Published online Aug 18, 2016. doi: 10.5312/wjo.v7.i8.487
Peer-review started: February 27, 2016
First decision: March 24, 2016
Revised: May 19, 2016
Accepted: June 1, 2016
Article in press: June 3, 2016
Published online: August 18, 2016
AIM: To determine outcomes using the Femoro-Patella Vialla (FPV) arthroplasty and if there is an ideal patient for this implant.
METHODS: A total of 41 FPV patellofemoral joint replacements were performed in 31 patients (22 females, 9 males, mean age 65 years). Mean follow-up was 3.2 years (minimum 2 years). Radiographs were reviewed preoperatively and postoperatively. We assessed whether gender, age, previous surgery, patella atla or trochlear dysplasia influenced patient satisfaction or patient functional outcome.
RESULTS: The median Oxford Knee Score was 40 and the median Melbourne Patellofemoral Score was 21 postoperatively. Seventy-six percent of patients were satisfied, 10% unsure and 14% dissatisfied postoperatively. There was no radiological progression of tibiofemoral joint arthritis, using the Ahlback grading, in any patient. One patient, who was diagnosed with rheumatoid arthritis postoperatively, underwent revision to total knee replacement. There were no intraoperative lateral releases and no implant failures. Gender, age, the presence of trochlear dysplasia, patella alta or bilateral surgery did not influence patient outcome. Previous surgery did not correlate with outcome.
CONCLUSION: In contrast to the current literature, the FPV shows promising early results. However, we cannot identify a subgroup of patients with superior outcomes.
Core tip: We demonstrate good outcomes regarding the Femoro-Patella Vialla implant which recently has had poor outcomes reported. As it is a popular implant, we think this article is important as there is a paucity of literature concerning outcomes from independent centres. In addition, we are the first group to use a patellofemoral score as one of the outcome measures. However, we cannot identify a subgroup of patients with superior outcomes.
- Citation: Halai M, Ker A, Anthony I, Holt G, Jones B, Blyth M. Femoro Patella Vialla patellofemoral arthroplasty: An independent assessment of outcomes at minimum 2-year follow-up. World J Orthop 2016; 7(8): 487-493
- URL: https://www.wjgnet.com/2218-5836/full/v7/i8/487.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i8.487
Patellofemoral arthroplasty (PFA) is a bone preserving procedure for the treatment of severe isolated patellofemoral arthritis. Its legacy dates back to Blazina’s first report of PFA in 1979[1]. Early designs, such as the Lubinus device, reported high failure rates[2]. Since then, newer devices have been developed which more accurately mimic normal knee anatomy and patellar alignment. PFA is now a tibiofemoral joint-sparing alternative to traditional total knee arthroplasty in the treatment of patellofemoral arthritis.
The AVON (Stryker Howmedica Osteonics, Allendale, New Jersey) design was developed from the Kinemax plus (Stryker Howmedica Osteonics, New Jersey) which had a low rate of patellofemoral complications. The early results of this prosthesis from the originating centre have been promising[3]. In another prospective review, good results were also experienced in 37 cases at 2 years[4]. However, there have been mixed results in terms of revision rates at short term follow-up for patellofemoral arthroplasty in general, with rates of between 3% and 15% quoted in the literature[5].
Newer devices such as the Femoro-Patella Vialla (FPV, Wright Medical, United Kingdom) have more recently become available. Stated benefits include a broad trochlea with proximal extension, together with a sagittal curve that promotes superior patella tracking. The sulcus angle of the FPV is 140 degrees, which mimics the human trochlear anatomy more accurately, compared to the Avon which has an angle of 125 degrees[6]. The trochlea is also designed to extend distally to the intercondylar notch, ensuring that the patella does not dislocate inferiorly in deep flexion. The patella features a facetted design with a longitudinal ridge which in theory contains the patella more readily in full extension. The footprint of the patella component is oval in shape, increasing patella contact area, in contrast to the AVON which has a medially offset dome.
There have been reports suggesting that the presence of preoperative trochlear dysplasia can be associated with superior outcomes after PFA[7]. Another series have shown that patellofemoral arthritis associated with malalignment, such as patella alta, was the most common clinical presentation prior to PFA[8]. Furthermore, Farr et al[9] confirmed that the best outcome after PFA can be expected when the indication is trochlear dysplasia or patellar malalignment. All of these studies were not based on the FPV.
There are three independent outcome studies of the FPV in the literature, of which two of these report high rates of revision of 17%[10,11]. We are not aware of any studies looking at the effects of pre-existing patella alta, trochlear dysplasia or bilateral disease on outcome of the FPV specifically. In addition, none of the published studies have used a validated patellofemoral score as one of their outcome measures. We report early outcomes of the FPV in 41 consecutive knees with a minimum follow up of 2 years.
Forty-four consecutive FPV PFAs were performed at a single tertiary centre between November 2007 and November 2011. One patient died from unrelated causes and another patient, who had bilateral FPVs implanted, was lost to follow up. The patient lost to follow-up had a normal postoperative recovery and satisfactory radiographs, with no revision surgery documented in their case-notes.
This left 41 FPV procedures in 31 patients producing a 94% follow-up rate. There were 22 females and 9 males. There were 11 patients (22 FPVs) who had bilateral replacements as staged procedures. The mean age of the cohort was 65 years (range 41-81). The mean follow-up was 3.2 years with a minimum of 2-year follow-up for all patients. The causes of the patellofemoral arthritis were as follows: Osteoarthritis (39 cases, 95%) and trauma (2 cases, 5%).
Patients were considered for surgery if they had disabling knee pain, Outerbridge grade 4 patellofemoral arthritis and normal medial and lateral knee compartments on weight-bearing radiographs[12]. The preoperative diagnosis was isolated severe patellofemoral arthritis in all cases. Diagnosis was based on a combination of clinical, radiological and, where available, arthroscopic findings. Previous surgery was documented and summarised in Table 1.
| Previous surgery | No. of knees (% of total) |
| Arthroscopy | 3 (7) |
| Tibial tuberosity transfer | 2 (5) |
| Medial patellofemoral ligament reconstruction | 2 (5) |
| No intervention | 34 (83) |
| Total | 41 (100) |
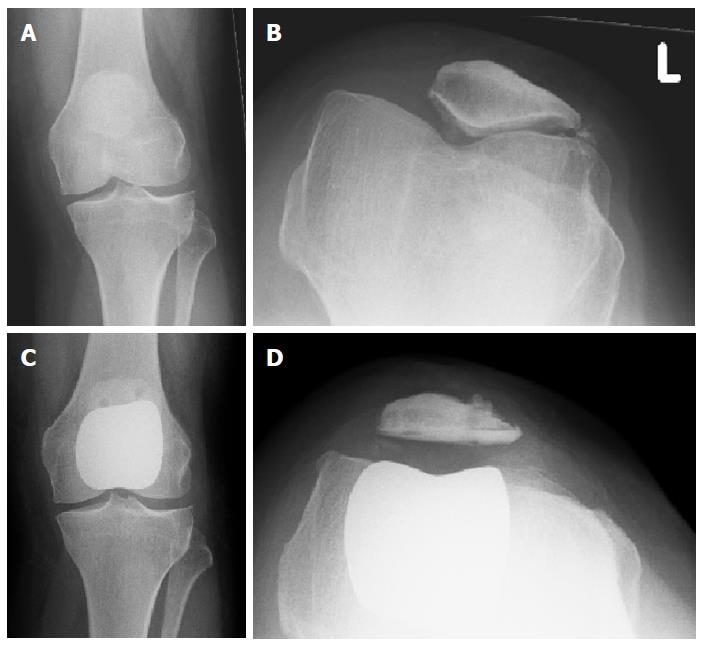
Each patient had a weight-bearing anteroposterior, lateral radiograph and skyline radiograph of their affected knee preoperatively (Figure 1). The presence of a dysplastic trochlea was evaluated on preoperative radiographs, including a true lateral. This was scored independently by two of the authors. Trochlear dysplasia was identified where there was a crossing sign and a sulcus angle greater than 145° as has been previously described[13]. The presence of patella alta was also documented from the lateral preoperative radiographs using the Insall-Salvati ratio[14]. A ratio of greater than 1.2 was taken to be indicative of patella alta.
All operations were performed by, or under direct supervision of, the two senior authors. A medial parapatellar approach was adopted in all cases under pneumatic tourniquet control. All patients had intravenous antibiotics at induction as per local microbiology policy. Palacos R and G cement was used in all cases. No lateral releases were performed. The mean tourniquet time was 49 min. No patients required a blood transfusion postoperatively. The median time for discharge for all patients was at day 3 postoperatively.
Patients were followed in our Outcomes Assessment clinic run by independent nurse practitioners. We performed a retrospective audit of case-notes and radiographs. Patient factors such as preoperative diagnosis and a history of previous surgery or trauma were noted. Functional outcome was assessed at scheduled appointments. These consisted of a preoperative visit and a 3 mo postoperative visit. Thereafter patients were reviewed on a yearly basis. The mean follow-up at the latest appointment was 3.2 years (range 24-58 mo). Patient reported outcome measures included the Oxford Knee Score (OKS) and the validated Melbourne Patellofemoral Score[15,16]. Patient satisfaction with the outcome of the surgery was also documented using a simple 5 point question. The patient was asked in writing, at latest follow-up, to grade their satisfaction postoperatively as: Very satisfied, satisfied, unsure, dissatisfied or very dissatisfied. Radiographs were reviewed postoperatively for the development of tibiofemoral arthritis using the Ahlback grading[17]. Complications were determined at postoperative clinic visits and from the case-notes. The data presented was collected retrospectively and analysed as part of a routine audit of our clinical practice.
All data was analysed using SigmaPlot vs11.0 (Systat Software Inc). Parametric data (Melbourne Score) was analysed using t test and non-parametric data (OKS) was analysed using Mann-Whitney test. Pearson’s correlation was used to determine linear correlation between variables. P value less than 0.05 was considered significant for all tests. The statistical methods of this study were conducted by the biostatistician Iain Anthony of the Glasgow Royal Infirmary.
The median postoperative OKS and Melbourne scores were 40 and 21 respectively at latest follow-up. Thirty-eight percent of patients were very satisfied, 38% satisfied, 10% unsure and 14% dissatisfied with their final result. There were no patients who were “very dissatisfied”. The results are summarised with respect to different patient characteristics in Table 2. Patient factors (gender, the presence of trochlear dysplasia or patella alta, or if bilateral surgery was performed) did not impact on clinical outcome scores. Previous surgery had no significant effect on clinical outcome. No significant correlation was found between age and OKS or Melbourne score (P = 0.162, r = 0.273 and P = 0.278, r = -0.173 respectively).
| Patient factor | Category | n | Median OKS (Q1, Q3) | P value | Mean Melbourne Score (SD) | P value |
| Sex | Male | 12 | 42 (38, 46) | 0.28 | 21.3 (4.7) | 0.31 |
| Female | 29 | 40 (37, 42) | 19.1 (6.4) | |||
| Trochlear dysplasia | Non-dysplastic | 10 | 41 (36, 43) | 0.95 | 20.0 (5.7) | 0.67 |
| Dysplastic | 31 | 41 (38, 43) | 19.0 (7.1) | |||
| Patella alta | Yes | 21 | 41 (37, 42) | 0.56 | 19.3 (6.4) | 0.65 |
| No | 20 | 40 (36, 44) | 20.2 (5.6) | |||
| Uni- or bi-lateral | Unilateral | 19 | 41 (37, 42) | 0.83 | 19.8 (5.6) | 0.97 |
| Bilateral | 22 | 41 (37, 43) | 19.7 (6.4) | |||
| Previous surgery | Yes | 10 | 40 (37, 42) | 0.70 | 22.0 (5.0) | 0.28 |
| No | 31 | 41 (37, 43) | 19.0 (6.1) |
Two patients had superficial wound infections that were diagnosed and treated with a course of oral antibiotics in the community within 2 wk of discharge. Both patients went on to have favourable outcomes and were satisfied. There were no deep infections to date and there have been no infections that have required operative attention. We report no mechanical failures of the FPV prosthesis and there have been no periprosthetic fractures. The complications are included in Table 3.
| Ref. | Implant | Number knees/patients | Mean age (yr) | Mean follow-up (yr) | OKS | Melbourne Score | Patient satisfaction | Trochlear dysplasia | Complications | Further operations |
| Dalury[23] | TKR | 33/25 | 70 | 5.2 | NR | NR | 100% | NR | NR | 0 |
| Ackroyd et al[3] | AVON | 109/85 | 68 | 5.0 | 39 | 25 | 80% | NR | 4 superficial infections 2 stiffness | 4 (4.2%) conversions to TKR |
| Starks et al[4] | AVON | 37/29 | 66 | 2.0 | 39 | 28 | 86% | NR | 1 patella fracture 1 patella resurfacing | 1 (2.7%) patella resurfacing |
| Al-Hadithy et al[22] | FPV | 49/41 | 62 | 3.0 | 38 | NR | NR | NR | 1 scar pain | 3 (6%); 2 (4%) to TKR |
| Williams et al[10] | FPV | 48/48 | 63 | 2.1 | NR | NR | NR | Trochlear dysplasia associated with less revision | 10 persistent pain 1 infection, 1 fracture, 1 hypertrophic scar | 7 (15%); 5 to TKR |
| The present report | FPV | 41/31 | 65 | 3.2 | 40 | 21 | 78% | 84% of cases had trochlear dysplasia preoperatively No difference in outcomes | 2 superficial infections: Treated with oral antibiotics | 1 (2%) conversion to TKR. No lateral releases |
One patient was diagnosed with seronegative rheumatoid arthritis subsequent to her FPV replacement and was revised to a total knee replacement (TKR) at 6 mo following her index procedure. This represents a 97.6% survival at minimum 2 years of follow-up.
At latest follow-up, there was no progression of arthritis of the tibiofemoral joint using the Ahlback grading in any case. In addition there was no medial or lateral tilt of the patella postoperatively and no lateral releases have been performed postoperatively.
Our study shows that good results can be achieved in the short term with the FPV patellofemoral joint replacement. The high Oxford and Melbourne scores observed are reflected in a 78% patient satisfaction rate (satisfied or very satisfied). The procedure compares favourably to TKR with a mean tourniquet time of 49 min, no blood transfusions, a mean length of stay of 3 d and an OKS of 40, at a minimum of 2 years follow-up.
The philosophy behind PFR is theoretically appealing for selected patients with isolated patellofemoral arthritis whom have failed with non-operative therapies. The PFR spares the tibiofemoral joint, with both anterior and posterior cruciate ligaments and menisci, and therefore allows for more natural kinematics, leaving more bone stock for revision surgery[18].
Anatomical patellofemoral abnormalities such as trochlear dysplasia and patella alta are increasingly recognised as the underlying cause of the later development of patellofemoral osteoarthritis. Farr et al[9] concluded in their study that better outcomes after PFR were seen in patients with trochlear dysplasia. Williams et al[10] has recently explored the relationship between trochlear dysplasia and FPV outcomes. They reported 7 revisions in their cohort of 48 knees at 2 years follow-up. Trochlear dysplasia was associated with a significantly lower rate of revision and a lower incidence of persistent pain in their cohort. In our study, it was interesting that over 80% of patients had a dysplastic trochlea according to Dejour’s classification, with over half displaying patella alta. Patellofemoral abnormalities were therefore present in the majority of the patients undergoing surgery in our series, although their presence had neither a positive or negative effect on clinical outcome.
Interestingly, despite the relative paucity of published results, the FPV is the second most used prosthesis for PFR in England and Wales, with the 10th annual National Joint Registry report stating that the FPV was used in approximately 20% of all PFRs performed in 2012 (National Joint Registry for England and Wales[19]). Revision rates for PFR are reported in the National Joint Registry to be 6 times higher than that of primary cemented TKR. Persistent pain is the main cause of revision according to the recent registry data. If all FPVs are considered, the registry calculates a 6.4% (range 4.9%-8.2%) Kaplan-Meier estimate of the cumulative percentage probability of first revision (95%CI) at 3 years. Our 3-year data shows a FPV revision rate of 2%.
Baker et al[20] examined the National Joint Registry and concluded that persistent unexplained pain was the principal reason for early revision following PFR, and that revisions usually occurred within the first 2 years. They suggested that patient selection was extremely important, and that PFR surgery should be concentrated in specialist centres. Therefore, we are encouraged by our 2% rate of revision at 3 years.
As with all partial knee replacements, ease of revision undoubtedly affects the rate of early failure. Faced with the unhappy patient, surgeons are potentially more likely to offer conversion to a TKR, as this can usually be achieved with straightforward surgery using primary TKR implants. However there is evidence that revision of partial joint replacements for unexplained pain does not give the pain relief experienced by those who are revised when a cause for failure has been identified[21]. Our low early revision rate might be explained by our reluctance to offer revision surgery to patients dissatisfied with the results of their procedure unless an identified cause for the dissatisfaction could be found.
A further apprehension about PFR is the advancement of osteoarthritis in the tibiofemoral articulation. In our series, there was no progression of tibiofemoral osteoarthritis at latest follow-up. Patient selection is critical and our success may be explained by our selection of patients with underlying trochelar dysplasia as a cause of their patellofemoral arthritis in the vast majority of cases. These patients are perhaps less likely to develop failure of the remainder of the knee over time, than patients whose patellofemoral arthritis develops as part of a more generalised degenerative process. Tibiofemoral osteoarthritis is not always easily identified either preoperatively. Magnetic resonance imaging (MRI) has been used to identify occult degenerative changes in the tibiofemoral articulation by the presence of subchondral cysts[7]. We did not routinely use MRI to screen for occult tibiofemoral arthritis in our patients and our good early results question the requirement for this expensive screening investigation.
The main weakness of our study is a lack of preoperative scores. In addition, this is a retrospective series with relatively small numbers and we do not have long-term follow-up yet. Nevertheless, out mean follow-up of 3.2 years is the longest for this implant in the literature. We specifically did not use a validated satisfaction score, such as the Western Ontario and McMaster Universities Osteoarthritis Index or SF12, for simplicity as we decided that the outcome measure process had to be streamlined. The satisfaction grading that was used in this study is used for all research projects from our institution.
Table 3 shows that our postoperative results are comparable to those previously published for patellofemoral arthroplasty and for TKR for isolated patellofemoral arthritis. There is one published report by Al-Hadithy et al[22], and they report similar satisfactory FPV outcomes with OKSs of 38 at 3 years. They reported 2 revisions, which were attributed to poor patient selection. Indeed, the one conversion to TKR in our series was due to a subsequent diagnosis of rheumatoid arthritis and this could also be retrospectively attributed to poor patient selection.
In conclusion, our early results suggest that the FPV patellofemoral joint replacement is a good alternative to TKR in the surgical management of advanced isolated patellofemoral osteoarthritis. However, we are unable to identify a subgroup of patients with superior outcomes, however do not recommend this procedure in patients suffering from rheumatoid arthritis. Further research is required to see if these initial promising results are maintained at longer term follow-up.
The knee joint has three compartments: Medial, lateral and patellofemoral. Some patients have isolated patellofemoral arthritis and therefore a novel “patellofemoral arthroplasty” is a treatment option to replace this compartment only, sparing the rest of the native knee joint.
These patellofemoral replacements are new and there is limited outcome evidence on this particular implant: The Femoro Patella Vialla (FPV) arthroplasty.
In contrast to the current literature, the FPV shows promising early results at 2 years in this study. However, the authors cannot identify a subgroup of patients with superior outcomes. The authors do not recommend performing this procedure on patients with a history of inflammatory arthritis.
These encouraging outcomes are some of the first published outside the designing centre. The authors await longer outcome studies.
“Patellofemoral” means the joint of the femur and patella (kneecap).
The authors have submitted a clinical analysis of the efficacy of using FPV patellofemoral joint replacement as a good alternative to total knee replacement in the surgical management of advanced isolated patellofemoral osteoarthritis. The authors have a relatively good selection of patients in the clinical trial (41 replacements in 31 patients) with radiographic observations and lysholm scoring techniques. The paper is well written and will be of interest to readers.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cartmell S, Malik H S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Blazina ME, Fox JM, Del Pizzo W, Broukhim B, Ivey FM. Patellofemoral replacement. 1979. Clin Orthop Relat Res. 2005;3-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Tauro B, Ackroyd CE, Newman JH, Shah NA. The Lubinus patellofemoral arthroplasty. A five- to ten-year prospective study. J Bone Joint Surg Br. 2001;83:696-701. [PubMed] [Cited in This Article: ] |
| 3. | Ackroyd CE, Newman JH, Evans R, Eldridge JD, Joslin CC. The Avon patellofemoral arthroplasty: five-year survivorship and functional results. J Bone Joint Surg Br. 2007;89:310-315. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 4. | Starks I, Roberts S, White SH. The Avon patellofemoral joint replacement: independent assessment of early functional outcomes. J Bone Joint Surg Br. 2009;91:1579-1582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Sarda PK, Shetty A, Maheswaran SS. Medium term results of Avon patellofemoral joint replacement. Indian J Orthop. 2011;45:439-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Davies AP, Costa ML, Shepstone L, Glasgow MM, Donell S. The sulcus angle and malalignment of the extensor mechanism of the knee. J Bone Joint Surg Br. 2000;82:1162-1166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 83] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Nicol SG, Loveridge JM, Weale AE, Ackroyd CE, Newman JH. Arthritis progression after patellofemoral joint replacement. Knee. 2006;13:290-295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Cartier P, Sanouiller JL, Grelsamer R. Patellofemoral arthroplasty. 2-12-year follow-up study. J Arthroplasty. 1990;5:49-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 81] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Farr J, Barrett D. Optimizing patellofemoral arthroplasty. Knee. 2008;15:339-347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Williams DP, Pandit HG, Athanasou NA, Murray DW, Gibbons CL. Early revisions of the Femoro-Patella Vialla joint replacement. Bone Joint J. 2013;95-B:793-797. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Davies AP. High early revision rate with the FPV patello-femoral unicompartmental arthroplasty. Knee. 2013;20:482-484. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Outerbridge RE. The etiology of chondromalacia patellae. 1961. Clin Orthop Relat Res. 2001;5-8. [PubMed] [Cited in This Article: ] |
| 13. | Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1326] [Cited by in F6Publishing: 1170] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 14. | Berg EE, Mason SL, Lucas MJ. Patellar height ratios. A comparison of four measurement methods. Am J Sports Med. 1996;24:218-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 112] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63-69. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 655] [Cited by in F6Publishing: 866] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 16. | Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78:226-228. [PubMed] [Cited in This Article: ] |
| 17. | Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;Suppl 277:7-27772. [PubMed] [Cited in This Article: ] |
| 18. | Hollinghurst D, Stoney J, Ward T, Pandit H, Beard D, Murray DW. In vivo sagittal plane kinematics of the Avon patellofemoral arthroplasty. J Arthroplasty. 2007;22:117-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | National Joint Registry for England and Wales 10th Report 2013. Available from: http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/10th_annual_report. [Cited in This Article: ] |
| 20. | Baker PN, Refaie R, Gregg P, Deehan D. Revision following patello-femoral arthoplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:2047-2053. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Kerens B, Boonen B, Schotanus MG, Lacroix H, Emans PJ, Kort NP. Revision from unicompartmental to total knee replacement: the clinical outcome depends on reason for revision. Bone Joint J. 2013;95-B:1204-1208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Al-Hadithy N, Patel R, Navadgi B, Deo S, Hollinghurst D, Satish V. Mid-term results of the FPV patellofemoral joint replacement. Knee. 2014;21:138-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Dalury DF. Total knee replacement for patellofemoral disease. J Knee Surg. 2005;18:274-277. [PubMed] [Cited in This Article: ] |