Published online Nov 18, 2017. doi: 10.5312/wjo.v8.i11.846
Peer-review started: February 2, 2017
First decision: June 26, 2017
Revised: July 10, 2017
Accepted: September 3, 2017
Article in press: September 4, 2017
Published online: November 18, 2017
To compared outcomes between the hypothenar fat pad flap (HTFPF) and conventional open carpal tunnel release (COR) in primary carpal tunnel syndrome (CTS).
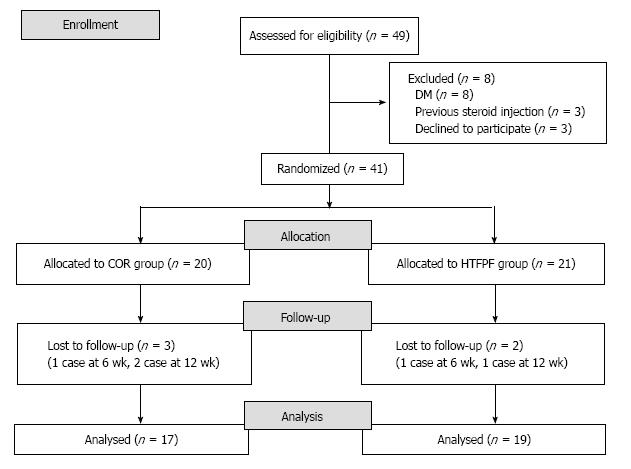
Forty-five patients (49 hands) were enrolled into the study from January 2014 to March 2016, 8 patients were excluded. Randomization was conducted in 37 patients (41 hands) by computer generated (Block of four randomization) into COR and HTFPF group. Nerve conduction study (NCS) included distal sensory latency (DSL), distal motor latency (DML), sensory amplitude (S-amp), motor amplitude (M-amp) and sensory nerve conduction velocity (SCV) were examined at 6 and 12 wk after CTR. Levine score, grip and pinch strength, pain [visual analog scale (VAS)], 2-point discrimination (2-PD), Semmes-Weinstein monofilament test (SWM), Phalen test and Tinel’s sign were evaluated in order to compare treatment outcomes.
The COR group, 19 patients (20 hands) mean age 50.4 years. The HTFPF group, 20 patients (21 hands) mean age 53.3 years. Finally 33 patients (36 hands) were analysed, 5 patients were loss follow-up, 17 hands in COR and 19 hands in HTFPF group. NCS revealed significant difference of DSL in HTFPF group at 6 wk (P < 0.05) compared with the COR group. S-amp was significant improved postoperatively in both groups (P < 0.05) but not significant difference between two groups. No significant difference of DML, M-amp and SCV postoperatively in both groups and between two groups. Levine score, pain (VAS), grip and pinch strength, 2-PD, SWM, Phalen test and Tinel’s sign were improved postoperatively in both groups, but there was no significant difference between two groups.
There is no advantage outcome in primary CTS for having additional HTFPF procedure in CTR. COR is still the standard treatment. Nevertheless, improvement of DSL and S-amp could be observed at 6 wk postoperatively.
Core tip: The study conducted a randomized controlled trial to compare between the hypothenar fat pad flap additional and conventional open carpal tunnel release in primary carpal tunnel syndrome. The study showed no advantage, however improvement of nerve conduction study was observed in the early postoperatively.
- Citation: Kanchanathepsak T, Wairojanakul W, Phakdepiboon T, Suppaphol S, Watcharananan I, Tawonsawatruk T. Hypothenar fat pad flap vs conventional open release in primary carpal tunnel syndrome: A randomized controlled trial. World J Orthop 2017; 8(11): 846-852
- URL: https://www.wjgnet.com/2218-5836/full/v8/i11/846.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i11.846
Carpal tunnel syndrome (CTS) is the most common compression neuropathy in the upper extremity[1]. The worldwide incidence is 5.8% in women and 0.6% in men[2], while the pathology and the causes are unclear. Several studies describe that the symptoms caused by direct nerve compression and nerve ischemia[3,4].
Fullerton[4] found that the numbness symptom of CTS may arise from the nerve ischemia. The median nerve ischemia alters axonal threshold and significantly increases both sensory and motor refractoriness resulting numbness and paresthesia in CTS patients[3]. Furthermore, the nerve ischemia may cause by venous return obstruction dued to external pressure that increases pressure in the region of entrapment, leading to nerve edema and eventually resulting in nerve damage and fibrous tissue[5,6] and also can be provoked by ganglia, neoplastic masses, vascular abnormalities, ligamentous attachments, and also different various structures (anomalous muscles, bifid median nerve, persistent median artery)[7].
Carpal tunnel release (CTR) is a standard treatment for patients who indicated to surgery of CTS and the success rate was 75%-98%. However, several studies[8] found that some patients who had persist or recurrent compressive symptoms after this surgery was as high as 2%-25%. Nancollas et al[9], a retrospective review of 60 cases with an average of 5.5 years follow-up, had reported 57% recurrent symptoms within 2 years after surgery.
The hypothenar fat pad flap (HTFPF) procedure, first described by Cramer and refined by Strickland et al[10] is usually utilized in recurrent CTS, there is a adipose tissue from hypothenar eminence as a pedicle flap to cover the median nerve that provides vascularity, enhance nerve gliding property and prevent adhesion to the median nerve. This procedure had an excellent result and low rate of complication[8,10,12]. We hypothesized that increasing vascularity to the median nerve by HTFPF procedure could improve the nerve recovery and the success rate of CTR in primary CTS compared to the conventional CTR alone.
Forty-five patients (49 hands) who diagnosed with primary carpal tunnel syndrome were enrolled into the study during January 2014 and March 2016 while 8 of them were excluded from the study. Thirty-seven patients (41 hands) were conducted in this prospective randomized controlled trial study according to consort diagram (Figure 1). The study was approved by the local institutional review board and all patients signed an informed consent.
The inclusion criteria were primary idiopathic carpal tunnel syndrome, age 20-60 years, duration of symptoms at least 3 mo and no improvement of symptoms after conservative treatment. The exclusion criteria were previous CTR or trauma in affected hand, history of steroid injection, cerebrovascular disease, cervical radiculopathy, combined other nerve compression, diabetes mellitus, cognitive impairment and unwilling to participate.
Patients were randomized into either conventional open carpal tunnel release group (COR) or HTFPF group by using a computer generated table, STATA 12.0, Statacorp, college station, TX, United States (Block of four randomization) and concealed with sealed envelopes which were opened during the operation after transverse carpal ligament was released. All of the patients and assessors in this study were blinded after the interventions assignment.
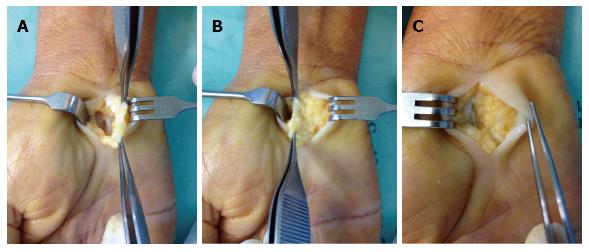
The only one senior hand surgeon performed CTR throughout the study. All patients were injected with 1% lidocaine without adrenaline for local anesthesia. A tourniquet was inflated 250 mmHg. Longitudinal skin incision was made from distal to the distal wrist flexion crease and 5 mm ulnar to thenar crease along the Kaplan’s line about 3 cm in length. Subcutaneous tissue and palmar fascia were dissected and retracted by Ragnel retractors. The transverse carpal ligament (TCL) was exposed and released by Stevens tenotomy scissors until clearly identified the median nerve (Figure 2A).
The concealed envelopes were opened to allocate the group of patients. In COR group, normal saline was irrigated and skin sutured with nylon no 5-0. In HTFPF group, superficial dissection at hypothenar fat was performed deep to palmaris brevis muscle and care should be taken to avoid digital nerve injury of ring and small fingers. The hypothenar fat pad with its vascular from ulnar artery was harvested (Figure 2B) then sutured HTFPF to radial half of TCL remnant with absorbable suture material for coverage over the median nerve (Figure 2C). Normal saline was irrigated and skin was sutured with nylon no 5-0. Wound dressing was applied in both groups.
All of patients were followed up 6 and 12 wk after surgery and nerve conduction study (NCS), physical examination, pain [visual analog scale (VAS)], symptom severity scale and functional status scale (Boston questionnaire) were recorded at each visit. Sutured was removed 2 wk after surgery in all patients.
The primary outcome was NCS including distal sensory latency (DSL), sensory amplitude (S-amp), distal motor latency (DML), motor amplitude (M-amp) and sensory conduction velocity (SCV). Self-administered questionnaire described by Levine et al[13], which also known as Boston questionnaire was used to evaluate the hand function. Boston questionnaire consists of symptom severity scale (SSS) which includes 11 questions which each answer score from 1 (best) to 5 (worst), making a total score of 55 and functional status scale (FSS) which includes 8 questions which each answer score from 1 (best) to 5 (worst), making total score 40.
Age, gender, body mass index (BMI), onset of duration, side of operation and hand dominant were collected. Pain (visual analog scale, VAS), Tinel’s sign, Phalen test, grip strength, pinch strength, 2-point discrimination (2-PD), Semmes-Weinstein monofilament test (SWM) and complication were evaluated in all patients.
NCS, pain (VAS), Levine score and all examination were compared between two groups at preoperatively, and 6 and 12 wk postoperatively. The NCS was performed as described in the previous literature[17] by the same physician.
The demographic data including age, gender, BMI, onset of duration, side of operation, hand dominant and examination (Tinel’s sign and Phalen test) were collected with excel version 2013. All of the continuous data were normally distributed and were presented with mean ± SD, while the categorical data were shown in percentage.
The primary and secondary outcomes were analyzed with the repeated ANOVA and Graphpad software version 6.0 and the relationship between groups and time to follow-up were evaluated. These data include NCS, Levine score, pain (VAS), 2-PD, grip strength, pinch strength and SWM. P < 0.05 was used to determine the correlation between two groups and time to follow-up postoperatively.
The COR group consists of 19 patients (20 hands, n = 20), all were female with the mean age of 50.4 years (41-62 years). The HTFPF group consists of 20 patients (21 hands, n = 21); 2 males (11%) and 16 females (89%) with the mean age of 53.3 years (42-63 years). Five patients were lost to follow-up; 3 cases in COR group and 2 cases in HTFPF group. Finally 33 patients (36 hands) were analysed in this study with 17 hands in COR group and 19 hands in HTFPF group. The demographic data of the included patients are summarized in Table 1.
| COR group (n = 17) | HTFPF group (n = 19) | P value | |
| Age (yr) mean ± SD | 50.4 (1.5) | 53.3 (1.5) | 0.182 |
| Gender (%) | 0.231 | ||
| Male | 0 (0) | 2 (11) | |
| Female | 17 (100) | 17 (89) | |
| Body mass index mean ± SD | 28.4 (1.3) | 25.5 (0.9) | 0.064 |
| Hand dominant (%) | 1 | ||
| Right | 15 (88) | 17 (90) | |
| Left | 2 (12) | 2 (10) | |
| Side of operation (%) | 0.017 | ||
| Right | 6 (35) | 15 (79) | |
| Left | 11 (65) | 4 (21) | |
| Onset of duration mo mean ± SD | 11.8 (2.3) | 13.3 (2.5) | 0.675 |
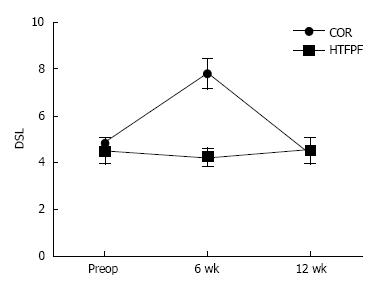
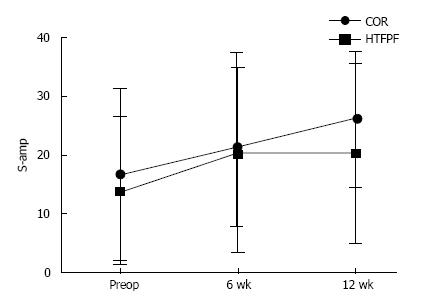
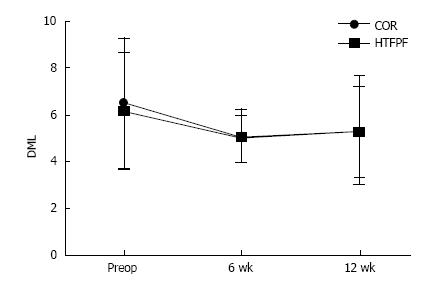
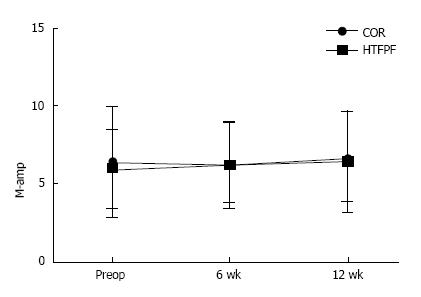
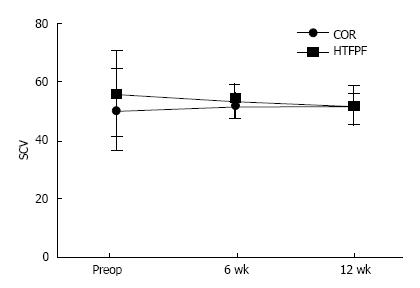
NCS revealed the improvement of DSL in HTFPF group at 6 and 12 wk postoperatively and statistically significant difference at 6 wk (P < 0.05) comparing with the COR group (Figure 3). S-amp was statistically significant improved postoperatively in both groups (P < 0.05) but not significantly different between two groups (Figure 4). There were no statistically significant differences of DML, M-amp and SCV between preoperative and postoperative in both groups and no statistically significant different of DML, M-amp and SCV between two groups (Figures 5-7).
Postoperative pain (VAS) was decreased in both groups but there was no significantly different between two groups. Negative result in both Tinel’s sign and Phalen test were detected in both groups postoperatively. Grip strength, pinch strength, 2-PD, SWM and Levine score were improved in both groups, however there was no statistical difference between two groups was shown (Tables 2-4).
| Levine score | Preop., mean ± SD | 6 wk postop., mean ± SD | 12 wk postop., mean ± SD | P value | |||
| COR | HTFPF | COR | HTFPF | COR | HTFPF | ||
| Symptom severity scale | 2.6 (0.6) | 2.5 (0.5) | 1.7 (0.5) | 1.7 (0.5) | 1.5 (2.5) | 1.1 (0.1) | > 0.05 |
| Functional status scale | 2.4 (1.0) | 2.5 (0.9) | 1.8 (0.7) | 1.7 (0.6) | 1.4 (0.6) | 1.1 (0.2) | > 0.05 |
| Preop., mean ± SD | 6 wk postop., mean ± SD | 12 wk postop., mean ± SD | P value | ||||
| COR | HTFPF | COR | HTFPF | COR | HTFPF | ||
| Grip strength (Pound) | 29.2 (15.0) | 28.9 (14.1) | 22.3 (12.8) | 21.4 (10.4) | 30.4 (13.0) | 31.4 (10.8) | > 0.05 |
| Pinch strength (Pound) | 12.0 (3.3) | 11.9 (3.9) | 11.0 (2.8) | 11.5 (3.4) | 13.3 (3.3) | 15.5 (3.0) | > 0.05 |
| Preop., mean ± SD | 6 wk postop, mean ± SD | 12 wk postop, mean ± SD | P value | ||||
| COR | HTFPF | COR | HTFPF | COR | HTFPF | ||
| Pain (VAS) | 4.6 (3.4) | 4.4 (3.4) | 0.4 (1.0) | 0.5 (1.1) | 0 (0) | 0 (0) | > 0.05 |
| 2-PD (mm) | 3.5 (1.0) | 4.7 (2.9) | 3.1 (0.8) | 2.9 (0.7) | 2.5 (0.5) | 2.7 (0.8) | > 0.05 |
| SWM | 3.7 (0.3) | 4.1 (1.0) | 3.4 (0.4) | 3.4 (0.5) | 3.3 (0.4) | 3.1 (0.4) | > 0.05 |
At 6 wk after operation, painful scar was occurred 11.76% and 31.58% in COR and HTFPF groups respectively, eventually the symptom was resolved in both groups at 12 wk and there were no statistically significant difference between two groups. Two of 19 cases in HTFPF group had pain over hypothenar eminence at 6 wk, however this symptom was disappeared at 12 wk.
The HTFPF is vascularized pedicle flap that supplied by branches of ulnar artery and widely used for recurrent or persistent CTS with median nerve hypersensitivity. Most authors reported an excellent result of HTFPF[8,10-12], even though had some modification by Craft et al[12] suggested the combination of microneurolysis of the median nerve and HTFPF.
It is limited evidence in the flap coverage procedure on the median nerve in primary CTS. Increasing vascularity to the median nerve may result in rapid nerve recovery and improve success rate. For that reason this study was conducted to add this procedure during CTR. This study used NCS for detection of nerve electrophysiology in short-term follow-up since there was no difference in the outcome of mid-term and long-term follow-up[9,14].
The advantage of HTFPF procedure are well-vascularized pedicle flap, could be harvested from same incision use of CTR with no donor site morbidity and sufficient to cover the median nerve in carpal tunnel[10,15].
The result of NCS revealed better nerve recovery in DSL in HTFPF group at 6 wk but not different at 12 wk compared to COR group. The S-amp was improved after surgery in both groups, however no significant difference between two groups was observed. There was no advantage outcomes of HTFPF procedure compared to COR in primary CTS. There were few studies performed the NCS in early postoperative, however this study shows an early detect of the electrophysiological conduction change in median nerve. This result was similar to study of Ginanneschi et al[14] reported at one month after CTR, SCV and DML were improved.
Conversely, El-Hajj et al[16] compared the DML and DSL, M-amp and S-amp, and SCV preoperatively and postoperatively, the result showed an improvement in all studied variables, except the DSL at 18 wk after surgery which improved only at 42 wk. The author explained that recovery of the sensory was delayed compare to motor, because the sensory fibers were affected more than motor fibers, and the myelin sheath more than the axons in most cases of CTS. Tahririan et al[17] study showed significant improvement in DSL, DML and SCV 6 mo postoperatively.
The strength of this study is the prospective randomized controlled trial, while small number of cases in each group is the limitation. Increased risk of painful scar and pain over the hypothenar eminence was found in HTFPF group. However, there was no statistical difference between two groups.
This study concluded that there was no advantage outcome in primary CTS for having additional HTFPF procedure in CTR compared with conventional technique. COR is still the standard treatment in primary CTS. Nevertheless, improvement of DSL and S-amp could be observed at 6 wk postoperatively. However, the interesting point is the recurrent rate in long-term follow-up between two groups and further data collection and analysis should be carried out in the future.
Carpal tunnel syndrome is the most common compression neuropathy. Carpal tunnel release is a standard treatment for patient who indicated for surgery although complete nerve recovery was not achieved for all of patients. This study hypothesized that increasing vascularity to the median nerve by hypothenar fat pad flap procedure could improve the nerve recovery of carpal tunnel release in primary carpal tunnel syndrome.
Many recent studies used flap coverage procedure on the median nerve for recurrent or persistent carpal tunnel syndrome.
There is no other studies have done the comparison between hypothenar fat pad flap and conventional carpal tunnel release in primary carpal tunnel syndrome before.
Although no advantage outcome in primary carpal tunnel syndrome for having additional hypothenar fat pad flap procedure in carpal tunnel release. However, improvement of distal sensory latency and sensory amplitude could be observed at 6 wk postoperatively.
Hypothenar fat pad flap is vascularized pedicle flap that supplied by branches of ulnar artery.
It is a well presented prospective randomized controlled trial comparing the hypothenar fat pad flap with conventional open techniques for carpal tunnel syndrome.
Manuscript source: Unsolicited Manuscript
Specialty type: Orthopedics
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Georgiev GPP, Lykissas MG, Mavrogenis AF S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
| 1. | Phalen GS. The carpal-tunnel syndrome. Clinical evaluation of 598 hands. Clin Orthop Relat Res. 1972;83:29-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 391] [Cited by in F6Publishing: 375] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1158] [Cited by in F6Publishing: 1128] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 3. | Han SE, Boland RA, Krishnan AV, Vucic S, Lin CS, Kiernan MC. Ischaemic sensitivity of axons in carpal tunnel syndrome. J Peripher Nerv Syst. 2009;14:190-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Fullerton PM. The effect of ischaemia on nerve conduction in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1963;26:385-397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 90] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Sunderland S. The nerve lesion in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1976;39:615-626. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 243] [Cited by in F6Publishing: 246] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Werner RA, Andary M. Carpal tunnel syndrome: pathophysiology and clinical neurophysiology. Clin Neurophysiol. 2002;113:1373-1381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 278] [Cited by in F6Publishing: 253] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 7. | Georgiev GP, Jelev L. Unusual coexistence of a variant abductor digiti minimi and reversed palmaris longus and their possible relation to median and ulnar nerves entrapment at the wrist. Rom J Morphol Embryol. 2009;50:725-727. [PubMed] [Cited in This Article: ] |
| 8. | Abzug JM, Jacoby SM, Osterman AL. Surgical options for recalcitrant carpal tunnel syndrome with perineural fibrosis. Hand (N Y). 2012;7:23-29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Nancollas MP, Peimer CA, Wheeler DR, Sherwin FS. Long-term results of carpal tunnel release. J Hand Surg Br. 1995;20:470-474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Strickland JW, Idler RS, Lourie GM, Plancher KD. The hypothenar fat pad flap for management of recalcitrant carpal tunnel syndrome. J Hand Surg Am. 1996;21:840-848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 117] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Mathoulin C, Bahm J, Roukoz S. Pedicled hypothenar fat flap for median nerve coverage in recalcitrant carpal tunnel syndrome. Hand Surg. 2000;5:33-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 60] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Craft RO, Duncan SF, Smith AA. Management of recurrent carpal tunnel syndrome with microneurolysis and the hypothenar fat pad flap. Hand (N Y). 2007;2:85-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, Katz JN. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75:1585-1592. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1271] [Cited by in F6Publishing: 1244] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 14. | Ginanneschi F, Milani P, Reale F, Rossi A. Short-term electrophysiological conduction change in median nerve fibres after carpal tunnel release. Clin Neurol Neurosurg. 2008;110:1025-1030. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Tollestrup T, Berg C, Netscher D. Management of distal traumatic median nerve painful neuromas and of recurrent carpal tunnel syndrome: hypothenar fat pad flap. J Hand Surg Am. 2010;35:1010-1014. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | El-Hajj T, Tohme R, Sawaya R. Changes in electrophysiological parameters after surgery for the carpal tunnel syndrome. J Clin Neurophysiol. 2010;27:224-226. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Tahririan MA, Moghtaderi A, Aran F. Changes in electrophysiological parameters after open carpal tunnel release. Adv Biomed Res. 2012;1:46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Delisa JA. Manual of nerve conduction velocity and clinical Neurophysiology. New York, USA: Raven Press; 1994; . [Cited in This Article: ] |