Published online Jul 18, 2014. doi: 10.5312/wjo.v5.i3.379
Revised: January 7, 2014
Accepted: April 3, 2014
Published online: July 18, 2014
AIM: To review our outcomes and compare the results of the Less Invasive Stabilization System (LISS) to other implants for distal femur fracture management at a regional Australian hospital.
METHODS: The LISS is a novel implant for the management of distal femur fractures. It is, however, technically demanding and treatment results have not yet been assessed outside tertiary centres. Twenty-seven patients with 28 distal femur fractures who had been managed surgically at the Mackay Base Hospital from January 2004 to December 2010 were retrospectively enrolled and assessed clinically and radiologically. Outcomes were union, pain, Lysholm score, knee range of motion, and complication rates.
RESULTS: Twenty fractures were managed with the LISS and eight fractures were managed with alternative implants. Analysis of the surgical techniques revealed that 11 fractures managed with the LISS were performed according to the recommended principles (LISS-R) and 9 were not (LISS-N). Union occurred in 67.9% of fractures overall: 9/11 (82%) in the LISS-R group vs 5/9 (56%) in the LISS-N group and 5/8 (62.5%) in the alternative implant group. There was no statistically significant difference between pain, Lysholm score, and complication rates between the groups. However, there was a trend towards the LISS-R group having superior outcomes which were clinically significant. There was a statistically significant greater range of median knee flexion in the LISS-R group with compared to the LISS-N group (P = 0.0143) and compared with the alternative implant group (P = 0.0454).
CONCLUSION: The trends towards the benefits of the LISS procedure when correctly applied would suggest that not only should the LISS procedure be performed for distal femur fractures, but the correct principle of insertion is important in improving the patient’s outcome.
Core tip: We recommend that orthopaedic surgeons have a good understanding of the Less Invasive Stabilization System (LISS) principles, and endeavour to follow these principles when using the LISS to treat distal femur fractures. Improved outcomes with the LISS may be achieved by providing more in-service training and courses on the use of this system for orthopaedic surgeons.
- Citation: Batchelor E, Heal C, Haladyn JK, Drobetz H. Treatment of distal femur fractures in a regional Australian hospital. World J Orthop 2014; 5(3): 379-385
- URL: https://www.wjgnet.com/2218-5836/full/v5/i3/379.htm
- DOI: https://dx.doi.org/10.5312/wjo.v5.i3.379
Distal femur fractures are defined as fractures that affect the lower nine to fifteen centimetres of the femur, down to the articular surface of the knee[1-3]. These fractures account for approximately 4% to 6% of all fractures affecting the femur[4]. A study by Martinet et al[5] found that distal femur fractures have a bimodal age distribution. The younger age group comprises mostly males in their second to third decade of life who typically sustain their injuries via high energy mechanisms such as motor vehicle accidents. The older age group mostly comprises females in their sixth decade of life onwards, who typically sustain their injury via low energy mechanisms of injury from osteoporosis[6,7]. Because of its biomechanical specifics, the treatment of distal femur fractures has historically been associated with a high incidence of complications, including non-union or delayed union, malalignment of the femur, infections of the bone and soft tissues, chronic pain and decreased range of motion and function of the knee joint[8-10]. The evolution of the minimally invasive plate osteosynthesis (MIPO) concept, however, has significantly changed the approach to distal femur fracture management[10-13]. The MIPO technique avoids extensive open surgical procedures in order to reduce damage to the blood supply of the bone and surrounding tissues, thus, in theory, facilitating better healing[14,15]. The Less Invasive Stabilization System (LISS) is a novel implant which has been developed to conform to the MIPO concept[16,17]. The LISS incorporates many new features that potentially make it favourable for the management of distal femur fractures[18-20] (Table 1). Despite the proposed benefits of the LISS, a number of limitations have been identified, the most important being the LISS is technically demanding[18]. Many studies have concluded that significant surgical experience is a prerequisite for optimal outcomes when using the LISS implant, however there is limited information on outcomes from using the LISS in the generalist orthopaedic setting[9,18,21,22].
| The approach to the distal femur should be minimally invasive, through either a lateral or antero-lateral incision |
| Stable fixation of the joint fragments is done under direct visualisation |
| The metaphyseal part of the fracture is reduced in a closed manner under image intensifier guidance. Direct Handling of the fracture is avoided, and the fracture must be reduced before application of the LISS |
| The LISS implant is inserted sub-muscularly under image intensifier guidance and is positioned alongside the femur. |
| The LISS is fixed distally and proximally to the femur with locking screws. The screw ratio for the diaphyseal part should be 0.4, meaning that in a 10 hole plate the maximum number of screws should be 4. The diaphyseal screws should have bicortical fixation. |
| The plate used should have a minimum length of nine holes |
| Primary bone grafting of the fracture site is not necessary. |
The aim of this study was to compare the results of the LISS with other implants for distal femur fracture management at a regional hospital where orthopaedic surgeons are not sub- specialised in lower limb conditions. The outcome measures were union, pain, Lysholm score, range of knee motion, and complication rates. The study setting was a regional hospital which services a population of approximately 160000 people, and receives an average of eight to ten distal femur fractures annually.
A retrospective, single centre study was designed to identify and evaluate the method of distal femur fracture management. Potential study participants were identified by a search of Mackay Base Hospital’s electronic clinical database from January 2004 to December 2010. Additionally, a manual search of the electronic surgical records for all orthopaedic surgeries performed at the hospital during this time was undertaken to identify any potential participants missed by the initial primary search.
Participants were included if they had a distal femur fracture and were age > 18 years, able to mobilise independently prior to fracture, and the fracture was managed surgically. Eligible participants were invited to attend an assessment at the orthopaedic outpatient clinic. The assessment involved four components: (1) Lower limbs were examined for fracture site deformity, prominence of the implant, knee range of motion, and pain in the knee and over the implant; (2) A Lysholm questionnaire was completed to determine the level of knee function; (3) Pain was assessed using a Visual Analogue Scale; and (4) Radiographs were taken (standard anterior-posterior and lateral projections of the affected distal femur, and standing long leg radiographs of both legs) to assess the leg length and axis.
Ethical approval was obtained through Queensland health ethics committee. Statistical Analysis was performed using SAS 9.1 (SAS Institute, Cary, NC) and R 2.12.0. Data was categorized based on surgical management: LISS or alternative implants which include distal femoral nail (DFN), dynamic condylar screw (DCS), and angled blade plate (ABP). The LISS group was further sub-classified based on whether the recommended principles of insertion were used (LISS-R) or not (LISS-N). Continuous variables are reported as means, and standard deviations with group comparisons were analysed by variance. Discrete variables are reported as numbers and percentages, with group comparisons analysed by Pearson’s chi-square or Fisher’s exact test. All statistical tests were evaluated at the 5% level of significance.
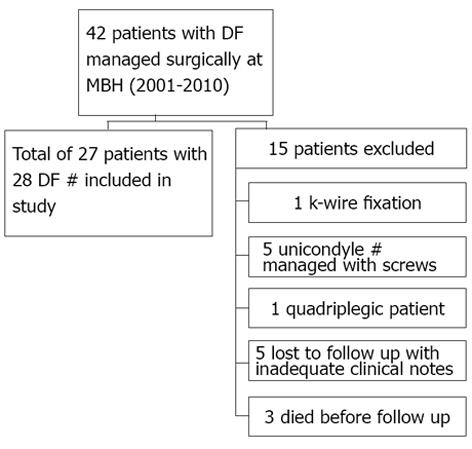
From January 2004 to December 2010, 42 adult patients were managed surgically for distal femur fractures, 32 of which were eligible for this study. Of the 32 eligible participants identified, 27 participants (8 male, 19 female) with 28 distal femur fractures attended an orthopaedic outpatient clinic for further assessment (Figure 1). The participants’ mean age was 64.7 years (range 18 to 94 years) with the mean age of female participants being 72.3 years (range 32 to 94) compared to 46.6 years (range 18 to 81) for males. The mean duration of follow-up for study participants was 30 mo (6 to 74 mo).
Twenty of the 28 fractures (71.4%) were managed with the LISS, while eight (28.6%) were managed with alternative implants: four with Distal Femoral Screw (DFN), three with Dynamic Condylar Screw (DCS), and one with an angular blade plate (ABP). A review of the operative notes revealed that 11/20 (55%) of the LISS procedures had been conducted according to recommend procedures for insertion (LISS-R group). However, 9/20 (45%) of fractures managed with the LISS were not operated on according to the recommended principles, using atypical techniques or implant constructs (Figure 2). There were no significant differences between the three treatment groups (LISS-R, LISS-N and alternative implants) with regard to patient demographics and co-morbidities or periprosthetic factors (Table 2). However, patients in the LISS group had significantly shorter operation times compared to the alternative implant group (P = 0.0048) however, there was no difference in blood loss (P = 0.2304). In regard to rehabilitation post-op, the LISS-R group required less rehabilitation time than both the LISS-N and alternative implant groups (P = 0.0308).
| Surgical implant | P-value | ||||||
| LISS(n = 19) | LISS-R(n = 11) | LISS-N(n = 8) | Alternative(n = 8) | LISS vs alternative | LISS-R vs LISS-N | LISS-R vs LISS-N vs alternative | |
| Surgery within first 48 h | 11 (58%) | 6 (55%) | 5 (63%) | 6 (75%) | 0.6655 | 1.0000 | 0.8773 |
| Operation blood loss (mL) | 521.1 (296.4) | 490.9 (328.5) | 562.5 (261.5) | 806.3 (925.2) | 0.2304 | 0.6173 | 0.4761 |
| Operation time (min) | 118.4 (24.6) | 121.0 (30.0) | 114.8 (16.7) | 158.5 (42.8) | 0.0048 | 0.5988 | 0.0187 |
| Length of acute hospital stay (d) | 11.7 (6.9) | 9.4 (4.6) | 14.9 (8.5) | 8.9 (6.6) | 0.3378 | 0.0859 | 0.1357 |
| No rehabilitation | 11 (58%) | 4 (36%) | 7 (88%) | 7 (88%) | 0.2011 | 0.0587 | 0.0308 |
| Rehabilitation less than 14 d | 4 (21%) | 4 (36%) | 0 (0%) | 0 (0%) | 0.28551 | 0.10321 | 0.02681 |
Overall, 67.9% of fractures proceeded to complete union within six months postoperatively: 14/20 (70%) managed with the LISS compared to 5/8 (62.5%) treated with alternative implants (P = 1.0000). In the LISS-R group 9/11 (82%) achieved complete union versus 5/9 (56%) in the LISS-N group, which was clinically, but not statistically, significant (P = 0.3359).
Pain on a constant or daily basis was reported in 10/27 (47.4%) of fractures treated with the LISS, and 5/8 (62.5%) of fractures treated with alternative implants. Pain was less common in the LISS-R treatment group than LISS-N patients, affecting 3/11 (27.3%) and 6/8 (75.0%) respectively (P = 0.0698), which tended towards significance.
There was no difference in the Lysholm scores between the LISS and alternative implant groups (P = 0.9108).
Knee range of motion (ROM) was categorised into flexion and extension. There was a statistically significant difference in the median knee flexion in the LISS-R group with 102.0 degrees compared to the LISS-N group with 90.0 degrees (P = 0.0143) which remains statistically significant when compared across all implant groups (P = 0.0454) All other primary outcomes did not reach statistical significance (Table 3). There was no statistically significant difference across the different implant groups regarding knee extension (Table 3).
| Surgical implant | P-value | ||||||
| LISS(n = 20) | LISS-R(n = 11) | LISS-N(n = 9) | Alternative(n = 8) | LISS vs alternative | LISS-R vs LISS-N | LISS-R vs LISS-N vs alternative | |
| Median Knee Extension (degrees) | 0.5 (12.5) | 6.0 ( 5.7) | 0.0 (18.2) | 2.5 ( 9.8) | 0.8257 | 0.9134 | 0.9698 |
| Median knee flexion (degrees) | 96.0 (19.6) | 102.0 (13.7) | 90.0 (20.2) | 90.0 (18.5) | 0.8634 | 0.0143 | 0.0454 |
| Median lysholm score | 57.0 (29.4) | 67.0 (30.4) | 42.0 (21.9) | 56.5 (11.0) | 0.9108 | 0.1809 | 0.3075 |
| Excellent (> 90) | 2 (10%) | 2 (18%) | 0 | 0 | 1.00001 | 0.47891 | 0.31481 |
| Good (84-90) | 0 | 0 | 0 | 0 | NA | NA | NA |
| Fair (65-83) | 2 (10%) | 2 (18%) | 0 | 1 (13%) | 1.00001 | 0.47891 | 0.60711 |
| Poor (< 65) | 8 (40%) | 4 (36%) | 4 (44%) | 3 (38%) | 1.0000 | 1.0000 | 1.0000 |
| Union after 6 mo | 14 (70%) | 9 (82%) | 5 (56%) | 5 (63%) | 1.0000 | 0.3359 | 0.4670 |
There were no statistically significant differences in the rate of complications between any of the treatment groups (Table 4). There were 5/20 (25.0%) cases of malunion in the LISS group: 2/11 (18.2%) in the LISS-R group and 3/9 (33.3%) in the LISS N group compared with 4/8 (50.0%) in the alternate implant group. This was clinically but statistically significant. There were 4/20 (20.0%) cases of implant failure in the LISS group: 1/11(9.1%) in the LISS-R group and 3/9 (33.3%) in the LISS-N group compared with 1/8 (12.5%) in the alternative implant group. Again this was of clinical, but not statistical, significance.
| Surgical Implant | P-value | ||||||
| LISS(n = 20) | LISS-R(n = 11) | LISS-N(n = 9) | Alternative(n = 8) | LISS vs alternative | LISS-R vs LISS-N | LISS-R vs LISS-N vs alternative | |
| Complications of healing | |||||||
| Non-union | 6 (30) | 2 (18) | 4 (44) | 2 (25) | 1.0000 | 0.3359 | 0.5065 |
| Delayed union | 0 | 0 | 0 | 1 (13) | 0.28571 | n/a | 0.28571 |
| Varus/valgus malalignment | 5 (25) | 2 (18) | 3 (33) | 4 (50) | 0.3715 | 0.6169 | 0.3627 |
| Recurvation | 2 (10) | 2 (18) | 0 | 0 | 1.00001 | 0.47891 | 0.31481 |
| Limb shortening | 3 (15) | 1 (9) | 2 (22) | 1 (13) | 1.00001 | 0.56581 | 0.80661 |
| Superficial infection | 2 (10) | 2 (18) | 0 | 0 | 1.00001 | 0.47891 | 0.31481 |
| Implant related complications | |||||||
| Implant malpositioning | 2 (10) | 1 (9) | 1 (11) | n/a2 | n/a | 1.00001 | n/a |
| Proximal screw pullout | 1 (5) | 0 | 1 (11) | n/a2 | n/a | 0.45001 | n/a |
| Implant failure | 4 (20) | 1 (9) | 3 (33) | 1 (13) | 1.00001 | 0.28481 | 0.46411 |
Our study shows that when comparing outcomes of fracture union, pain, Lysholm scores, knee ROM, and complication rates, there is no difference between the entire LISS procedure group and the alternative implants group. However, a number of LISS procedures included in this series were performed in a manner contrary to recommended LISS principles. Trends in the results showed better outcomes for patients that were managed with the LISS according to the recommended principles (LISS-R), compared to fractures treated with atypical LISS techniques (LISS-N) or with alternative implants. Difference in median knee flexion was our only significant outcome measure across the implant groups with better outcomes in the LISS-R group. Despite reaching statistical significant, the difference was not considered to be of clinical relevance. On the other hand, the superior outcomes of the LISS-R group compared with the LISS-N groups with regard to union, malunion and implant failure were considered to be clinically significant although the study was not adequately powered to show statistical significance.
Overall, the results of the LISS procedure in our study was worse than in the literature[18,23,24] (Our study has a fracture union rate at 6 mo of 70% which is significantly lower than the literature found - a rate of 85%[23]. However, when examining the LISS-R group only, the union rate at 6 mo become 82% which is much closer to the literature rate.
This was not the case for the Lysholm score where the literature six months after surgery had a score of 80.5 (40-100)[18] where our LISS group had a Lysholm score 57.0 (12 to 100) which was not much improved looking only at the LISS-R group 67.0 (12-100).
A similar trend was seen with the median knee flexion. The median knee flexion of 96 (70 to 136) degrees for the LISS group is lower than the corresponding results in many other studies, such as in the paper by Schandelmaier et al[18] with median knee flexion of 104 (20 to 140). Again, when examining only the LISS-R group, the median knee flexion becomes much closer to the literature result at 102 (90 to 136).
In total, nine of the 20 (45%) fractures fixated with LISS in this study series were managed using a technique which differed from the recommended procedure. Of these, only one had a documented explanation for the deviation from the standard LISS procedure, which was conversion to an open procedure after the closed technique had failed. The most common reasons for divergence from the recommended LISS procedure were the use of short implants and the use of unicortical proximal locking screws for fixation of the LISS in osteoporotic bone. Wong et al[25] reported a 20% failure rate in their study population which they attributed to using short plates and mono-cortical screws. Other authors made similar observations[19,26]. Kregor et al[19] hypothesized that this was caused by the inability of the plate to adequately bridge the fracture and create a construct with enough rigidity and flexibility to allow secondary fracture healing by callus formation. In our population the rate of proximal screw pull-out was 11% (1/9) in the LISS-N with none in the LISS-R group; the most common reason for failure was using an implant that was too short. There were no statistically significant differences in the rate of complications between any of the treatment groups.
An interesting observation was the significant difference in the rehabilitation time required prior to discharge from hospital. The majority of the patients admitted to the rehabilitation ward were in the LISS-R group (78%). Despite the LISS-R group having the most patients, they required the least amount of rehabilitation time, with 57% requiring less than 14 d (P = 0.0308). All the rehabilitation attendees were females older than 55 years with more co-morbidities than the no-rehabilitation patients, including 78% with osteoporosis, 67% with previous TKR, and 22% with diabetes. Following the categorization of distal femur fractures suggested by Martinet et al[5], rehabilitation patients tended to be from the older age group who typically sustained their injury via low energy mechanisms.
To the best of our knowledge, this is the first study to evaluate the use of the LISS implant system in a regional hospital, where surgeon experience with this system and distal femur fracture management in general is limited. Furthermore, it is the first study to identify a distinct series of distal femur fractures that have been treated with the LISS system using a non-recommended technique, and to compare these to other fractures which have been managed according to the recommended principles of this system. Despite small numbers, we think this study successfully explains that good outcomes with the LISS in distal femur fractures are dependent on its correct application. This relies on a comprehensive understanding of the LISS principles by the surgeon and a high level of exposure to, and experience with, the use of the LISS for the treatment of these fractures.
It must be acknowledged that there are several limitations in analysing and generalising our study. The study involved a small number of participants enrolled at a single centre which is a small regional hospital. Numbers do not allow meaningful statistical analysis of several of the outcomes, and in some cases we can provide only a description of our findings. However, our results do show some interesting trends which can inform clinical practice. We feel that the results of this preliminary study can be used to inform future research.
Although most results were not statistically significant, there was a trend towards the correctly inserted LISS-R group having superior outcomes to both the incorrectly inserted LISS-N group as well as the alternative implants. This trend would suggest that not only should the LISS procedure be performed for distal femur fractures, but the correct principle of insertion is important in improving the patients’ outcome.
On the basis of these trends, it is recommended that orthopaedic surgeons have a good understanding of the LISS principles, and endeavour to follow these principles when using the LISS to treat distal femur fractures. Improved outcomes with the LISS may be achieved by providing more in-service training and courses on the use of this system for orthopaedic surgeons.
The Less Invasive Stabilization System (LISS) is a novel implant for the management of distal femur fractures. It is, however, technically demanding and treatment results have not yet been assessed outside tertiary centres.
LISS was introduced in 2000. Early research has shown improved outcomes and reduced complications in comparison with previous conventional implants.
Although most results were not statistically significant, we showed a clinically significant trend towards the correctly inserted LISS-R group having superior outcomes to both the incorrectly inserted LISS-N group as well as the alternative implants. This trend would suggest that not only should the LISS procedure be performed for distal femur fractures, but the correct principle of insertion is important in improving the patients’ outcome.
It is important that LISS is inserted correctly in order to result in better outcomes that alternative implants. Improved outcomes may be achieved by providing more in-service training for orthopaedics surgeons.
Adequate surgeon training for LISS procedures should be emphasized irrespective of clinical experience of the surgeon.
P- Reviewers: Popoola OO, Wu CC S- Editor: Ma YJ L- Editor: A E- Editor: Lu YJ
| 1. | Stover M. Distal femoral fractures: current treatment, results and problems. Injury. 2001;32 Suppl 3:SC3-S13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 55] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Martin JS, Marsh JL, Bonar SK, DeCoster TA, Found EM, Brandser EA. Assessment of the AO/ASIF fracture classification for the distal tibia. J Orthop Trauma. 1997;11:477-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 84] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Swiontkowski MF, Sands AK, Agel J, Diab M, Schwappach JR, Kreder HJ. Interobserver variation in the AO/OTA fracture classification system for pilon fractures: is there a problem? J Orthop Trauma. 1997;11:467-470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 70] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Kolmert L, Wulff K. Epidemiology and treatment of distal femoral fractures in adults. Acta Orthop Scand. 1982;53:957-962. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury. 2000;31 Suppl 3:C62-C63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 167] [Cited by in F6Publishing: 155] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Forster MC, Komarsamy B, Davison JN. Distal femoral fractures: a review of fixation methods. Injury. 2006;37:97-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Kammerlander C, Riedmüller P, Gosch M, Zegg M, Kammerlander-Knauer U, Schmid R, Roth T. Functional outcome and mortality in geriatric distal femoral fractures. Injury. 2012;43:1096-1101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Strømsøe K. Fracture fixation problems in osteoporosis. Injury. 2004;35:107-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 74] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Schütz M, Müller M, Krettek C, Höntzsch D, Regazzoni P, Ganz R, Haas N. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001;32 Suppl 3:SC48-SC54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 229] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 10. | Strømsøe K, Høiseth A. [“Osteoporosis” and physiological variation]. Tidsskr Nor Laegeforen. 2006;126:483. [PubMed] [Cited in This Article: ] |
| 11. | Miclau T, Martin RE. The evolution of modern plate osteosynthesis. Injury. 1997;28 Suppl 1:A3-A6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 73] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997;28 Suppl 1:A20-A30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 209] [Cited by in F6Publishing: 212] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Krettek C, Müller M, Miclau T. Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury. 2001;32 Suppl 3:SC14-SC23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 136] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Kregor PJ, Zlowodzki M, Stannard J. Submuscular plating of the distalfemur. Oper Tech Orthop. 2003;13; 85-95. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Mashru RP, Perez EA. Fractures of the distal femur: current trends in evaluation and management. Curr Opin in Orthop. 2007;18:41-48. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury. 1997;28 Suppl 1:A31-A41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur Less Invasive Stabilization System (LISS). Injury. 2001;32 Suppl 3:SC24-SC31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 163] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 18. | Schandelmaier P, Partenheimer A, Koenemann B, Grün OA, Krettek C. Distal femoral fractures and LISS stabilization. Injury. 2001;32 Suppl 3:SC55-SC63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 143] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 19. | Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury. 2001;32 Suppl 3:SC32-SC47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 153] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Smith TO, Hedges C, MacNair R, Schankat K, Wimhurst JA. The clinical and radiological outcomes of the LISS plate for distal femoral fractures: a systematic review. Injury. 2009;40:1049-1063. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Syed AA, Agarwal M, Giannoudis PV, Matthews SJ, Smith RM. Distal femoral fractures: long-term outcome following stabilisation with the LISS. Injury. 2004;35:599-607. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Kobbe P, Klemm R, Reilmann H, Hockertz TJ. Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury. 2008;39:472-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Schütz M, Müller M, Regazzoni P, Höntzsch D, Krettek C, Van der Werken C, Haas N. Use of the less invasive stabilization system (LISS) in patients with distal femoral (AO33) fractures: a prospective multicenter study. Arch Orthop Trauma Surg. 2005;125:102-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 24. | Markmiller M, Konrad G, Südkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res. 2004;252-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 87] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 25. | Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. Int Orthop. 2005;29:117-120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Kanabar P, Kumar V, Owen PJ, Rushton N. Less invasive stabilisation system plating for distal femoral fractures. J Orthop Surg (Hong Kong). 2007;15:299-302. [PubMed] [Cited in This Article: ] |