Published online Jul 18, 2017. doi: 10.5312/wjo.v8.i7.553
Peer-review started: February 12, 2017
First decision: April 18, 2017
Revised: May 15, 2017
Accepted: May 30, 2017
Article in press: May 31, 2017
Published online: July 18, 2017
To evaluate the clinical and X-ray results of acetabular components and tantalum augments in prosthetic hip revisions.
Fifty-eight hip prostheses with primary failure of the acetabular component were reviewed with tantalum implants. The clinical records and X-rays of these cases were retrospectively reviewed. Bone defect evaluations were based on preoperative CT scans and classified according to Paprosky criteria of Radiolucent lines and periprosthetic gaps; implant mobilization and osteolysis were evaluated by X-ray. An ad hoc database was created and statistical analyses were performed with SPSS software (IBM SPSS Statistics for Windows, version 23.0). Statistical analyses were carried out using the Student’s t test for independent and paired samples. A P value of < 0.05 was considered statistically significant and cumulative survival was calculated by the Kaplan-Meier method.
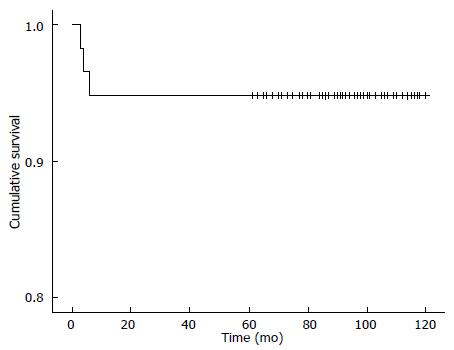
The mean follow-up was 87.6 ± 25.6 mo (range 3-120 mo). 25 cases (43.1%) were classified as minor defects, and 33 cases (56.9%) as major defects. The preoperative HHS rating improved significantly from a mean of 40.7 ± 6.1 (range: 29-53) before revision, to a mean of 85.8 ± 6.1 (range: 70-94) at the end of the follow-up (Student’s t test for paired samples: P < 0.001). Considering HHS only at the end of follow-up, no statistically significant difference was observed between patients with a major or minor defect (Student’s t test for independent samples: P > 0.05). Radiolucent lines were found in 4 implants (6.9%). Postoperative acetabular gaps were observed in 5 hips (8.6%). No signs of implant mobilization or areas of periprosthetic osteolysis were found in the x-rays at the final follow-up. Only 3 implants failed: 1 case of infection and 2 cases of instability. Defined as the end-point, cumulative survival at 10 years was 95% (for all reasons) and 100% for aseptic loosening of the acetabular component.
The medium-term use of prosthetic tantalum components in prosthetic hip revisions is safe and effective in a wide variety of acetabular bone defects.
Core tip: Revisions of acetabular implant components are frequently associated with bone defects. Porous tantalum acetabular cups and augments were introduced to improve biological fixing and restore the normal centre of rotation. The greatest advantage is for major bone defects, where the tantalum cup and augments provide stable primary fixing with the biological potential for bone ingrowth. Nowadays, porous tantalum represents the ideal bone substitute in prosthetic revisions.
- Citation: Evola FR, Costarella L, Evola G, Barchitta M, Agodi A, Sessa G. Acetabular revisions using porous tantalum components: A retrospective study with 5-10 years follow-up. World J Orthop 2017; 8(7): 553-560
- URL: https://www.wjgnet.com/2218-5836/full/v8/i7/553.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i7.553
The revision of the acetabular component of a prosthetic implant is frequently associated with a bone defect. Different types of treatment and its complications are described in the literature: The use of structural allograft from cadaver or synthetic bone substitutes with anti-protrusio rings or reconstruction cages do not fix biologically and are at high risk of medium-term failure (15%-45% within 10 years)[1-7]. The use of morcellised bone grafts (impaction grafting) with cemented acetabular inserts can cause fractures, resorption with implant migration, and transmission of infectious diseases[8,9]. Implanting bilobed oblong cups or extra-large uncemented hemispherical so-called “jumbo cups” can destroy the rear column because the upper and lower bone defects are larger than the front and back ones[10,11]. High hip centres alter joint bio-mechanics and are associated with greater risks of dislocation and mobilization[12,13]. Cementless fixing in primary and revision implants has demonstrated greater survival in the medium and long-term compared to cemented fixing[13-15].
Biological bone integration of the implant requires intimate contact between the components and bone and immediate mechanical stability during the operation; often the surgeon is forced to implant the acetabular component high up in the revisions leading to altered abductor muscle function and heterometry of the limbs[16]. In the last decade porous tantalum-made acetabular cups and augments have been introduced to improve biological fixing in bone defects and allow the normal centre of rotation to be restored[13,17].
Tantalum is a ductile metal, inert and bio-compatible in vivo. Porous tantalum, produced through a process of chemical deposition of the metal in a reticulated skeleton in glassy carbon, is 80% porous, has an average pore size of 550 microns, an elastic modulus of 3.1 Gigapascals (Gpa) and a friction coefficient of 0.88 to form a structure very similar to cancellous bone[17]. Due to its three-dimensional structure and bioactivity, porous tantalum has shown complete bone integration in animal models in 4-6 wk from implantation[18]. Furthermore, compared to titanium implants, it can fill up periprosthetic gaps of up to 5 mm[17,18]. Therefore the use of tantalum components represents a viable alternative to traditional surgical techniques, especially in the presence of large bone defects, because the implant can achieve immediate stability. There are only a few studies in the literature with small samples of tantalum components in hip revisions, the majority of these studies being short term.
The aim of this study is to evaluate the clinical and radiographic results of acetabular components and tantalum augments in prosthetic hip revisions, and assess whether bone defect types can compromise outcomes or the medium term survival of the implants.
From December 2006 to December 2011, 58 hip prostheses with primary failure of the acetabular component were reviewed with implants in tantalum. A retrospective review of the clinical records and X-rays of these cases was performed. Patients underwent clinical and radiographic evaluation before and after the review procedure at regular intervals. Clinical evaluation was performed pre-operatively and at the end of the follow-up, using the Harris Hip Score (HHS): A score of 91 to 100 was considered as “excellent”, 81 to 90 as “good”, 71 to 80 as “fair”, and below 70 as “poor”.
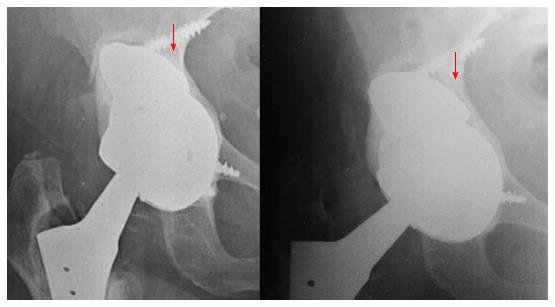
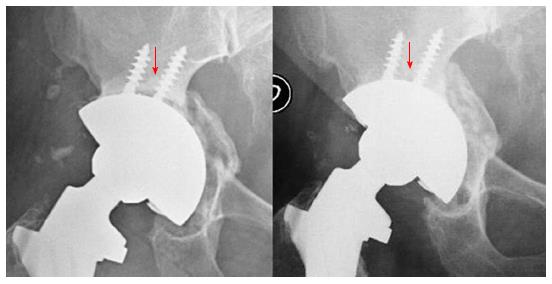
Radiographic evaluation was performed with axial and front-rear views of the pelvis; X-rays were evaluated by two independent orthopedists (GL and SB) who did not take part in this project. Radio-lucent lines, periprosthetic gaps, implant mobilization and osteolysis were evaluated radiographically. Radio-lucent lines of the acetabular components and augments were described according to the DeLee et al[19] criteria and measured through a transparent ruler; radio-lucent lines are considered significant if > 2 mm or progressive (Figure 1). Acetabular gaps were defined as areas in which the prosthesis surface did not achieve direct initial contact with the bone in early postoperative X-rays. The gaps differentiate from radio-lucent lines appearing on subsequent X-rays and are measured through a transparent ruler; acetabular gaps were considered positive when > 1 mm on the initial postoperative X-ray (Figure 2). Implant mobilization is defined by angle inclinations over 8° compared to post-operative X-ray checks or the presence of radiolucent lines in all three DeLee and Charnley zones[20,21]. X-ray evidence of stable implant fixing was shown by prosthesis contact with the bone and no radiolucent lines in 2 of the 3 zones. Osteolysis is the presence of a > 4 mm lucent area (by X-ray) near the prosthesis[22].
The evaluation of bone defects was based on preoperative CT scans and classified by Paprosky criteria[23]. Type 1: Limited bone defect, with unaltered rhyme, wall and columns; type 2 (A, B, C): Unaltered columns, but with deformed rhyme and walls; type 3 (A and B): Destroyed posterior column.
According to Watson-Jones, an anterolateral approach has been used in all procedures, regardless of the type of surgery previously performed. Twenty-eight (48.3%) uncemented press-fit Trabecular Metal Monoblock Acetabular Cups (Zimmer®) and thirty (51.7%) Trabecular Metal Revision Shells (Zimmer®) were implanted. The decision to use adjunctive screw fixes in uncemented Monoblock cups was taken intraoperatively. For complex acetabular revisions, Revision Shells offer the most versatile option, because the polyethylene liner is cemented inside the cup with adjustable inclination and anteversion; furthermore, the non-modular component offers advantages over the modular component having a lower modulus of elasticity and better screw fixing and positioning directly through the tantalum shell.
The tantalum augments, of different shapes and sizes, with rim screw holes, are used to restore the center of rotation and the normal bio-mechanics of the hip, fill large bone defects (> 50%) and restore the acetabular support margins, to allow greater prosthesis-bone contact and better mechanical stability[16,18,22].
The decision to use augments was based on bone defect and intraoperative prosthetic stability. Augments are screw-fixed into the acetabulum and separated from the prosthesis with a thin layer of polymethylmethacrylate; they also reduce the use of morcellised bone or structural cadaver bone and are resistant to fractures, mobilization, and resorption, which, however, can affect massive grafts as a result of vascular integration and periprosthetic bone remodelling[24]. Augments were used in 16 cases: 3 type 2C, 8 type 3A, 5 in type 3B. Autologous morcellised bone from acetabular reamers, or homologous from the frozen head of the femur, was inserted between the implant and the remaining bone defect and has been used in 38 revision procedures of (29 major and 3 minor). Structural bone grafts, synthetic bones nor demineralized bone matrices were not used.
Experienced prosthetic hip surgeons performed the revisions. After surgery, an abduction brace was applied for two days after surgery and partial load with crutches for at least thirty days was recommended. A specific rehabilitation program was used to prevent mobilization or early dislocation of the implant. Data was ere analyzed anonymously and results were reported in an aggregate manner.
All the data was made into an ad hoc database and statistical analyses were performed using the SPSS software (IBM SPSS Statistics for Windows, version 23.0). Descriptive statistics were used to characterize the population using frequencies and means ± SD. Statistical analyses of HHS were carried out using the Student’s t test for independent and paired samples. A P value of < 0.05 was considered statistically significant. A standard life table was constructed, and cumulative survival was calculated by means of the Kaplan-Meier method, using all causes and infections of the acetabular component as end-points.
Statistical analyses were performed by two Authors (Antonella Agodi and Martina Barchitta) using the SPSS software (IBM SPSS Statistics for Windows, version 23.0).
During the study period, a total of 58 acetabular revisions were performed and reviewed. The main patient and procedure characteristics are reported in Table 1. There were 31 women (53.4%) and 27 men (46.6%) with a mean age of 71.9 years (range: 42-82 years) at the time of revision. The most frequent indicator for revision was aseptic loosening of the implant (84.5%).
| Characteristic | |
| Age, mean ± SD, yr | 71.9 ± 5.5 |
| Gender | |
| Male | 27 (46.6) |
| Female | 31 (53.4) |
| Revision motive | |
| Aseptic loosening | 49 (84.5) |
| Polyethylene wear | 7 (12.1) |
| Infection | 2 (3.4) |
| Paprosky’s classification | |
| Type 2A | 11 (19.0) |
| Type 2B | 14 (24.1) |
| Type 2C | 13 (22.4) |
| Type 3A | 15 (25.9) |
| Type 3B | 5 (8.6) |
| Augment usage among 2C, 3A and 3B | 16 (48.5) |
| Average follow-up, mo, (± SD; range) | 87.6 (± 25.6; range 3-120) |
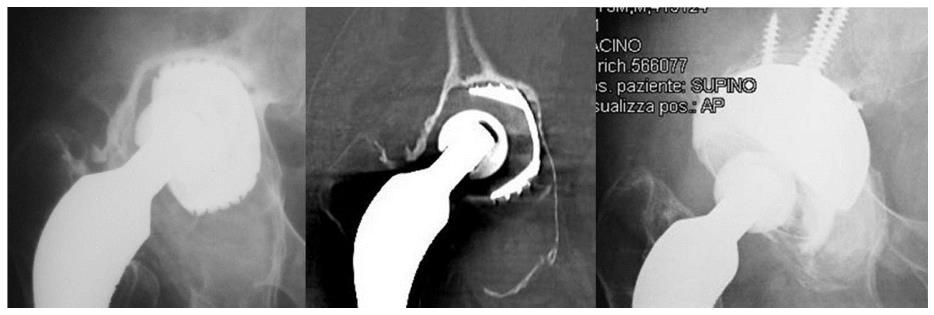
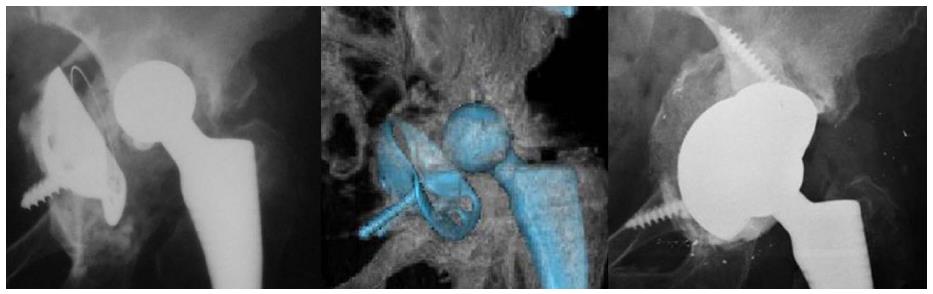
According to Paprosky’s classification, 11 hips (19.0%) were type 2A, 14 (24.1%) were type 2B, 13 (22.4%) were type 2C, 15 (25.9%) were type 3A and 5 (8.6%) were type 3B. Thus, a total of 25 cases (43.1%) were classified as minor defects (types 2A and 2B) (Figure 3) and 33 cases (56.9%) as major defects (types 2C, 3A and 3B) (Figure 4).
The mean follow-up was 87.6 ± 25.6 mo (range 3-120 mo).The preoperative HHS rating improved significantly from a mean of 40.7 ± 6.1 (range: 29-53) before revision, to a mean of 85.8 ± 6.1 (range: 70-94) at the end of the follow-up (Student’s t-test for paired samples: P < 0.001), with 75.6% of patients in the “excellent” or “good” categories.
Considering only the HHS at the end of the follow-up, no statistically significant difference was observed between patients with a major defect (types 2C, 3A and 3B, mean HHS 86.3 ± 4.9) and patients with a minor defect (types 2A and 2B, mean HHS 85.3 ± 7.5) (Student’s t test for independent samples: P > 0.05). HHS ratings of patients with implant failure were not included in these analyses.
Radiolucent lines were found in 4 implants (6.9%): In 3 implants the lines were not more than 2 mm or progressive and involved only one of the three DeLee and Charnley areas, while in 1 implant, which was revised because of infection, they were progressive. Therefore all implants, except the one revised for an infection, were X-ray defined as stable. The excellent osteoconductive properties of tantalum enabled rapid strong biological fixing, even where there was limited vital bone, especially in major defects.
Postoperative acetabular gaps were observed in 5 hips (8.6%) all of which disappeared during the initial 12 mo after surgery and thus were not found at the final follow-up.
No signs of implant mobilization or areas of periprosthetic osteolysis were found in the X-rays at the final follow-up. Morcellised bone grafts with augments to fill bone defects showed no signs of resorption in regular X-ray controls. Only 3 implants failed: 1 case of infection (6 mo after surgery) (Figure 5) and 2 cases of instability (3 and to 4 mo after surgery). The first patient with instability was treated with dislocation reduction and a tutor for 30 d; the second patient with instability required revision surgery implant a constrained liner for chronic instability. In the patient with infection, because of poor general condition and limited functional requirements, the implant was removed and treated with Girdlestone resection arthroplasty. Minor complications were: 2 cases of deep vein thrombosis treated with heparin, 1 case of superficial infection treated with surgical revision of the wound, 1 case of neuro apraxia of the sciatic nerve resolved spontaneously after 2 mo from surgery. None of the patients underwent revision for aseptic loosening until the final follow-up.
Defined as the end-point, cumulative survival at 10 years was 95% (for all reasons) and 100% for aseptic loosening of the acetabular component (Figure 6).
Treatment of a failed acetabular component in total hip prosthesis is technically demanding because immediate and long term stability of the implant is required, as well as maintaining or increasing bone stock, restoring the centre of rotation, and preventing limb discrepancy.
Traditional hemispherical cups (titanium alloy and cobalt chromium alloy) are an effective solution in revisions where adequate bone stock (> 50%) is available to support the acetabular component and allow for bone ingrowth[16,17,22,25,26]. In cases where the biological potential and mechanical stability of the prosthetic implant are compromised by bone deficit (< 50% acetabular bone available to support the acetabular component), alternative treatments should be used[7,27].
Porous tantalum implants have been used since 1997 and provide excellent initial stability and bone ingrowth. The higher porosity (80%) promotes better growth of vascularized bone inside the prosthesis (microfixing) in comparison to common porous surfaces; the high coefficient of friction to the cancellous (0.88) and cortical (0.74) bone ensures greater primary stability (macrofixing); the low modulus of elasticity (3.1 GPa) brings the material closer to the trabecular bone (1.5 GPa) compared to titanium (110 GPa) and cobalt-chromium (220 GPa), allowing greater load-induced bone remodelling and minimized stress shielding near the cup[17]. The three-dimensional structure and excellent osteoconductive properties of porous tantalum provide faster and stronger biological fixing when there is limited vital bone availability, and facilitate the restoration of the bone stock[28].
The ingrowth properties of porous tantalum are superior to bone graft in revision surgery; allograft reabsorption can lead to component instability, while porous tantalum maintains its structure and stability[26]. A stable bone-implant interface and favourable osteoconductive properties of the material are important for bone ingrowth of prostheses. Furthermore, the availability of augments in tantalum has reduced the need for structural bone grafts in revisions and safer recovery of the hip rotation centre.
Clinical evaluation at the final follow-up showed a statistically significant increase in preoperative HHS from 40.7 to 85.8. In this study we did not find a statistically significant association between bone defect size and increased clinical results at final follow-up, demonstrating that the clinical results of acetabular revisions with tantalum components do not seem to be influenced by the degree of preoperative bone defect. However, other authors have shown that clinical outcomes are influenced by bone defects when using traditional techniques, such as structural bone grafting and reconstruction cages[18,29].
X-rays revealed no prosthetic implant migration. Some non-progressive radiolucent lines in three implants were probably due to some fibrous fixing in part of the implant, and requires X-ray monitoring in the future.
Several authors report instability as the main cause of failure of tantalum implants[1,16]. In this study the survival of the implants for 10 years was 95%, considering the revision for any reason as end-point. Of the three reported failures, two were for implant dislocation. Only one failure showed incorrect positioning of the socket.
High numbers of dislocations in the literature suggest that special attention should be addressed to correcting the centre of rotation and implant positioning, and to using constrained implants in cases of deficient abductor mechanisms.
This study has several limitations: (1) it is a retrospective study with a limited sample size, heterogeneous patient ages and a variety of bone defects; (2) restoring the normal rotation centre of the implant was not monitored by X-ray (calculating the vertical and horizontal distance from the inter-teardrop line); (3) the study did not consider the size of the acetabular component and femoral head diameter according to preoperative bone defect; and (4) this study has not control group for comparison. A future multi-centre study including homogeneous samples by age and bone defect would be useful in assessing the medium and long-term clinical and X-ray results of tantalum implants in prosthetic hip revisions.
In conclusion, the medium-term use of prosthetic tantalum components in prosthetic hip revisions is safe and effective in a wide variety of acetabular bone defects. The greatest advantage is found in major bone defects, where the tantalum cup and augments provide stable primary fixation with the biological potential for bone ingrowth. Despite these advantages, the metallic debris effects of this material are still unknown. Long-term studies are needed to evaluate the longevity of these implants and demonstrate their advantages over conventional methods such as massive grafting and reconstruction cages. Nowadays, porous tantalum represents the ideal bone substitute in prosthetic revisions.
This study evaluates the results of acetabular components and tantalum augments in prosthetic hip revisions, assessing whether the type of bone defect can compromise the outcome or the medium-term survival of the implants. In this study the authors did not find a statistically significant association between the size of the bone defect and increased clinical results. Defined as the end-point, cumulative survival at 10 years was 95% (for all reasons) and 100% for aseptic loosening of the acetabular component.
Treating the failure of the acetabular component in total hip prosthesis is technically demanding because of significant bone defect. Nowadays, studies are being directed towards searching for a material which possesses bone-like biomechanical characteristics. Porous tantalum implants provide excellent initial stability, bone ingrowth and allow for greater load-induced bone remodelling near the cup.
There are few studies on hip reviews with tantalum components in the literature where the samples are small, have non-homogeneous bone defect severity and short term follow-ups. This study evaluates the medium-term clinical and X-ray results of tantalum components in acetabular revisions with major bone defects.
The use of prosthetic tantalum components in prosthetic hip revisions is safe and effective for large acetabular bone defects. Nowadays, porous tantalum represents the ideal bone substitute in prosthetic revisions and provides excellent mechanical stability of the implants.
Tantalum is a ductile metal, inert and bio-compatible in vivo. Due to its three-dimensional structure and bioactivity, porous tantalum has a structure very similar to cancellous bone.
This is an interesting manuscript dealing with a popular field of revision hip arthroplasty.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Li JM, Recnik G S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Issack PS. Use of porous tantalum for acetabular reconstruction in revision hip arthroplasty. J Bone Joint Surg Am. 2013;95:1981-1987. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Bostrom MP, Lehman AP, Buly RL, Lyman S, Nestor BJ. Acetabular revision with the Contour antiprotrusio cage: 2- to 5-year followup. Clin Orthop Relat Res. 2006;453:188-194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Beckmann NA, Weiss S, Klotz MC, Gondan M, Jaeger S, Bitsch RG. Loosening after acetabular revision: comparison of trabecular metal and reinforcement rings. A systematic review. J Arthroplasty. 2014;29:229-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Brüggemann A, Fredlund E, Mallmin H, Hailer NP. Are porous tantalum cups superior to conventional reinforcement rings? Acta Orthop. 2017;88:35-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Sessa G, Costarella L, Pavone V, Graceffa A, Evola G, Evola FR. Equine bone tissue in acetabular revision: our experience. Minerva Ortopedica e Traumatologica. 2010;61:469-476. [Cited in This Article: ] |
| 6. | Flecher X, Paprosky W, Grillo JC, Aubaniac JM, Argenson JN. Do tantalum components provide adequate primary fixation in all acetabular revisions? Orthop Traumatol Surg Res. 2010;96:235-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Van Kleunen JP, Lee GC, Lementowski PW, Nelson CL, Garino JP. Acetabular revisions using trabecular metal cups and augments. J Arthroplasty. 2009;24:64-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Busch VJ, Gardeniers JW, Verdonschot N, Slooff TJ, Schreurs BW. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old: a concise follow-up, at twenty to twenty-eight years, of a previous report. J Bone Joint Surg Am. 2011;93:367-371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | van Egmond N, De Kam DC, Gardeniers JW, Schreurs BW. Revisions of extensive acetabular defects with impaction grafting and a cement cup. Clin Orthop Relat Res. 2011;469:562-573. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Hendricks KJ, Harris WH. Revision of failed acetabular components with use of so-called jumbo noncemented components. A concise follow-up of a previous report. J Bone Joint Surg Am. 2006;88:559-563. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Dearborn JT, Harris WH. Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow-up study. J Arthroplasty. 2000;15:8-15. [PubMed] [Cited in This Article: ] |
| 12. | Dearborn JT, Harris WH. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty. Results after a mean of ten years. J Bone Joint Surg Am. 1999;81:469-480. [PubMed] [Cited in This Article: ] |
| 13. | Flecher X, Appy B, Parratte S, Ollivier M, Argenson JN. Use of porous tantalum components in Paprosky two and three acetabular revision. A minimum five-year follow-up of fifty one hips. Int Orthop. 2017;41:911-916. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Whitehouse MR, Masri BA, Duncan CP, Garbuz DS. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin Orthop Relat Res. 2015;473:521-527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Evola FR, Evola G, Graceffa A, Sessa A, Pavone V, Costarella L, Sessa G, Avondo S. Performance of the CLS Spotorno uncemented stem in the third decade after implantation. Bone Joint J. 2014;96-B:455-461. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA. Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop. 2014;38:689-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Batuyong ED, Brock HS, Thiruvengadam N, Maloney WJ, Goodman SB, Huddleston JI. Outcome of porous tantalum acetabular components for Paprosky type 3 and 4 acetabular defects. J Arthroplasty. 2014;29:1318-1322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Fernández-Fairen M, Murcia A, Blanco A, Meroño A, Murcia A, Ballester J. Revision of failed total hip arthroplasty acetabular cups to porous tantalum components: a 5-year follow-up study. J Arthroplasty. 2010;25:865-872. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;20-32. [PubMed] [Cited in This Article: ] |
| 20. | Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration. An experimental study. J Arthroplasty. 1989;4:245-251. [PubMed] [Cited in This Article: ] |
| 21. | Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995;77:432-439. [PubMed] [Cited in This Article: ] |
| 22. | Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22:151-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 23. | Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33-44. [PubMed] [Cited in This Article: ] |
| 24. | Macheras GA, Papagelopoulos PJ, Kateros K, Kostakos AT, Baltas D, Karachalios TS. Radiological evaluation of the metal-bone interface of a porous tantalum monoblock acetabular component. J Bone Joint Surg Br. 2006;88:304-309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 25. | Del Gaizo DJ, Kancherla V, Sporer SM, Paprosky WG. Tantalum augments for Paprosky IIIA defects remain stable at midterm followup. Clin Orthop Relat Res. 2012;470:395-401. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 26. | Moličnik A, Hanc M, Rečnik G, Krajnc Z, Rupreht M, Fokter SK. Porous tantalum shells and augments for acetabular cup revisions. Eur J Orthop Surg Traumatol. 2014;24:911-917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Davies JH, Laflamme GY, Delisle J, Fernandes J. Trabecular metal used for major bone loss in acetabular hip revision. J Arthroplasty. 2011;26:1245-1250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Lachiewicz PF, Soileau ES. Tantalum components in difficult acetabular revisions. Clin Orthop Relat Res. 2010;468:454-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 29. | Skyttä ET, Eskelinen A, Paavolainen PO, Remes VM. Early results of 827 trabecular metal revision shells in acetabular revision. J Arthroplasty. 2011;26:342-345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |