keratinocytes. J Pharmacol Exp Ther. 2003;306:29-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 107] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 86. | Wei H, Zhang X, Zhao JF, Wang ZY, Bickers D, Lebwohl M. Scavenging of hydrogen peroxide and inhibition of ultraviolet light-induced oxidative DNA damage by aqueous extracts from green and black teas. Free Radic Biol Med. 1999;26:1427-1435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 7] [Reference Citation Analysis (0)] |
| 87. | Proniuk S, Liederer BM, Blanchard J. Preformulation study of epigallocatechin gallate, a promising antioxidant for topical skin cancer prevention. J Pharm Sci. 2002;91:111-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |