Revised: December 9, 2012
Accepted: December 23, 2012
Published online: January 18, 2013
Femoral impaction grafting is a reconstruction option applicable to both simple and complex femoral component revisions. It is one of the preferred techniques for reconstructing large femoral defects when the isthmus is non-supportive. The available level of evidence is primarily derived from case series, which shows a mean survivorship of 90.5%, with revision or re-operation as the end-point, with an average follow-up of 11 years. The rate of femoral fracture requiring re-operation or revision of the component varies between several large case series, ranging from 2.5% to 9%, with an average of 5.4%.
- Citation: Scanelli JA, Brown TE. Femoral impaction grafting. World J Orthop 2013; 4(1): 7-11
- URL: https://www.wjgnet.com/2218-5836/full/v4/i1/7.htm
- DOI: https://dx.doi.org/10.5312/wjo.v4.i1.7
Managing bone loss is one of the most challenging aspects of revision total hip arthroplasty. Femoral impaction grafting is a technically demanding and time consuming procedure, but if performed well, is capable of restoring bone stock in the revision setting with high rates of graft incorporation[1]. The technique was developed in Europe in the 1980’s and popularized by the Exeter, UK group in the early 90’s. Long-term follow-up data is now available showing excellent survivorship beyond 10 years[2,3]. Advances in instrumentation, and the use of longer stems to bypass areas of weak cortical bone distally, have reduced the risk of stem subsidence and femoral fracture[4,5]. The performance time and technically demanding aspects of the operation currently limit its more widespread use compared to other types of revision stems that rely on biologic fixation. The long-term success of impaction grafting ultimately depends on incorporation of particulate allograft into host bone. This process is characterized by an initial inflammatory phase followed by revascularization. Allograft is eventually resorbed and replaced with new host bone by 6-12 mo after the operation.
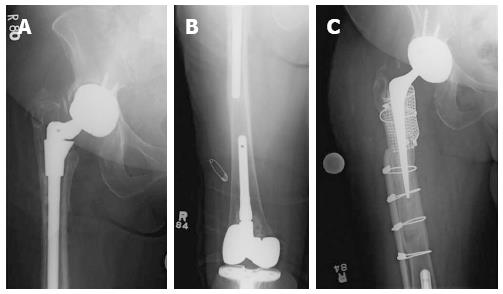
Femoral impaction grafting is an attractive option for restoring femoral bone stock, especially if patients are likely to require an additional reconstructive procedure in their lifetime. It can be used in revisions where the intramedullary canal is > 18 mm, as a fully porous coated stem in this situation is associated with an increased incidence of thigh pain. In femoral defects where there is not 4-6 cm of cortical bone distally to provide scratch fit of a porous coated stem, or the isthmus is non-supportive, femoral impaction grafting is a viable option. If there is minimal cancellous bone present after removal of a femoral stem, impaction grafting is capable of creating a neomedullary canal that allows the use of a cemented stem with durable fixation. When a stem from an ipsilateral total knee arthroplasty prevents femoral component revision of a hip prosthesis with a long extensively porous coated implant, femoral impaction grafting is an option (Figure 1).
A continuous femoral tube must be confirmed intra-operatively before commencing with impaction of cancellous bone, otherwise another technique for revision should be considered. Segmental bone loss that can be converted to a contained defect with metal mesh, allograft struts or bulk allograft is amenable to impaction grafting. Although not commonly used for managing periprosthetic fracture, Tsiridis et al[6] reported a fracture union rate of 84% with 4 year follow-up when femoral impaction grafting was used to manage Vancouver B2 and B3 fractures.
Femoral impaction grafting requires the patient to be medically stable enough to tolerate a long operation. The technique becomes exceptionally challenging in reconstructions where there is near complete loss of the proximal 10 cm of the femur[7]. In these situations, an allograft prosthesis composite or megaprosthesis reconstruction is recommended. Although femoral impaction grafting can be used to manage infection, a two-stage operation is generally preferred over a single-stage revision.
The patient is positioned laterally on the operating table and secured between two hip positioners, ensuring enough space is available to dislocate the hip before prepping and draping. A posterior or posterolateral approach is preferred in all cases and can easily be extended. Previous scars in line with the planned incision are incorporated. The fascia lata is incised along the mid to posterior portion of the femoral shaft and the gluteus maximus bluntly dissected in line with its fibers to allow adequate exposure of the hip joint and proximal femur. The short external rotators and posterior hip capsule are then taken down as a single layer to the level of the lesser trochanter distally and repaired back to the greater trochanter with drill holes at the conclusion of the case. The anterior capsule is elevated off the femoral neck to help deliver the femur out of the wound. The iliopsoas and the femoral insertion of the gluteus maximus tendon are usually taken down to ensure enough soft tissue tension is released to safely dislocate the femur without causing a fracture. A bone hook is placed underneath the femoral neck to lift the femoral head out of the socket instead of rotating through the leg to perform the dislocation.
Prior to removal of the femoral component, the surgeon should ensure enough space is cleared of soft tissue and bone laterally between the prosthesis and the greater trochanter to reduce the risk of femoral fracture during stem extraction. An extended trochanteric osteotomy is utilized if the stem cannot be removed easily. If a cemented stem is being revised, the cement is carefully removed with an osteotome, high-speed burr or ultrasonic device. If the cement plug is well fixed and is >2 cm from the tip of the planned revision stem, it need not be removed and can be left in situ to occlude the femoral canal distally.
Particulate allograft bone is the most common graft type utilized for impaction grafting. The structural support provided by the impacted graft depends on the size of the graft as well as how tightly the graft is packed at the time of revision surgery[8]. The optimal graft size and method of preparation is currently debated amongst surgeons. Commercially available bone mills typically produce graft sizes of 2 to 5 mm, however some published data suggests that larger sizes (7 to 10 mm) of graft material provide better stability[9]. Washing the graft prior to impaction removes fat and marrow contents, which theoretically improves the resistance to shear stresses and enhances frictional resistance providing a more mechanically stable environment to support the prosthesis and allow incorporation of the graft with host bone[10]. In general, smaller pieces of bone graft are impacted distally and larger ones used proximally at the time of reconstruction.
A continuous femoral tube must be confirmed intra-operatively before commencing with impaction of bone graft. This starts with assessing the size and location of femoral endosteal and cortical bone loss from pre-operative radiographs. Areas of cortical bone destruction around the tip of the stem to be revised deserve close attention. These are frequently the site and cause of femoral fractures[4], and the surgeon should attempt to bypass these defects by two cortical diameters at the time of impaction grafting. Otherwise these areas should be reinforced with allograft struts or plate fixation. Fractures have occurred through these stress risers when reinforcement with only metal mesh or cerclage wires was performed[3]. Prophylactic cerclage wires should also be used liberally to reinforce weak areas of cortical bone.
A threaded distal intramedullary plug is placed 2 cm beyond the tip of the planned revision stem whose length and offset are determined from templating pre-operative radiographs. A central guidewire is screwed into the occlusion plug through which cannulated instruments are advanced to impact bone graft with a slotted mallet. The largest phantom (femoral stem shaped bone tamp) that passes through the canal without impinging distally with the appropriate offset is selected. Next, a series of distal impactors are chosen and marked according to the depth to which they should be advanced. Impaction of bone graft starts distally and advances proximally until the femur is backfilled to the mid-portion of the diaphysis. The phantom is then used to impact bone graft while being sure the desired amount of anteversion is reproduced with each sequential impaction. Graft impaction continues until there is enough axial and rotational stability of the phantom to allow a trail reduction. Metal mesh and cerclage wires are then used to reconstruct the proximal femur. The phantom is left it place and then larger bone graft pieces impacted around the phantom with proximal tamping instruments. The phantom should be difficult to remove at the conclusion of graft impaction and axial and rotational stability achieved.
The canal is then dried with a suction device that threads into the phantom and a collarless, polished, tapered femoral stem cemented in place. The distal aspect of the neomedullary tube takes the shape of a thin cone, which requires the cement to be inserted with a low enough viscosity to squeeze through a narrow tipped nozzle.
After the cementation is complete and the femoral head reduced, the wound is copiously irrigated and the short external rotators and hip capsule repaired back to the proximal femur through drill holes with a heavy non-absorbable braided suture.
Deep drains are utilized, and the incision is closed in layers in routine fashion.
Total hip precautions are instituted after surgery and start with a hip abduction pillow placed between both lower extremities at the conclusion of the operation. Radiographs are taken shortly after surgery to assess whether there are any areas of cortical bone that may be deemed high risk for a post-operative fracture and to confirm there are no complications that would require early return to the operating room. Patients are frequently fitted for an abduction orthosis limiting hip flexion greater than 70 degrees to decrease torsional forces on the femoral stem and decrease the risk of implant loosening. The patient is mobilized on the first post-operative day and is toe touch weight bearing for 6 wk followed by gradual advancement of weight bearing to tolerance.
If the indication for femoral impaction grafting is primarily to reconstitute cancellous bone loss and cortical bone is otherwise structurally intact, it is reasonable to allow weight bearing to tolerance in the acute peri-operative period. The hospital stay varies amongst different countries, but in the United States patients usually are discharged after 3 d. The patient returns for follow-up at 6 wk, 12 wk, 6 mo, 1 year and then every 2 years for clinical and radiographic surveillance.
The long-term survivorship of the prosthesis depends on the success of graft incorporation. Ling et al[11] performed histological analysis following post-mortem retrieval of revisions utilizing femoral impaction grafting. The authors described three zones of different cellular morphology and activity: A “deep zone” adjacent to the implant contained necrotic bone encased by cement, an “interface zone” consisted of osteoid in direct contact with methyl methacrylate and scattered giant cells. There was no evidence of viable mineralized bone in direct contact with cement in this zone. The “outer zone”, or regenerated cortical zone, was composed of normal cortical bone, fatty bone marrow and a few contained areas of dead bone.
Histology from biopsy specimens taken at multiple time points over a 4 year period from 19 patients who underwent revision surgery with femoral impaction grafting showed a cellular response characterized by infiltration of fibrous tissue into impacted bone graft with new peripherally located bone formation by one year. Reabsorption of bone graft however can take years to complete. Areas of necrotic bone were identified adjacent to well-fixed stems at 4 years from the time of revision surgery[12].
Halliday et al[4] reported 90.5% survivorship of 226 hips with re-operation as the end point with 10-11 year follow-up using the Universal Exeter stem in all cases. Femoral fracture was the most common indication for re-operation in this series. The authors reported 17 (7.5%) intra-operative femoral fractures. Eight of these were managed at the time of the initial procedure without requiring further surgery. The reported rate of revision for aseptic loosening for any cause after the initial procedure was 7%. The authors noted poor quality bone around the tip of the femoral stem probably predisposed some patients to femoral fractures. This led the group to modify their technique by using longer femoral stems for most revision cases and the development of instrumentation that permits impaction grafting along the entire length of the stem to bypass these inherently weak areas of femoral cortical bone.
Lamberton et al[2] found a 84.2% 10 year survival rate in their cohort of 487 patients treated with femoral impaction grafting with revision for any reason as the primary end-point. With aseptic loosening as the end-point, the 10-year survival rate was 98%. The most common intra-operative complication was perforation of the femoral shaft (8.5%). Other intra-operative complications included fracture of the greater trochanter (3.5%), calcar (5.9%) and femoral shaft (1.9%). The authors used supplemental fixation in the form of cerclage wires, cables, cortical strut allograft, metallic mesh or dynamic compression plating in 56% of the 540 revisions in their series of 487 patients. 36% of the 540 revisions required the use of 2 or more types of reinforcement to manage deficient bone stock to make impaction grafting feasible. The post-operative rate of femoral fracture was 5.4%.
A retrospective review of the Swedish National Joint Registry[13] revealed 1305 cases of femoral impaction grafting in 1188 patients with a mean age of 71 years at the time of revision surgery. Kaplan-Meier survivorship at 15 years was 94% considering all causes of failure. There was no difference in survivorship of the femoral component with respect to age or gender in the study group. The authors found centers where over 100 cases of femoral impaction grafting were performed had better outcomes. Interestingly, there was not difference in the rate of survivorship in revisions using a long stemmed femoral component over a shorter stem. The majority of complications requiring revision after the initial femoral impaction grafting procedure occurred within four years. Infection and femoral fracture were the most common complications (47.5%), while aseptic loosening (15.7%) and subsidence (18.6%) were also cited as causes of failure.
Wraighte et al[14] retrospectively reviewed 75 patients who were treated with femoral impaction grafting and reported a 92% survivorship with revision for any reason as the end-point with a mean follow-up of 10.5 years. Intra-operative fracture was associated with an increased risk of post-operative subsidence of the femoral component. The median subsidence of the femoral stem was 2 mm at 1 year and 10-year follow-up. Femurs with greater pre-operative bone loss were at higher risk of subsidence after impaction grafting. The data from the study group however showed no association between long-term clinical outcome and subsidence of the femoral component. Patients being re-revised for infection were more prone to complications than patients being managed for aseptic loosening with impaction grafting. The median Harris Hip score was 80.6 at the mean follow-up duration of 10.5 years and 88% of patients were either pain free or reported only mild pain.
Sierra et al[15] retrospectively reviewed 567 cases of femoral impaction grafting from the Princess Elizabeth Orthopaedic Centre at Royal Devon and Exeter Hospital in Exeter, United Kingdom to determine the rate of post-operative periprosthetic fracture using a long stemmed (> 220 mm) femoral component. They established a cohort of 40 patients in whom 42 revisions were performed with a long stemmed femoral component and had a minimum follow-up of 5 years. The average age of their study group was 73.8 years. They found a substantial post-operative surgical complication rate of 33%, but only 2 of the 42 cases (4.7%) resulted in post-operative femoral fracture. The survival rate at 5 and 10 years with re-operation of the femur for any reason was 82%.
Schreurs et al[3] reported 100% survivorship of 33 femoral revisions managed with impaction grafting at a mean of 10.4 years with revision of the femoral component as the end-point. Three femoral fractures occurred post-operatively at three, six and twenty two months and successfully treated with open reduction and internal fixation. This decreased the survivorship to 85% at nine years with re-operation for any reason as the end-point. These fractures occurred at the tip of the stem where a segmental defect existed at the time of impaction grafting. In one case it was reinforced with metal mesh at the time of the initial procedure, and not reinforced in the other two. Two of the three post-operative fractures resulted from a fall and the other occurred unexpectedly. Three intra-operative complications resulted in femoral fracture that were not identified at the time of surgery, but successfully healed without an additional operation. Subsidence of the femoral stem within the cement mantle was common and averaged 3 mm over the case series. The largest change in stem position occurred within the first six months after impaction grafting. Interestingly, subsidence did not deleteriously affect Harris Hip scores. Seven patients with an average Harris Hip scores of 85 points, developed subsidence of the femoral stem within the cement mantle > 5 mm.
In conclusion, Femoral impaction grafting is primarily indicated for restoring bone stock in patients who require reconstruction of the femoral component, and for type IV femoral defects where the isthmus is not capable of supporting an implant that relies on biologic fixation. There are concerns about the risk of iatrogenic fracture both intra-operatively and post-operatively as well as subsidence[16]. The procedure is technically challenging and time consuming. Femoral impaction grafting is not suitable for patients who are medically unable to tolerate a long procedure, or where an intact femoral tube cannot be restored. Despite the potential drawbacks of impaction grafting, this technique is associated with high survivorship rates at ten-year follow-up (Table 1), and represents a viable option when an extensively porous coated stem cannot be used.
| Ref. | No. of femoral impaction grafting cases | Average follow-up (yr) | Outcome measures | Survivorship | Rate of femoral fracture | Rate of infection |
| Lamberton et al[2] | 540 | 10 | Revision | 84.2% | 5.4% | 3.9% |
| Schreurs et al[3] | 33 | 10.4 | Revision | 100% | 9% | 0.0% |
| Halliday et al[4] | 226 | 10 | Re-operation | 90.5% | 7.5% | 2.2% |
| Ornstein et al[13] | 1305 | 15 | Revision | 94% | 2.5% | 1.4% |
| Wraighte et al[14] | 75 | 10.5 | Revision | 92% | 2.6% | 1.3% |
| Sierra et al[15] | 42 | 10 | Re-operation | 82% | 4.7% | 4.8% |
| Summary | 2221 | 11 | Re-operation (including revision) | 90.5% | 5.3% | 2.3% |
P- Reviewers Sakamoto A, Sikorski JM S- Editor Cheng JX L- Editor A E- Editor Zhang DN
| 1. | Deakin DE, Bannister GC. Graft incorporation after acetabular and femoral impaction grafting with washed irradiated allograft and autologous marrow. J Arthroplasty. 2007;22:89-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Lamberton TD, Kenny PJ, Whitehouse SL, Timperley AJ, Gie GA. Femoral impaction grafting in revision total hip arthroplasty: a follow-up of 540 hips. J Arthroplasty. 2011;26:1154-1160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Schreurs BW, Arts JJ, Verdonschot N, Buma P, Slooff TJ, Gardeniers JW. Femoral component revision with use of impaction bone-grafting and a cemented polished stem. J Bone Joint Surg Am. 2005;87:2499-2507. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Halliday BR, English HW, Timperley AJ, Gie GA, Ling RS. Femoral impaction grafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg Br. 2003;85:809-817. [PubMed] [Cited in This Article: ] |
| 5. | Howie DW, Callary SA, McGee MA, Russell NC, Solomon LB. Reduced femoral component subsidence with improved impaction grafting at revision hip arthroplasty. Clin Orthop Relat Res. 2010;468:3314-3321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Tsiridis E, Narvani AA, Haddad FS, Timperley JA, Gie GA. Impaction femoral allografting and cemented revision for periprosthetic femoral fractures. J Bone Joint Surg Br. 2004;86:1124-1132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 64] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Buttaro MA, Comba F, Piccaluga F. Proximal femoral reconstructions with bone impaction grafting and metal mesh. Clin Orthop Relat Res. 2009;467:2325-2334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Malkani AL, Voor MJ, Fee KA, Bates CS. Femoral component revision using impacted morsellised cancellous graft. A biomechanical study of implant stability. J Bone Joint Surg Br. 1996;78:973-978. [PubMed] [Cited in This Article: ] |
| 9. | Schreurs BW, Slooff TJ, Buma P, Verdonschot N. Basic science of bone impaction grafting. Instr Course Lect. 2001;50:211-220. [PubMed] [Cited in This Article: ] |
| 10. | Dunlop DG, Brewster NT, Madabhushi SP, Usmani AS, Pankaj P, Howie CR. Techniques to improve the shear strength of impacted bone graft: the effect of particle size and washing of the graft. J Bone Joint Surg Am. 2003;85-A:639-646. [PubMed] [Cited in This Article: ] |
| 11. | Ling RS, Timperley AJ, Linder L. Histology of cancellous impaction grafting in the femur. A case report. J Bone Joint Surg Br. 1993;75:693-696. [PubMed] [Cited in This Article: ] |
| 12. | Ullmark G, Obrant KJ. Histology of impacted bone-graft incorporation. J Arthroplasty. 2002;17:150-157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 104] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Ornstein E, Linder L, Ranstam J, Lewold S, Eisler T, Torper M. Femoral impaction bone grafting with the Exeter stem - the Swedish experience: survivorship analysis of 1305 revisions performed between 1989 and 2002. J Bone Joint Surg Br. 2009;91:441-446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Wraighte PJ, Howard PW. Femoral impaction bone allografting with an Exeter cemented collarless, polished, tapered stem in revision hip replacement: a mean follow-up of 10.5 years. J Bone Joint Surg Br. 2008;90:1000-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Sierra RJ, Charity J, Tsiridis E, Timperley JA, Gie GA. The use of long cemented stems for femoral impaction grafting in revision total hip arthroplasty. J Bone Joint Surg Am. 2008;90:1330-1336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID. Massive early subsidence following femoral impaction grafting. J Arthroplasty. 1997;12:535-540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 189] [Article Influence: 7.0] [Reference Citation Analysis (0)] |