Revised: July 13, 2012
Accepted: September 26, 2012
Published online: October 2, 2012
Primary cutaneous anaplastic large cell lymphoma (C-ALCL) is regarded as an indolent type of cutaneous T-cell lymphoma. However, a few recent publications revealed that C-ALCL patients with initial leg involvement had significantly worse survival than those without initial leg involvement. Herein, we report a case of C-ALCL with subsequent leg involvement, which led to death after chemoradiation therapy. A 75 years old Japanese man presented with multiple erythematous nodules in his left arm and the side of his left chest. Histopathological and immunohistochemical studies led to the diagnosis of primary C-ALCL. At the initial diagnosis, no leg lesion was found. One year after the initial diagnosis, C-ALCL appeared in his right lower thigh and left hip. Radiation therapy, low-dose etoposide and CHOP therapy were performed; however, the patient died of malignant lymphoma 4 years after the initial diagnosis. We speculated that the occurrence of subsequent leg involvement may also be indicative of a worse prognosis, as in the case with initial leg involvement in C-ALCL. Therefore, we propose that C-ALCL patients with initial or subsequent leg involvement should be classified as a distinct clinicopathological variant of C-ALCL (“leg-type” involvement) and that they may require intense therapy.
- Citation: Ishida M, Fujii N, Okabe H. Primary cutaneous anaplastic large cell lymphoma with subsequent leg involvement. World J Dermatol 2012; 1(3): 38-40
- URL: https://www.wjgnet.com/2218-6190/full/v1/i3/38.htm
- DOI: https://dx.doi.org/10.5314/wjd.v1.i3.38
Primary cutaneous anaplastic large cell lymphoma (C-ALCL) is a member of the primary cutaneous CD30-positive T-cell lymphoproliferative disorders group, which is the second most common type of cutaneous T-cell lymphoma[1]. The prognosis of C-ALCL is usually favorable, with a 10 year disease-related survival of approximately 90%[1]. However, a few recent publications revealed that C-ALCL patients with leg involvement had worse survival than those without leg involvement[2,3].
Herein, we report a case of C-ALCL with subsequent leg involvement, which led to death after chemoradiation therapy.
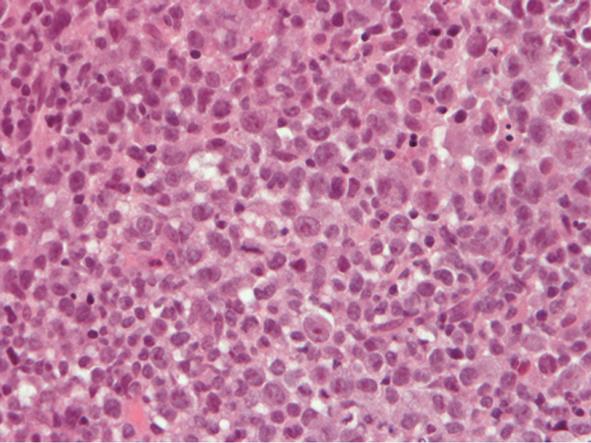
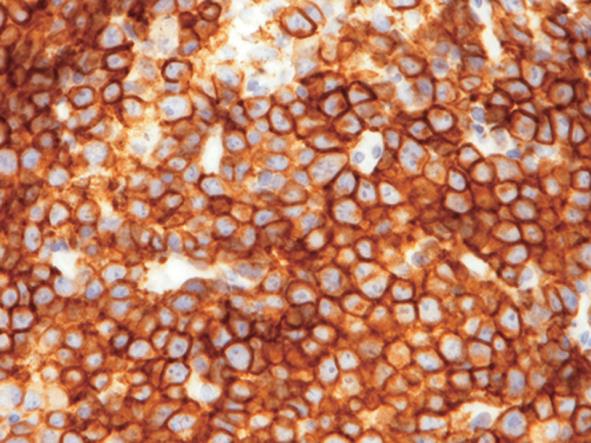
A 75 years old Japanese man, with no evidence of immunosuppression, presented with multiple erythematous nodules in his left arm and the side of his left chest. The biopsy specimen from his left arm nodule revealed diffuse infiltrate with cohesive sheets of large atypical lymphocytes without epidermotropism in the dermis. These atypical lymphocytes had large round to oval nuclei with prominent nucleoli and rich eosinophilic cytoplasm (Figure 1). Immunohistochemically, the atypical lymphocytes expressed CD3, CD4, CD30 and epithelial membrane antigen (Figure 2). Granzyme B and T cell intracellular antigen-1 were also expressed in some of the atypical lymphocytes but they were negative for CD15, CD56 and anaplastic lymphoma kinase protein. These histopathological and immunohistochemical findings were typical for C-ALCL. In addition, gene analysis revealed clonal rearrangement of the T cell receptor C β gene. Physical examination and systemic computed tomography did not reveal any lymph node and visceral lesions. All these findings led to the diagnosis of primary C-ALCL. At the initial diagnosis, no leg lesion was found.
After the diagnosis, resection of the nodules and radiation therapy were performed. During the medical follow-up, some nodules showed spontaneous remission.
One year after the initial diagnosis, erythematous nodules appeared in his right lower thigh and left hip, although the erythematous nodules in his arm and chest had mostly disappeared. The histopathological and immunohistochemical features of his right lower thigh specimen were the same as those of the first biopsy specimen. Radiation therapy and administration of low-dose etoposide were performed; however, the nodules continued to enlarge and increase in number. CHOP therapy was added but the patient died of malignant lymphoma 4 years after the initial diagnosis.
Primary C-ALCL is regarded as an indolent type of cutaneous T-cell lymphoma[1]. Risk factors that predict an unfavorable course in patients with C-ALCL are largely unknown. However, previous studies suggested that patients who are older than 60 years of age and have multifocal skin lesions and the absence of spontaneous remission show correlation with unfavorable prognosis. Recently, Benner and Willemze[2] analyzed the clinical outcome of 18 cases of C-ALCL with generalized skin lesions. Three of 11 cases with leg involvement at initial presentation died of malignant lymphoma, compared with none of the 7 cases without any initial leg involvement. In addition, in the patients with a regional skin lesion, initial leg involvement was associated with reduced 5 years disease-specific survival[2]. These results indicate that C-ALCL patients with initial leg involvement have significantly worse survival than those without initial leg involvement. However, they did not present any data regarding whether subsequent leg involvement, as seen in the present case, shows a poor prognosis or not. We speculate that the occurrence of subsequent leg involvement may also be indicative of a worse prognosis, as in the case with initial leg involvement in C-ALCL.
Moreover, Benner and Willemze emphasized that C-ALCL patients with regional and generalized skin lesions that involve the leg should be monitored very closely and may require systemic chemotherapy at an earlier phase of disease progression[2], although the therapeutic guideline created by Bekkenk et al[4] indicates that in patients with regional skin lesions, excision and radiotherapy are the first choice of treatment, whereas in patients with multiple lesions, low-dose oral methotrexate and/or radiotherapy are preferred.
In conclusion, if dermatologists encounter a patient with subsequent leg involvement, as seen in the present case, careful observation is expected to determine whether the patient will show an aggressive clinical course or not. Further clinicopathological studies are needed to clarify the therapeutic strategies for C-ALCL with subsequent leg involvement.
Peer reviewer: Luca Negosanti, MD, Plastic Surgery Department, S.Orsola-Malpighi Hospital, Via Massarenti 9, 40138 Bologna, Italy
S- Editor Gou SX L- Editor Roemmele A E- Editor Zheng XM
| 1. | Ralfkiaer E, Willemze R, Pauli M, Kadin ME. Primary cutaneous CD30-positive T-cell lymphoproliferative disorders. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. Lyon: IARC Press 2008; 300-301. [Cited in This Article: ] |
| 2. | Benner MF, Willemze R. Applicability and prognostic value of the new TNM classification system in 135 patients with primary cutaneous anaplastic large cell lymphoma. Arch Dermatol. 2009;145:1399-1404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Liu HL, Hoppe RT, Kohler S, Harvell JD, Reddy S, Kim YH. CD30+ cutaneous lymphoproliferative disorders: the Stanford experience in lymphomatoid papulosis and primary cutaneous anaplastic large cell lymphoma. J Am Acad Dermatol. 2003;49:1049-1058. [PubMed] [Cited in This Article: ] |
| 4. | Bekkenk MW, Geelen FA, van Voorst Vader PC, Heule F, Geerts ML, van Vloten WA, Meijer CJ, Willemze R. Primary and secondary cutaneous CD30(+) lymphoproliferative disorders: a report from the Dutch Cutaneous Lymphoma Group on the long-term follow-up data of 219 patients and guidelines for diagnosis and treatment. Blood. 2000;95:3653-3661. [PubMed] [Cited in This Article: ] |