Published online Mar 18, 2015. doi: 10.5312/wjo.v6.i2.202
Peer-review started: September 6, 2014
First decision: October 14, 2014
Revised: November 7, 2014
Accepted: December 16, 2014
Article in press: December 17, 2014
Published online: March 18, 2015
The aim is to describe advanced strategies that can be used to diagnose and treat complications after knee arthrodesis and to describe temporary knee arthrodesis to treat infected knee arthroplasty. Potential difficult complications include nonunited knee arthrodesis, limb length discrepancy after knee arthrodesis, and united but infected knee arthrodesis. If a nonunited knee arthrodesis shows evidence of implant loosening or failure, then bone grafting the nonunion site as well as exchange intramedullary nailing and/or supplemental plate fixation are recommended. If symptomatic limb length discrepancy cannot be satisfactorily treated with a shoe lift, then the patient should undergo tibial lengthening over nail with a monolateral fixator or exchange nailing with a femoral internal lengthening device. If a united knee arthrodesis is infected, the nail must be removed. Then the surgeon has the option of replacing it with a long, antibiotic cement-coated nail. The authors also describe temporary knee arthrodesis for infected knee arthroplasty in patients who have the potential to undergo insertion of a new implant. The procedure has two goals: eradication of infection and stabilization of the knee. A temporary knee fusion can be accomplished by inserting both an antibiotic cement-coated knee fusion nail and a static antibiotic cement-coated spacer. These advanced techniques can be helpful when treating difficult complications after knee arthrodesis and treating cases of infected knee arthroplasty.
Core tip: Knee arthrodesis nonunion can be treated effectively with autologous bone grafting and two modes of fixation such as a plate and intramedullary rod. The hardware in a well-fused but infected knee arthrodesis is surgically challenging to remove, but preserving the intact knee fusion is critical. Symptomatic limb length discrepancy after knee arthrodesis can be treated with intramedullary lengthening devices or lengthening over a rod. Temporary knee arthrodesis provides a stable, durable solution to treat infection after total knee arthroplasty in an obese patient.
- Citation: Wood JH, Conway JD. Advanced concepts in knee arthrodesis. World J Orthop 2015; 6(2): 202-210
- URL: https://www.wjgnet.com/2218-5836/full/v6/i2/202.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i2.202
Knee arthrodesis has been performed for more than 100 years and is currently a treatment option for limb salvage in a failed total knee arthroplasty, unilateral post-traumatic osteoarthritis in a young patient, reconstruction after tumor resection, and knee joints that are unable to be reconstructed after severe trauma[1]. Techniques for knee arthrodesis are well documented, but the rates of complications range from 20% to 84%[2-6]. Although postoperative complications are commonplace, little information exists regarding treatment options for these complications.
This article will review how to evaluate a patient presenting with complications after knee arthrodesis. Surgical treatment options for nonunion, limb length discrepancy (LLD), and an infected but solidly united knee fusion will be discussed. In addition, we will discuss our indications and surgical technique for the treatment of infected total knee arthroplasty with a “temporary knee fusion”.
A thorough patient evaluation is paramount when developing a treatment plan for nonunion, LLD, or infection in a united knee arthrodesis. Relevant clinical information regarding the affected extremity includes: the surgical history of the limb (number, type, and date of procedures), infection history (date, culture results, and treatment), and previous difficulties with wound or bone healing. History of draining wounds or constitutional symptoms such as fevers, chills, or weight loss should raise the suspicion of occult infection. Pain should be assessed by determining its location, duration, intensity, and associated alleviating or aggravating factors.
Comorbidities are optimized preoperatively, especially those affecting bone healing such as diabetes, vitamin D deficiency, calcium deficiency, hyperparathyroidism, hypothyroidism, nutritional deficiency, and peripheral vascular disease. Patients are advised to discontinue tobacco use and are informed of its detrimental effects on bone healing.
During the physical examination, the patient’s gait pattern and overall strength are observed. Both lower extremities are inspected for conditions that affect wound healing including venous insufficiency (e.g., edema, varicose veins, venous dermatitis), arterial disease (e.g., cool skin, decreased peripheral pulses), and neuropathy (e.g., hair loss, smooth shiny skin, sensation). The affected extremity is visually inspected for clinical signs of infection (e.g., erythema, effusion, wound drainage, sinus tracts).
Particular attention is paid to the location of previous incisions, skin grafts, and flaps. Poor skin quality or soft tissue integrity is taken into account when developing the surgical plan, as both can lead to wound healing difficulties. Vascular supply to previous flaps must be known so that iatrogenic injury can be avoided.
If unequal limb length is suspected, the “block test” is performed to evaluate functional LLD[7]. To perform this test, 1-cm wooden blocks are placed under the short limb sequentially until the patient feels that the pelvis is level. Functional limb length discrepancy does not always correlate with the objective findings on radiographs.
Radiographic studies should include a bilateral full length standing anteroposterior view and a full length standing lateral view of the affected extremity. A lift should be used to equalize limb lengths and prevent compensatory knee flexion or equinus, which can adversely affect the accuracy of the limb measurements. When radiographs are inconclusive for knee arthrodesis nonunion, the knee can be evaluated with a computed tomography (CT) scan with sagittal and coronal reconstructions.
Laboratory evaluation includes the erythrocyte sedimentation rate and an assessment of C-reactive protein to screen for infection as well as 25-hydroxy vitamin D, serum calcium, serum prealbumin, and serum albumin to identify vitamin or nutritional deficiencies known to affect bone and wound healing. Nutritional deficiencies are treated with high-protein supplements. Vitamin D deficiency is treated as per the Endocrine Society’s Clinical Practice Guidelines[8]. Patients with a body mass index of less than 30 kg/m2 are given oral supplements of 50000 IU vitamin D2 or vitamin D3 weekly for eight weeks, with a goal of increasing serum 25-hydroxyvitamin D to at least 30 ng/mL, with maintenance therapy of 1500 to 2000 IU/d given afterwards[8]. Because vitamin D is fat soluble, obese patients [body mass index > 30 kg/m2] require two to three times more vitamin D than non-obese patients[8].
Nonunion rates range from 17% to 80%[2-5] and are influenced by multiple factors including patient comorbidities, presence of active knee infection, and choice of implant. Nonunion after knee arthrodesis is typically asymptomatic until 6-9 mo after the arthrodesis procedure. Deconditioned and elderly patients are especially likely to have a delay in symptoms of nonunion as they are typically slow to mobilize. Plain radiographs normally confirm the diagnosis of nonunion, and a CT scan is ordered if plain films are indeterminate. If a nonunion is identified on radiographs but the patient is asymptomatic, surgical intervention is not required unless there is evidence of implant loosening or failure.
External fixation and exchange intramedullary nailing have been described as treatment options for nonunion of a knee arthrodesis[9,10]. An implant that no longer provides stable fixation due to failure or loosening should be removed. Nonunion often occurs when a short intramedullary (IM) nail is implanted in a limb with significant metaphyseal bone loss[3,11,12]. These patients always undergo revision from a short IM nail to a long IM nail, as long nails achieve stability through a diaphyseal fit and are capable of neutralizing the long lever arm and forces across the knee joint.
Surgical treatment options for nonunion of a knee arthrodesis with a retained long IM nail include bone grafting the nonunion site with graft harvested using the reamer/irrigator/aspirator (RIA) system (DePuy Synthes, West Chester, PA, United States) plus either exchange intramedullary nailing (EIN) or supplemental plate fixation (SPF). Implant failure, intramedullary canal diameter, soft tissue healing ability, and evidence of current infection must all be considered when deciding between EIN and SPF. In some cases, both EIN and SPF are used.
During EIN, the IM canal is reamed. The process of reaming the canal stimulates new bone formation[13] and also allows a larger diameter nail to be inserted, which provides additional rigidity and strength. Thus, EIN promotes bony healing through both biological and mechanical means.
SPF provides the mechanical advantages of increasing rotational stability, bending stiffness, and torsional stiffness[14]. The existing nail is left in situ. This technique can be helpful when a larger diameter IM nail either cannot be placed or would not provide additional stability at the nonunion site.
Supplemental Plate Fixation with Existing Intramedullary Nail, Harvest with the RIA System, and Bone Grafting.
Positioning: The patient is placed supine on radiolucent flattop table with the ipsilateral arm across the chest and a bump underneath the buttock to allow access to the existing IM nail. The draping should include the bilateral iliac crest, bilateral lower extremities, and previous IM nail entry point. The fluoroscope should be positioned perpendicular to the patient on the opposite side of the nonunion.
Description of procedure: Utilizing clean instruments, IM bone graft is harvested from the uninvolved femur using the RIA system. The RIA system can be used in an antegrade or retrograde fashion, and the technique is described in multiple papers[15-19]. After the bone graft harvest site is closed and sterile dressings have been applied, the graft is placed in a sterile cup on the back table. The authors prefer to obtain bone graft from the iliac crest only when the RIA system cannot be used to obtain bone graft from the uninvolved femur.
To insert the plate and apply the bone graft, a lateral or medial approach is used that is centered over the nonunion. The selection of an approach depends on two factors: soft tissue viability and bony contact. Soft tissue viability is the primary determinant in choice of surgical approach. Soft tissues that are suspicious for poor healing capability (e.g., local scarring, areas of previous flaps, skin grafts) are noted and avoided. An anterior knee incision is not typically performed, as previous procedures often cause significant scarring and decreased soft tissue healing potential. Bony contact is the second most important consideration. The approach should allow the plate to be applied to the nonunion so that the plate has the greatest amount of bony contact and thus the greatest potential for gaining bony apposition, fixation, and stability with plate fixation.
After the incision is made, dissection proceeds directly to bone. The nonunion site is burred until there is bleeding, indicative of viable bone. Autograft, combined with bone morphogenetic protein (BMP) 2, is distributed along the nonunion site. A large fragment plate should be selected that is of sufficient length to allow four screws to be inserted both distal and proximal to the nonunion. The plate is bent to accommodate the flare of the proximal tibia and distal femur. The locking plate can be secured with locking or non-locking screws based on surgeon preference. The plate is centered over the nonunion site and placed either on the medial or lateral aspect of the distal femur and proximal tibia, depending on the surgical approach that was chosen. Strategic plate placement increases the likelihood that bicortical screw fixation will be achieved; typically this involves adjusting the plate to sit slightly anterior or posterior to midline on the bone. Bicortical purchase is not always possible, and in these instances, unicortical purchase is accepted.
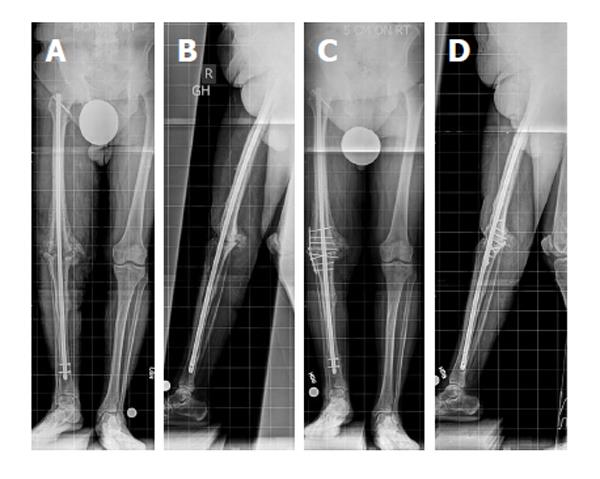
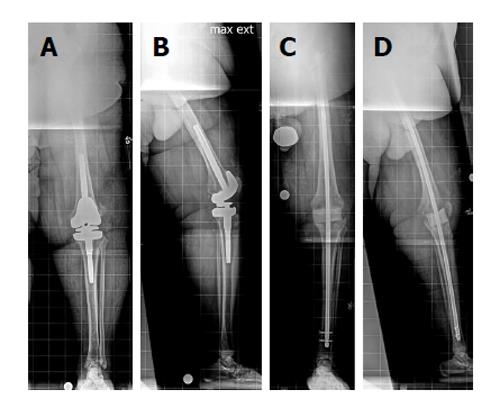
The incision is closed using a standard multilayer closure. Deep drains and an incisional negative pressure dressing are utilized on an as needed basis. Weightbearing is typically restricted for 6 wk, after which gradual progressive weightbearing is allowed (Figure 1).
Positioning: The patient is positioned supine on radiolucent flattop table. The draping includes bilateral iliac crest, bilateral lower extremities, and previous IM nail entry point. The fluoroscope is positioned perpendicular to the patient, on the opposite side of the nonunion. A non-sterile bump is placed under the sacrum to tilt the pelvis, which gives the surgeon access to IM nail entry portal and allows intraoperative lateral fluoroscopic views to be obtained.
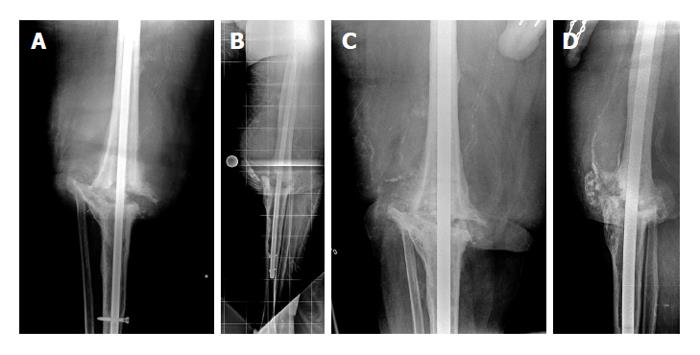
Description of procedure: IM bone graft is harvested from the uninvolved femur using the RIA system. The graft is placed in a sterile cup on the back table. The original IM nail and interlocking screws are removed. The nonunion site is identified, and either a medial or lateral approach is performed as described previously in the supplemental plate fixation technique. A subperiosteal pocket is created to accommodate the bone graft. The femur and tibia are sequentially reamed until osseous tissue is noted on the reamer and there is good chatter. An appropriately sized nail is placed, with a goal of placing a new nail that is 2 to 4 mm larger in diameter than the one that was removed[20]. Interlocking screws are placed for rotational control, and the harvested autograft is combined with BMP-2 prior to placing it in the previously developed subperiosteal pocket. Surgical incisions are closed and sterile dressings placed. Postoperatively, partial weightbearing with a gradual increase to full weightbearing is allowed over the ensuing weeks (Figure 2).
The goal after knee arthrodesis is a 1-cm LLD, with the fused side being shorter to allow for easier foot clearance when walking[21]. Multiple studies have reported an average LLD of greater than 2 cm[22-24], with some authors reporting an average LLD of greater than 5 cm[25,26]. If LLD is more than 1 cm, treatment may be needed. Nonoperative treatment consists of a shoe lift; however, balance issues occur more frequently as the lift height increases, especially when a lift height of 5 cm or more is required. Surgical intervention is considered for symptomatic LLD that cannot be satisfactorily treated with a shoe lift.
To select the appropriate shoe lift height or amount to lengthen, use the “block test” to determine functional LLD. In some cases, patients prefer not to have full correction of the limb length discrepancy. This is important to note so that the patient does not feel “over lengthened” when using the shoe lift or after the lengthening procedure.
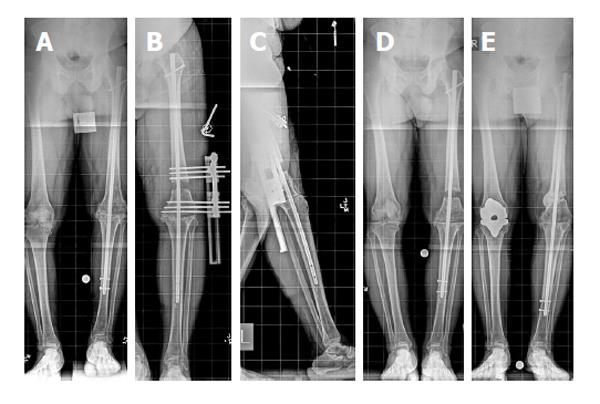
If surgical intervention is needed, options for limb lengthening after knee arthrodesis include lengthening over a nail or exchange nailing with an internal lengthening device (i.e., PRECICE, Ellipse Technologies, Irvine, CA, United States). Advanced age is not a contraindication to distraction osteogenesis[27]. Lengthening over an existing IM nail is a good option in patients whose limb would not tolerate rod removal, typically secondary to incomplete or inadequate healing of the knee arthrodesis. Options for the osteotomy level include the distal femur or the proximal tibia. A distal femoral osteotomy is easier because the fibula does not need to be cut and captured to protect the ankle (Figure 3). Lateral pins must be placed away from the nail. The proximal and distal metaphyseal bone around the knee are the best areas for fixator pins to be inserted.
Lengthening over a nail: Tibia.
Positioning: The patient should be positioned supine on radiolucent flattop table.
Description of procedure: A monolateral external fixator is used for this technique. External fixator pins are placed in the proximal and distal tibial metaphysis using the cannulated wire technique[28]. A total of four 6-mm hydroxyapatite-coated half-pins are used: two in the proximal segment and two in the distal segment. A fibular osteotomy is performed at the junction of the middle and distal 1/3 of the fibula. The fibula must be temporarily held at the level of the distal syndesmosis to protect the ankle joint with a screw. A tibial osteotomy is performed in the proximal tibial metaphysis through anterolateral and posteromedial 1-cm incisions.
Distraction is begun 5 to 7 d after surgery at a rate of 0.75-1 mm/d. Pin-site infections are prevented by using hydroxyapatite-coated pins to decrease loosening. Pin care is performed daily with a saline solution to remove crust from pins. Pin sites are dressed with tightly wrapped Kerlix gauze (Covidien, Mansfield, MA, United States) to prevent soft-tissue pistoning on the skin, which is a major contributor to pin site drainage and infection. If pin-site infections do occur, the majority of cases are treated with 10 d of oral antibiotics.
Postoperatively, the patient attends three to five physical therapy sessions per week to maintain ankle range of motion. Touchdown weightbearing is allowed during the distraction phase and advanced to full weightbearing when consolidation of the regenerate bone has occurred (Figure 4).
Positioning: The patient is positioned supine on radiolucent flattop table. The draping should include the bilateral iliac crest, bilateral lower extremities, and previous IM nail entry point. The fluoroscope is positioned perpendicular to the patient and on the opposite side of the nonunion. A non-sterile bump is placed under the sacrum to tilt the pelvis, which helps the surgeon access the IM nail entry portal and obtain intraoperative lateral view fluoroscopic images.
Description of procedure: The diameter of the PRECICE is selected during preoperative planning and templating. Intraoperative fluoroscopy is utilized to identify the planned osteotomy site, which is typically performed in the subtrochanteric region of the femur. Retained implants are removed from the lower extremity if needed. A small lateral incision is made, and multiple drill holes are placed using the 4.8-mm drill bit at the osteotomy site. These holes allow for local deposit of bone graft during intramedullary reaming and venting of the femur to decrease risk of pulmonary embolism. The femur is then sequentially reamed with a reamer that is 1-2 mm larger than the planned diameter of the PRECICE. A percutaneous osteotome is then used to complete the osteotomy. The PRECICE is inserted into the femur and locked both proximally and distally. A fixator can help control rotation and alignment when inserting the PRECICE nail. The nail is tested intraoperatively to ensure that lengthening occurs. Postoperatively, weightbearing is limited to touchdown until the distraction phase is completed. After the regenerate bone has consolidated, the patient progresses to full weightbearing.
Continued or recurrent infection following knee fusion with an IM nail typically requires nail removal to eradicate the infection. Both long and short IM knee arthrodesis nails are currently in use. Long IM nails are inserted in an antegrade fashion and can be rather easily accessed and extracted through their proximal femoral entry point. Short IM nails, including the Wichita fusion nail (Stryker Orthopaedics, Mahwah, NJ, United States) and the Neff femorotibial nail (Zimmer, Warsaw, IN, United States), are modular and are inserted through the knee. Removal of a short IM nail can be challenging, and preservation of the knee arthrodesis is not always possible. Preoperative evaluation should confirm knee fusion, as an infected nonunion requires a different surgical plan.
Infected knee arthrodesis with retained short intramedullary nail.
Positioning: The patient should be positioned supine on a radiolucent flattop table.
Description of procedure: A sterile thigh-high tourniquet is employed when possible, and the previous anterior knee incision from nail insertion is used for the surgical approach. An anterior bony window is made at the fusion site, and the IM nail is identified.
For the Wichita nail, all interlocking screws and the compression screw must be removed, followed by transection of the nail with the a metal cutting burr such as the Midas Rex Legend Tool (Medtronic, Minneapolis, MN, United States) high speed cutting burr. This occurs through a bone window at the level of the knee. Do not make this window too large or it will be a stress riser at the anterior distal femur and the bone will break during weightbearing. This can be very time consuming as the Wichita nail is solid, thus more than one burr may be needed to transect the nail. Since the metal cutting sound is very abrasive, the author recommends that the surgical team wear earplugs. The separate sections of the nail are then removed through the anterior bony window. The infection is treated with a burr or careful intramedullary reaming and thorough irrigation and débridement. If the limb has only a small area of bone loss, a mixture of antibiotic cement, calcium triphosphate, and hydroxyapatite is placed in this region to help provide support. A long, antibiotic cement-coated IM nail can be placed if a large amount of bone must be débrided or if the fusion is disrupted.
The Neff nail is solid and long. The fusion must be taken down when a Neff nail is used and can be performed through a transverse incision. The knee must be completely flexed to access the canals and extract the rods. Three small screws hold the sections together, and each section can be 30 cm or longer. In these cases, a long antibiotic cement-coated nail is then inserted in an antegrade fashion through the piriformis fossa to repeat the fusion.
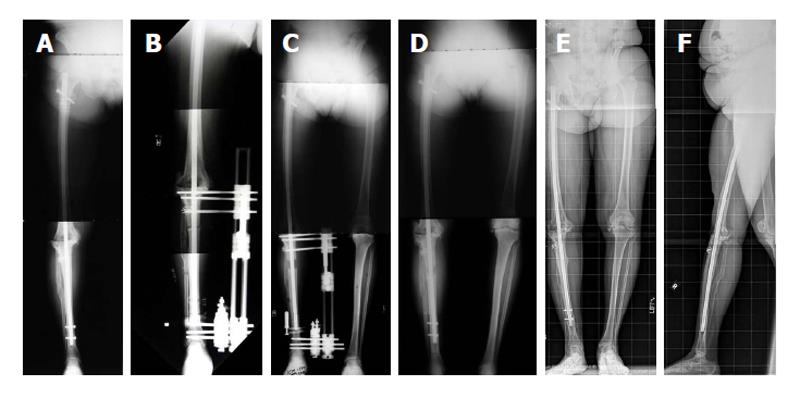
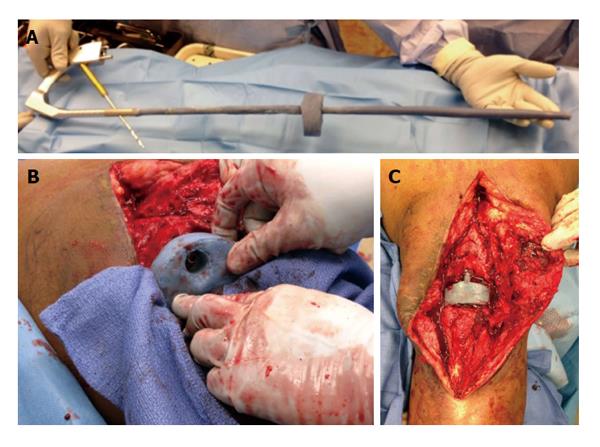
An infected total knee arthroplasty can be one of the more difficult conditions to treat[29]. In the United States, a chronic infection is commonly treated in a two-stage surgical fashion and articulating antibiotic cement-coated spacers are often used during the first stage of treatment[30]. In certain patients, however, an articulating antibiotic cement-coated spacer may not provide adequate stability and postoperative knee dislocation or inability to bear weight may be an issue. In these situations, the senior author has found that performing a temporary knee fusion provides sufficient stability to allow full weightbearing immediately postoperatively without concern for knee dislocation. A temporary knee fusion is accomplished by inserting both an antibiotic cement-coated IM knee fusion nail and a static antibiotic cement-coated spacer (Figures 5 and 6). Patients are considered for a temporary knee fusion if they are morbidly obese, lack an extensor mechanism, have significant soft tissue defects about the knee, or have extensive distal femoral or proximal tibial bone loss. Additionally, periprosthetic nonunion, especially infected nonunion, may warrant this procedure.
This procedure essentially has two goals: eradication of infection and stabilization of the knee. A double setup is utilized (i.e., “clean and dirty”) to remove the knee arthroplasty and resect necrotic bone and soft tissue followed by the reconstruction.
Positioning: The patient is positioned supine on a radiolucent flattop table. A non-sterile bump is placed under the sacrum, slightly off midline towards the operative side. The operative hip and buttock region must be placed at the edge of the table. Positioning the patient with the affected hip at the edge of the table and placing a bump under the sacrum allows the gluteus musculature and associated adipose tissue to fall posteriorly. This facilitates access to the nail insertion site.
Description of procedure: Our double setup includes a Mayo stand positioned at the foot of the bed. Any instrument utilized during the first portion of the procedure is kept on the Mayo stand. The surgical technologist passes clean instruments kept on the back table to the surgical team but avoids physical contact with the surgical team and surgical field, including the Mayo stand.
A medial parapatellar arthrotomy is typically performed, and the total knee arthroplasty components are accessed and removed. A thorough débridement of the bone and soft tissue is performed, including intramedullary reaming of both the femoral and tibial canals. Ball-tipped guidewires and flexible reamers are utilized for retrograde femoral and antegrade tibial reaming that is 2 mm wider than the templated intramedullary nail diameter, including antibiotic coating. The nail length is calculated and includes the entire length of the femur, the knee joint gap (space between distal femur and proximal tibia), and the tibial length to approximately 2 cm above the ankle. Necrotic and infected bone is further débrided with a burr, and synovectomy is performed. The capsule, lateral gutter, and medial gutter are débrided; the Versajet II Hydrosurgery System (Smith and Nephew, Largo, FL, United States) can facilitate posterior débridement. The femoral and tibial canals, as well as the knee joint, are then irrigated with 6 L of saline.
After removal of total knee components, irrigation, and débridement, the entire Mayo stand along with all instruments are removed from the surgical area. All contaminated items are removed from the surgical field (e.g., tubing, bovie). The extremity is re-prepared and re-draped, and all surgical team members change their gowns and gloves. A Trigen knee fusion nail (Smith and Nephew, Memphis, TN, United States) is prepared with an antibiotic cement coating (utilizing silicone tubing as described by Thonse et al[31]) and a static antibiotic cement-coated spacer is fashioned to fit the knee joint gap.
Typically, while the extremity is being irrigated, a member of the surgical team breaks scrub, regowns, regloves, and begins making the antibiotic cement-coated fusion nail and spacer. This allows time for the antibiotic cement to cure so that both the nail and spacer will be ready for insertion after irrigation is completed and the extremity is re-prepared and re-draped.
The antibiotic cement-coated fusion nail is inserted antegrade to the level of the distal femur, the static knee spacer is placed, and the IM nail insertion into the tibia is completed. Interlocking screws are placed proximally and distally. Incisions are closed using non-braided suture, and dressings are placed per routine. Incisional negative pressure wound therapy can be utilized on the anterior knee incision to facilitate healing.
Postoperatively, the patient is allowed to weight bear as tolerated. Antibiotics are tailored based on growth from intraoperative cultures and are typically administered intravenously or orally for 6 wk. Typically, the patient also takes anticoagulation medication for 6 wk.
The authors thank Amanda E Chase, MA, and Alvien Lee for their invaluable assistance with this manuscript.
P- Reviewer: Babis GC, Fisher DA S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ
| 1. | Somayaji HS, Tsaggerides P, Ware HE, Dowd GS. Knee arthrodesis--a review. Knee. 2008;15:247-254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Rothacker GW, Cabanela ME. External fixation for arthrodesis of the knee and ankle. Clin Orthop Relat Res. 1983;101-108. [PubMed] [Cited in This Article: ] |
| 3. | Knutson K, Hovelius L, Lindstrand A, Lidgren L. Arthrodesis after failed knee arthroplasty. A nationwide multicenter investigation of 91 cases. Clin Orthop Relat Res. 1984;202-211. [PubMed] [Cited in This Article: ] |
| 4. | Cunningham JL, Richardson JB, Soriano RM, Kenwright J. A mechanical assessment of applied compression and healing in knee arthrodesis. Clin Orthop Relat Res. 1989;256-264. [PubMed] [Cited in This Article: ] |
| 5. | Conway JD, Mont MA, Bezwada HP. Arthrodesis of the knee. J Bone Joint Surg Am. 2004;86-A:835-848. [PubMed] [Cited in This Article: ] |
| 6. | Conway JD. Arthrodesis of the knee. Limb Lengthening and Reconstruction Surgery. New York: Informa Healthcare 2007; 329-344. [Cited in This Article: ] |
| 7. | Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466:2910-2922. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 207] [Cited by in F6Publishing: 215] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 8. | Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6162] [Cited by in F6Publishing: 6237] [Article Influence: 479.8] [Reference Citation Analysis (0)] |
| 9. | Manzotti A, Pullen C, Guerreschi F, Catagni MA. The Ilizarov method for failed knee arthrodesis following septic TKR. Knee. 2001;8:135-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Rand JA, Bryan RS. The outcome of failed knee arthrodesis following total knee arthroplasty. Clin Orthop Relat Res. 1986;86-92. [PubMed] [Cited in This Article: ] |
| 11. | Wade PJ, Denham RA. Arthrodesis of the knee after failed knee replacement. J Bone Joint Surg Br. 1984;66:362-366. [PubMed] [Cited in This Article: ] |
| 12. | Rand JA, Bryan RS, Chao EY. Failed total knee arthroplasty treated by arthrodesis of the knee using the Ace-Fischer apparatus. J Bone Joint Surg Am. 1987;69:39-45. [PubMed] [Cited in This Article: ] |
| 13. | Pfeifer R, Sellei R, Pape HC. The biology of intramedullary reaming. Injury. 2010;41 Suppl 2:S4-S8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Vohra R, Singh A, Singh KK. Plate augmentation and bone grafting for aseptic nonunions following intramedullary nailing of comminuted fractures of femoral shaft. Pb J of Orthopaedics. 2013;14:26-31. [Cited in This Article: ] |
| 15. | McCall TA, Brokaw DS, Jelen BA, Scheid DK, Scharfenberger AV, Maar DC, Green JM, Shipps MR, Stone MB, Musapatika D. Treatment of large segmental bone defects with reamer-irrigator-aspirator bone graft: technique and case series. Orthop Clin North Am. 2010;41:63-73; table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 16. | Cox G, Jones E, McGonagle D, Giannoudis PV. Reamer-irrigator-aspirator indications and clinical results: a systematic review. Int Orthop. 2011;35:951-956. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 17. | Finkemeier CG, Neiman R, Hallare D. RIA: one community’s experience. Orthop Clin North Am. 2010;41:99-103; table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Conway JD. Autograft and nonunions: morbidity with intramedullary bone graft versus iliac crest bone graft. Orthop Clin North Am. 2010;41:75-84; table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 19. | Belthur MV, Conway JD, Jindal G, Ranade A, Herzenberg JE. Bone graft harvest using a new intramedullary system. Clin Orthop Relat Res. 2008;466:2973-2980. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 122] [Cited by in F6Publishing: 115] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 20. | Brinker MR, O’Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am. 2007;89:177-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Conway JD. Knee arthrodesis. Operative Techniques in Orthopaedic Surgery. Volume 1. Philadelphia, PA: Lippincott Williams Wilkins 2011; 1004-1015. [Cited in This Article: ] |
| 22. | Garcia-Lopez I, Aguayo MA, Cuevas A, Navarro P, Prieto C, Carpintero P. Knee arthrodesis with the Vari-Wall nail for treatment of infected total knee arthroplasty. Acta Orthop Belg. 2008;74:809-815. [PubMed] [Cited in This Article: ] |
| 23. | Leroux B, Aparicio G, Fontanin N, Ohl X, Madi K, Dehoux E, Diallo S. Arthrodesis in septic knees using a long intramedullary nail: 17 consecutive cases. Orthop Traumatol Surg Res. 2013;99:399-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Iacono F, Raspugli GF, Bruni D, Lo Presti M, Sharma B, Akkawi I, Marcacci M. Arthrodesis After Infected Revision TKA: Retrospective Comparison of Intramedullary Nailing and External Fixation. HSS J. 2013;9:229-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Watanabe K, Minowa T, Takeda S, Otsubo H, Kobayashi T, Kura H, Yamashita T. Outcomes of knee arthrodesis following infected total knee arthroplasty: a retrospective analysis of 8 cases. Mod Rheumatol. 2014;24:243-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Bargiotas K, Wohlrab D, Sewecke JJ, Lavinge G, Demeo PJ, Sotereanos NG. Arthrodesis of the knee with a long intramedullary nail following the failure of a total knee arthroplasty as the result of infection. J Bone Joint Surg Am. 2006;88:553-558. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;31-37. [PubMed] [Cited in This Article: ] |
| 28. | Paley D. Principles of Deformity Correction. 1st ed, Corr. 3rd printing. Berlin: Springer-Verlag 2005; . [Cited in This Article: ] |
| 29. | Bengtson S, Knutson K. The infected knee arthroplasty. A 6-year follow-up of 357 cases. Acta Orthop Scand. 1991;62:301-311. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 208] [Cited by in F6Publishing: 170] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 30. | Castelli CC, Gotti V, Ferrari R. Two-stage treatment of infected total knee arthroplasty: two to thirteen year experience using an articulating preformed spacer. Int Orthop. 2014;38:405-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Thonse R, Conway JD. Antibiotic cement-coated nails for the treatment of infected nonunions and segmental bone defects. J Bone Joint Surg Am. 2008;90 Suppl 4:163-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |