INTRODUCTION
New developments in technology have tremendous impact on managing trauma patients in austere conditions. Occasionally, hospitals can be destroyed or be out of function being stressed with lack of power, large number of trauma patients, and a need for rapid triage[1-3]. Mass casualty incidents (MCIs) occur when the medical needs of injured patients exceed the available medical resources[4,5]. Radiological workup of these patients, in this scenario, is important for accurate diagnosis and triage. So, any disaster management plan should include radiological workup as an integral part of it with full engagement of radiologists[6]. Trauma Computed tomography (CT) scan is not available worldwide and even difficult to transport to the pre-hospital setting. In contrast, high quality portable light ultrasound machines have been used in the pre-hospital setting[6,7]. They have rechargeable batteries that can last up to 4 h[3]. This is a great advantage compared with CT scans and conventional heavy X-ray machines. Point-of-care ultrasound (POCUS) is noninvasive, rapid, and repeatable and can be combined with clinical examination to make critical decisions in triage and resuscitation of shocked patients[8,9].
BASIC PHYSICS OF ULTRASOUND
Piezoelectric crystals of the ultrasound probes produce ultrasound waves and receive them. When these waves pass through body tissues, they get reflected depending on the density of the tissues. On the brightness (B) mode ultrasound images, fluids will be black, soft tissues will be grey, fibrous tissues will be white without a shadow, and bones will be bright white with a shadow. Accordingly, the cortex of long bones will be a white line with a black shadow deeper to it (Figure 1). Reverberation artifact which appears deeper to the cortical hyperdense white line occurs because ultrasound waves bounce between the transducer and the bone cortex. The white reverberation lines represent repetition of the cortical hyperdense white line as picked up by the ultrasound machine. The distance between these lines are equal[10] (Figure 1B). This simple principle is pivotal for mastering diagnosing fractures. Fractures will appear as a complete interruption of the hyperechoic cortical line of the bone or as a cortical defect (Figures 2 and 3).
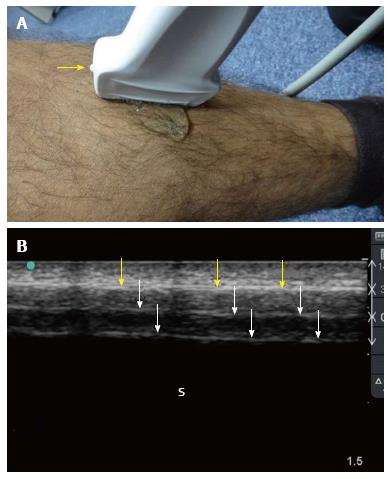
Figure 1 Ultrasound examination of the tibial shaft.
A linear probe having a frequency of 10-12 MHz was used (A). The marker (yellow arrow) is pointing proximally. The plain surface of the tibia makes the examination easy. Normal ultrasound findings (B) include a hyperechoic line (yellow arrows) representing the cortical line of the bone. There are reverberation artifacts deeper to this line (white arrows). These are linear lines parallel to the cortex, having the same distance between them and decreasing in density. A black shadow is located deeper to that. S: Sonographic shadow of the shaft of the tibia. Ultrasound study was performed by Professor Fikri Abu-Zidan, Department of Surgery, Al-Ain Hospital, Al-Ain, UAE.
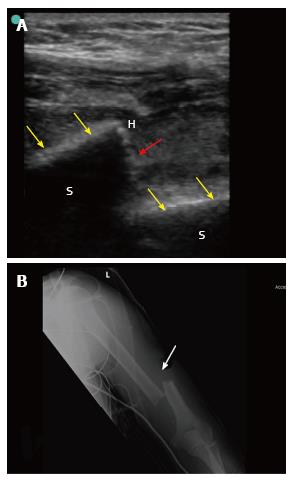
Figure 2 Point-of-care ultrasound of a 42-year-old laborer who fell from 8 meters high during work.
The patient presented with pain, swelling and deformity of the left arm. He had left wrist drop. B mode point-of-care ultrasound of the humeral shaft using a linear probe having a frequency of 10-12 MHz (A) showed that the white cortical line of the humeral shaft (yellow arrows) has been interrupted by a large gap (red arrow) suggesting a displaced fracture at the shaft. X-ray of the humerus (B) confirmed the presence of a displaced fracture (white arrow). S: Sonographic shadow of the humeral shaft; H: Hematoma at the edge of the fracture. Ultrasound study was performed by Professor Fikri Abu-Zidan, Department of Surgery, Al-Ain Hospital, Al-Ain, UAE.
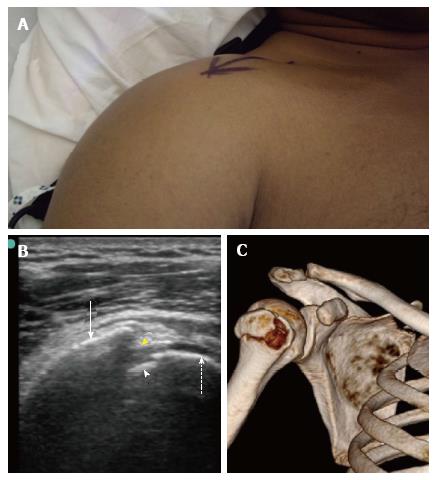
Figure 3 Point-of-care ultrasound of a 40-year-old front seat male passenger who was involved in a front impact collision with a tree.
When presenting to the hospital, he had severe pain, swelling and limitation of the movement of the right shoulder (A). B mode point-of-care ultrasound of the right shoulder using a linear probe having a frequency of 10-12 MHz (B) shows that the humeral head (dashed arrow) and the greater humeral tuberosity (white arrow). There is a discontinuity of the bony line (yellow arrow head) indicating a fracture in the greater tuberosity. A small piece of fractured bone is also seen near the humeral head (white arrow head). Three-dimensional bony reconstruction of the right shoulder confirms the ultrasound findings (C). Ultrasound study was performed by Professor Fikri Abu-Zidan, Department of Surgery, Al-Ain Hospital, Al-Ain, UAE.
TECHNICAL CONSIDERATIONS
High frequency linear probes (10-12 MHz) have high resolution and low depth of penetration. Accordingly, they are used for diagnosing fractures[10,11]. It will be easy to perform POCUS on long bones using the linear probe because it gets in direct contact over the long bone (Figure 1A). The patient is asked to point at the maximum point of pain. The finger of the examiner is gently passed over the area to define the suspected area of fracture. This may not be possible in children, geriatrics and unconscious patients. It is always advised to compare the injured region with the normal side especially in children. Starting with the normal side in children will assure them and avoid the pitfall of misdiagnosing ossification centers and epiphysis as fractures[11]. One of the major technical difficulties encountered when detecting fractures of small bones is the irregularity of the bone surface. Accordingly, air may be present between the probe and the bone. Air gives very highly echogenic reflections (white) and can cause a barrier when performing ultrasound. Adequate gel should be applied between the ultrasound probe and skin to reduce the artifacts caused by air (Figure 4). Some may even use water bath as an ultrasound transmitter to reduce the air artifact and pain while examining the patient[11]. Ultrasound is not recommended to be done on open fractures. The diagnosis is already clinically made; this will delay the management, may cause infection, and will be very painful.
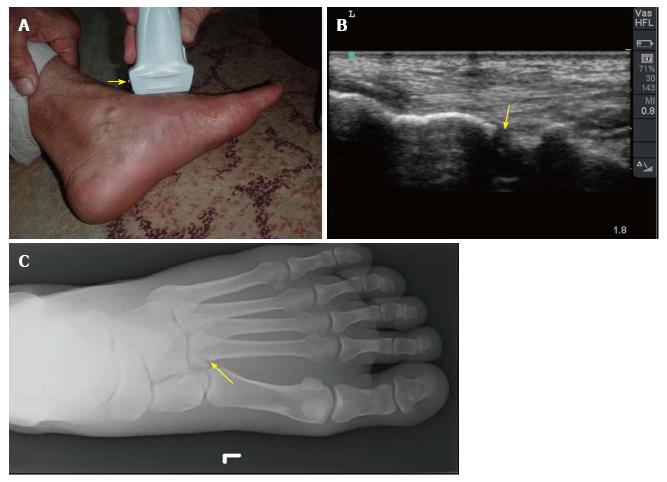
Figure 4 Point-of-care ultrasound of a 60-year-old man who twisted his left ankle and could not walk on it.
He had swelling of the left foot with maximum tenderness on the base of second metatarsal bone (A). The yellow arrow indicates the marker of linear probe which is shown on the left side of the screen while the groove on the other side is shown on the right side of the screen. B mode images of the previous patient showed a cortical defect (yellow arrow) at the base of the second metatarsal bone suggestive of a fracture (B). Plain X-ray of the foot confirmed these findings (C). Ultrasound study was performed by Professor Fikri Abu-Zidan, Department of Surgery, Al-Ain Hospital, Al-Ain, UAE.
ULTRASOUND IN MCIS
The benefits of using POCUS in MCIs are numerous. Multiple injured patients may need help in austere geographical locations where radiological investigations are not available. POCUS is of great value in these circumstances. Hand-held ultrasound units have been routinely used in hospital and pre-hospital settings as a normal practice with encouraging positive results[7,12,13]. This has increased the experience in using POCUS outside the routine hospital practice in conditions mimicking MCIs. Furthermore, POCUS has been done on patients during helicopter transportation in an unstable environment[14]. POCUS images were transmitted through satellite technology using the principles of telemedicine by evaluating images at distant centers[15]. Despite reduced clarity, overall accuracy in remotely detecting pericardial and peritoneal free fluid was 86%[15]. POCUS images have even been transmitted from the International Space Station to a remote-control center located on the earth yielding acceptable image quality to make clinical decisions[16,17]. Smartphones have been recently used in transmitting ultrasound images which is a very attractive approach in MCIs[18].
CLINICAL APPLICATIONS
ATLS have been advocated in many countries as the accepted guidelines in the management of multiply injured patients. This includes primary physiological survey (Airway, Breathing, Circulation, Disability, and Exposure) for treating life-threatening conditions. This is followed by secondary survey which includes examining the patient from head to toe, front and back. POCUS has been very useful in the primary survey to define the source of shock in multiply injured patients[19,20].
Diagnosing fractures by ultrasound should be part of the secondary survey. Certain protocols, like the CAVEAT protocol and FASTER protocol were developed to use portable ultrasound in the MCIs. They included extremity ultrasound examination in these protocols[4,5,21]. The CAVEAT protocol (Chest, Abdomen, Vena cava, and Extremities for Acute Triage) included ultrasound extremity examination as part of the triage during the secondary survey[4,5]. The FASTER protocol added the Extremity and Respiratory evaluation to the classical Focused Assessment Sonography for Trauma (FAST) examination[21]. Hand held ultrasound could properly diagnose long bone fractures in military conditions[22]. Dulchavsky et al[21] used portable machines with linear probes in 95 patients who had extremity injuries (158 extremity examinations). Ninety-four percent of these patients were accurately diagnosed. Ultrasound can diagnose occult fractures that can be missed by conventional X-rays because it is very sensitive to cortical defects[5,23] (Figure 4).
May and Grayson[24], in a Best Evidence Report published in 2009, critically appraised four papers. They reported that the results of using ultrasound to diagnose fractures of the wrist in children are very encouraging with high sensitivity reaching above 90%. Furthermore, they stressed the need for larger studies to prove their conclusions[24]. A systematic review and meta-analysis, which was published in 2013, showed that ultrasound was accurate in diagnosing extremity fractures. This study searched MEDLINE and EMBASE during the period of 1965 to 2012[25]. They included 8 studies in their final review. Six of these were in children. All studies used convenient, and not consecutive, samples. Ultrasound sensitivity for detecting extremity fractures ranged between 83% and 100%. The positive likelihood ratio ranged between 3.2 and 56.
An excellent recent systematic review and meta-analysis of high quality evaluated the diagnostic accuracy of ultrasound for distal forearm fractures[26]. The authors searched PubMed, EMBASE and Cochrane database and included 16 studies in their final meta-analysis. Almost all studies used convenient samples but their overall quality was average to high. Majority were in children. The pooled ultrasound sensitivity and specificity for detecting distal forearm fractures were 97% and 95% respectively. The positive likelihood ratio was 20. Nevertheless, the heterogeneity of the sensitivity and specificity of the studies was very high (82% and 87%) with a very significant p value from the chi-squared test (P < 0.0001).
POCUS TRAINING
The ultrasound guidelines for the American College of Emergency Physicians advocates the diagnosis of fractures by emergency physicians[11]. According to the CAVEAT protocol, extremity assessment by ultrasound is one of the most difficult skills to be achieved[4]. The results of ultrasound depend on three main factors: (1) training and experience of the operator; (2) quality of the machine; and (3) the studied region of the patient[27]. Operators’ experience in ultrasound varies tremendously which may dramatically affect its results[28,29]. This is important when defining the role of ultrasound in MCIs. In principle, POCUS training should be incorporated into the surgical and emergency physicians training. Ultrasound training should include understanding the basic physics, instrumentation and image interpretation[30,31]. Different methods have been used to achieve that including human models, patients, video clips, cadavers, simulation technology, and animal models[29,32-34].
PERSONAL VIEW
Although the discussed principles in this article look easy, I find it occasionally difficult to diagnose very minor fractures. The main reason is that it takes time to do a full screening especially for minor fractures in seriously injured patients. This is a limitation which has been acknowledged by others[6]. There is no doubt that POCUS is very useful to early diagnose fractures of long bone as they may cause shock. It is questionable whether diagnosing small bone fracture will have a long-term advantage on these patients.
Twenty-five years ago, no one would have imagined the place that POCUS will take in managing multiple trauma patients. The role of POCUS in MCIs in austere conditions is still evolving. Its potential is not yet fully defined. Its role in managing fractures will depend on different factors. The operator should master the technique, understand it limitations, and most importantly correlate the sonographic findings with the clinical ones. No doubt that portability, safety, repeatability, and cost-effectiveness of ultrasound are great advantages when treating multiply injured patients in MCIs. The technology is there but it is our duty to define its real value.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Arab Emirates
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hefny AF, Shahab F S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ