Published online May 18, 2022. doi: 10.5312/wjo.v13.i5.454
Peer-review started: December 29, 2021
First decision: February 21, 2022
Revised: March 19, 2022
Accepted: April 27, 2022
Article in press: April 27, 2022
Published online: May 18, 2022
Surgical treatment of complex fractures of the distal femur in the elderly is controversial. Osteoporosis and pre-existent osteoarthritis are common comorbidities in the elderly which add to the need for early walking and rapid restoration of function and also pose significant obstacles to achievement of satisfactory results with standard fixation techniques. Recently, several authors have suggested that primary arthroplasty could be a viable alternative option to standard fixation techniques in selected patients with complex distal femur fractures.
To present our experience with 11 cases of distal femur fractures treated with knee arthroplasty and large femoral resection in a population of patients over the age of 85.
Data from 11 consecutive patients (10 females, 1 male) presenting with acute intra-articular supracondylar or intercondylar distal femur fractures and with pre-existent primary osteoarthritis who were treated with primary knee arthroplasty were recorded. We collected standard demographic data, comorbidities and patient reported outcomes including Visual Analogical Scale (VAS), Oxford Knee Score (OKS) and Barthel’s Index. Post-operative joint range of motion (ROM) and standard radiographic data were also collected.
At a mean follow-up of 23.2 mo, all of the implants were well-positioned and osteointegrated. Furthermore, all the patients were alive and walking either independently or with walking aids. There was a marked improvement in pain (VAS 4.5 postop vs 1.9 at the last follow-up), OKS score (29.5 postop vs 36.81 at the last follow-up), ROM (96.2° postop vs 102° at the last follow-up) and restoration of pre-injury ambulatory status (average Barthel Index 77.3). The radiographic evaluations showed good restoration of the articular geometry. No deaths and no complications were recorded.
In conclusion, we believe that knee megaprosthesis in the case of complex fractures of the distal femur is a valid surgical choice. This is particularly true in elderly patients with severe osteoporosis and pre-existing osteoarthritis. It is important to note that this surgery should be performed by surgeons with proven experience in prosthetic hip and knee surgery and that a scrupulous selection of the cases is completed.
Core Tip: We evaluated safety and efficacy of a knee megaprosthesis in the setting of complex fractures of the distal femur in elderly patients with a short-term follow-up. We retrospectively evaluated 11 patients over the age of 85 treated with distal femoral replacement with a fully porous coated metaphyseal sleeve for acute fractures of the distal femur with a minimum follow-up of 2 years. During our study period we observed stability of the implants and improvement in the Visual Analogical Scale, Oxford Knee Score, range of motion, Barthel Index, quality of life and survival.
- Citation: Zanchini F, Piscopo A, Cipolloni V, Fusini F, Cacciapuoti S, Piscopo D, Pripp C, Nasto LA, Pola E. Distal femur complex fractures in elderly patients treated with megaprosthesis: Results in a case series of 11 patients. World J Orthop 2022; 13(5): 454-464
- URL: https://www.wjgnet.com/2218-5836/full/v13/i5/454.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i5.454
Fractures of the distal femur account for 0.4% of all bone fractures and 4% of all femoral fractures[1]. The incidence of this type of fracture is 8.7/100000/year[2] and it is steadily increasing due to the aging population, an increase of active elderly people and fragility fractures. Lower limb fragility fractures, both at the hip and the knee joint, represent a significant cause of morbidity and mortality in the elderly population as widely reported in the literature[2]. In many institutions a general trend toward early (i.e. within 48 h of injury) surgical intervention has been reported in an attempt at reducing the number of complications and 1-year mortality which it is estimated at 14%-36%[3]. Distal femoral fractures are most prevalent in females with a male-to-female ratio of 1:2 and have a bimodal distribution: in young people with healthy bones following a high energy trauma and in the osteoporotic elderly population following a low energy trauma. Fifty percent of these fractures are in fact found in patients above the age of 70[4].
Treatment of distal femoral fractures in the elderly has greatly improved with the evolution of implant technology, geriatric care, nursing assistance and physiotherapy. Historically, these fractures were managed in a conservative manner with trans-skeletal traction combined with bracing and followed by a prolonged period of immobilization. Nowadays, several surgical options exist for distal femur fractures including: retrograde intramedullary nailing, open reduction and internal fixation with plates and screws, variable angle locking compression plate, closed reduction and internal fixation with plates and screws, less invasive stabilization systems using minimally invasive plate osteosynthesis technique and external fixation. Other available techniques include arthroplasty in the acute setting or arthrodesis[5].
Although open reduction and internal fixation with locking plates is perhaps the most common method for treatment of these fractures, it retains a high rate of synthesis failure and loss of reduction in the elderly (i.e. up to 30% to 79% of cases)[6]. The osteoporotic bone is indeed less resistant to axial and torsional loading regardless of the internal fixation method used to stabilize the fracture. Furthermore, another important factor to take into account in these fractures is the presence of preexisting arthritis which may lead to an unsatisfactory outcome. Currently, the most popular technique to overcome these limitations is a staged total knee arthroplasty (TKA) procedure in which the fracture is repaired first, then a prosthetic implant is fitted after fracture healing. However, this method shows a high rate of arthrofibrosis, progressive reduction of the post-operative range of motion (ROM) as well as a modification of the anatomical and mechanical axis of the femur. An alternative approach is the primary TKA in the acute setting with the use of implants such as constrained prosthesis[7].
Currently, the use of distal femur replacement (DFR) in distal femur fractures can be considered for low-activity elderly patients with one or several of the following: severely comminuted intra-articular fracture patterns, osteoporosis, concomitant knee osteoarthritis and low pre-injury functional status. The goal of DFR is to resect the fracture and to allow full weight bearing as soon as possible to reduce hospital stay and to prevent complications such as deep vein thrombosis, pulmonary complications and other sequelae of post-operative decreased mobility. The aim of this study was to present our experience with treatment of complex fractures of the distal femur in an elderly osteoporotic cohort of eleven patients treated with acute knee megaprosthesis.
Following Institutional Review Board approval, we retrospectively reviewed a total of 11 patients who underwent total knee arthroplasty for acute fractures of the distal femur at our institution between 2014 and 2019. The inclusion criteria for the surgical procedure were: age of 85 or older, the presence of an acute (treated within 1 mo of the injury) traumatic low or high energy comminuted fracture, intra-articular supracondylar or intercondylar distal femur fracture (AO/OTA classification 33C), pre-existent primary or post-traumatic osteoarthritis Kallgren-Lawrence stage 3 or higher[8], pre-fracture walking distance > 200 m and a body mass index (BMI) < 35 kg/m2. The reason to restrict our study to patients over the age of 85 was based on the clinical finding of the overall bad outcomes reported for these patients following complex, comminuted articular fractures of the distal femur[6]. The same senior surgeon performed all surgical procedures. Patients with pathological fractures of the distal femur, dementia, inability to ambulate before the injury, infections, periprosthetic fractures, the presence of bilateral injuries, patients suffering from inflammatory diseases (rheumatoid arthritis) and/or neurological diseases (neurovascular event, chronic diseases) were not included.
To assess the presence of significant osteopenia or osteoporosis, standard radiographs were used to search for cortical thinning and hyper-transparency of the bone[7,9]. At the same time, the severity of degenerative disease was determined by the presence of subchondral sclerosis, subchondral cysts formation and periarticular osteophyte formation. Clinical data, radiological exams and outcome scores were evaluated by an independent researcher not involved in the care of the patients.
In all cases, a total cemented knee arthroplasty system was used (LPSTM Limb Preservation System, De Puy Synthes, Raynham, Massachusetts, United States). This is a megaprosthesis with modular distal femoral components, a cemented femoral and tibial stem with a fully porous coated metaphyseal sleeve, modular tibial component and a rotating hinge articulation. All surgical procedures were performed under spinal anesthesia; 2 g of cefazolin was administered before surgery and at 8, 16, 24 and 48 h after the surgery. Tranexamic acid was used for bleeding control, administered preoperatively, intraoperatively and 3 h after surgery. An intraoperative blood loss recovery system was used in all cases. Deep vein thrombosis prophylaxis with a daily dose of low molecular weight heparins was used during the first 35 d after surgery in all cases, starting from 24 h after the procedure. The procedure was performed using a standard medial parapatellar approach, the distal femoral fractures fragments were removed by subperiosteal dissection within a minimum distance of 8 cm from the joint line and retained on the operating room back table to allow for approximate sizing of components. Any other fragments proximal to the resection line were stabilized with metal wires (Orthopaedic Cable System, De Puy Synthes Trauma, NJ, United States). Placement of a "prophylactic" banding wire using a 1.7 mm De Puy Synthes Trauma Cable around the proximal end of the remaining diaphysis may potentially decrease the risk of intra-operative fracture during press-fit insertion of a porous femoral sleeve particularly with fragile bone. Furthermore, the crimp may be used as a landmark to help set femoral rotation throughout the operation. After a 1 cm proximal tibial cut, the tibial canal was sequentially reamed and broached to the appropriate size, followed by assembling of the final components. The tibial components were placed in a press-fit fashion with a small amount of cement beneath the tibial tray. The femoral canal was sequentially reamed and broached and trial components were assembled in the femur. Trialing was performed to assess rotation and patellar tracking. A canal plug was placed and the femoral canal was cleaned with a bottle brush followed by pulse lavage. The canal was filled in a retrograde manner using pressurized gentamicin bone cement and final components were cemented in place. SmartSet MV bone cement was used to fix the distal femoral stem extension to host bone. The wound was closed in layers with absorbable sutures. The second day, the drain was removed and the patients started the rehabilitation protocol consisting of continuous passive motion, active exercises and assisted loading with two crutches. All patients started to walk between 2 and 6 d after the surgery using crutches or a four-wheeled walker. All patients except one underwent rehabilitation in a specialized physical medicine unit.
Our cohort was clinically evaluated using numerous scales and indexes including: Visual Analogical Scale (VAS), Oxford Knee Score (OKS), ROM, mobilization and functional autonomy (Barthel’s Index), knee flexion deformity, muscle strength and joint stability. Patients were followed-up in our outpatient clinic at 45 d, 3, 6 and 12 mo and after the last visit a yearly follow-up was executed after a median period of 23 mo.
We also collected data regarding the operative duration, blood transfusions, blood intra-operative losses, type of implant, range of motion, stability, perioperative and postoperative complications, mortality rate at the 1-year follow-up, length of hospital and rehabilitation stays, preoperative ambulatory status and the presence of pre-existent implants or osteosynthesis. In all patients, standard antero-posterior (AP) and lateral x-ray and computed tomography scan of the knee, and subsequently long-leg x-ray, AP and lateral x-rays of the knee, Rosenberg and axial patella x-rays, AP x-ray of the pelvis and frog-leg view were taken after the procedure and at the last follow-up visit.
We also searched for subsidence on the last radiograph. Early non-progressive horizontal radiolucent lines under the tibial component were also analyzed and considered non-significant if < 2 mm. These evaluations were carried out on an AP x-ray of the knee (1, 2 medial zones and 3, 4 lateral zones) and on lateral x-ray of the knee (1, anterior zone and 2, posterior zone)[1]. Location, size, and progression of all radiolucent lines under the femoral component were also assessed on lateral knee x-ray. Location was determined using the Knee Society total knee arthroplasty radiographic evaluation and scoring system[10].
Mean mortality rate was calculated at 30 d and 1 year of follow-up in concordance with the majority of published literature assessing hip fracture mortality. Major and minor complications after surgery were monitored. Major complications included deep infection, pulmonary embolism, neurovascular accident, myocardial infarction, death or removal or revision of the implants. All other complications were considered minor.
A total of eleven patients, 10 women and 1 man, underwent DFR with a fully porous coated metaphyseal sleeve for acute fracture of the distal femur at our institution between 2014 and 2019. The mean age was 87 (range of 85-90 years), no patient died nor was lost to follow-up during the study period. Average BMI was 29.36 (min 24.3, max 35.5), with a slight left sided fractures prevalence (63.3%). Due to the relative older age of our cohort, the prevalent cause of fractures was accidental fall at home (9 patients), while 2 of them were caused by road accidents. The distribution of fractures, according to AO/OTA classification, was the following: 4 patients C1, 3 patients C2, 4 patients C3. Every patient showed radiological evidence of osteoarthritis and a history of knee pain prior to trauma. Furthermore, we noticed a large amount of osteoporosis around the knee despite all patients having a good degree of preoperative functional autonomy. None of the patients used walking aids prior to the accident (Table 1).
| Demographics of the study population | |
| Sex | 10 female; 1 male |
| Mean age in yr | 86 (84-90) |
| BMI | 29.36 (24.3-35.5) |
| Affected side, n (%) | 4 right-sided (36); 7 left-sided (63) |
| ASA score, n (%) | 8 grade II (72); 3 grade III (27) |
| Etiology, n | 2 traffic incidents 9 mechanical falls |
| Classification, n | 4 C1; 3 C2; 4 C3 |
| Type of implant | LPSTMLimb Preservation System De Puy Synthes |
| Prophylactic banding using a 1.7 mm DePuy Synthes trauma cable, n (%) | 7 (63) |
| Preoperative functionality level | All patients walked without walking aids |
| Prior implants/osteosynthesis, n (%) | 2 ipsilateral THA (18), 1 contralateral TKA (9), 1 ipsilateral intramedullary femoral nail (9) |
| Osteoporosis/prior osteoarthritis, n (%) | 11 (100) |
| Follow-up in mo | 23.2 (11-26) |
In our cohort we observed that the majority of patients had a pre-existent orthopaedic implant or osteosynthesis: 2 patients with elective total hip arthroplasty and 1 patient with contralateral TKA, while 1 patient with proximal femoral trochanteric nail ipsilateral to the fractures of the knee. Comorbidities of our cohort of patients are listed in Table 2. Five patients were affected by diabetes (45.5%), while 4 patients suffered from cardiovascular disease (36.4%). Only one patient had a low-grade form of Parkinson syndrome with no impact on his functional autonomy.
| Comorbidities of the patients | |
| Cancer | 0 |
| Diabetes | 5 (45%) |
| Chronic kidney disease | 1 (9%) |
| Steroidal use | 0 |
| Rheumatological disease | 0 |
| Immunosuppressants | 0 |
| Venous insufficiency | 1 (9%) |
| Liver cirrhosis | 0 |
| Cardiopathies | 4 (36%) |
| Neurological conditions | 1 (9%) |
The average hospitalization time in the orthopedic ward was 8.3 d for all patients, except in 2 cases (min 6, max 10) where they were transferred to an orthogeriatric rehabilitation unit. The mean surgical time was 112.9 min (min 96.6, max 130.7). The mean blood intra-operative loss was 280 mL (min 200, max 420); four patients required one blood transfusion, whereas two patients needed two transfusions.
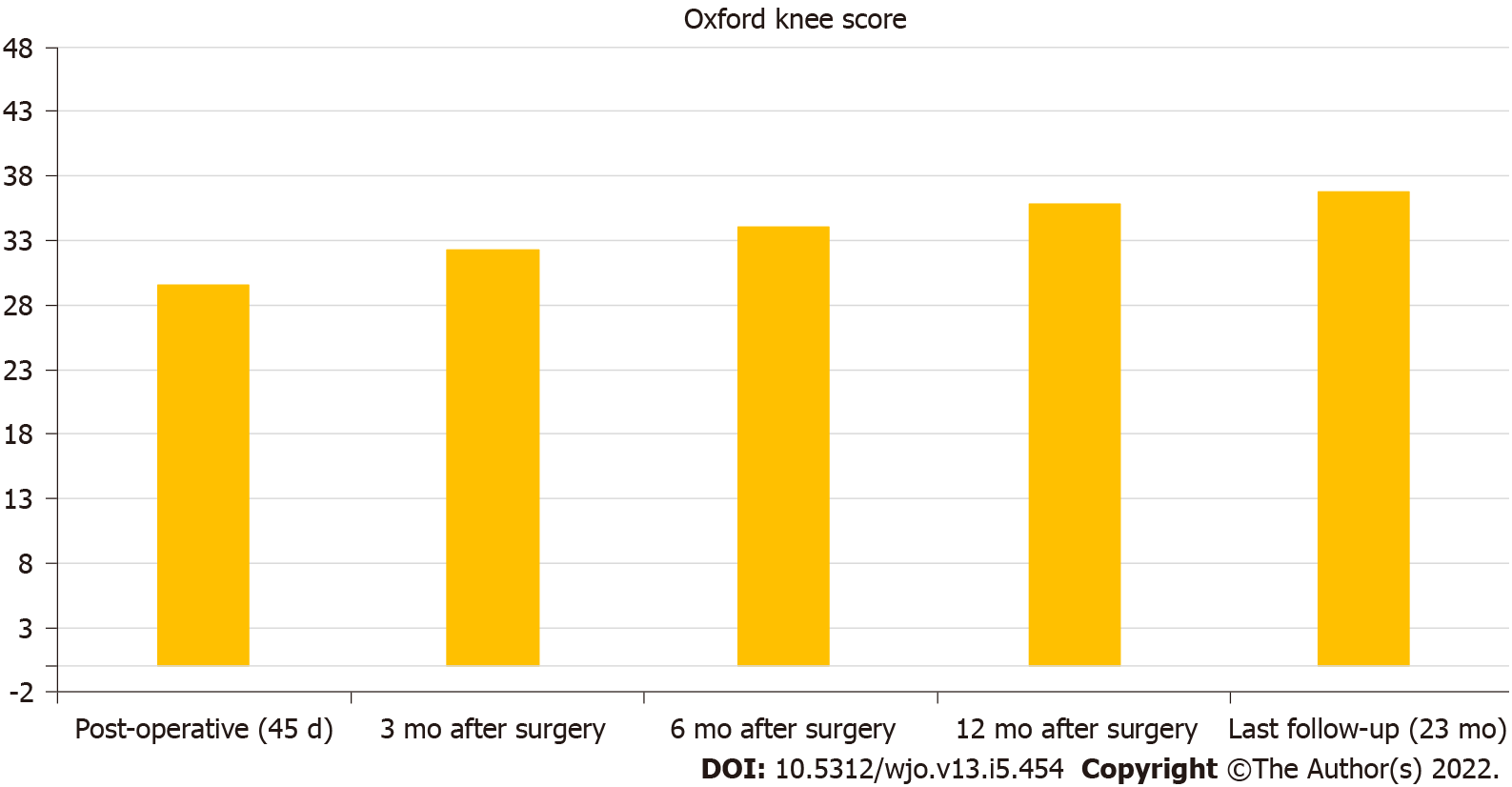
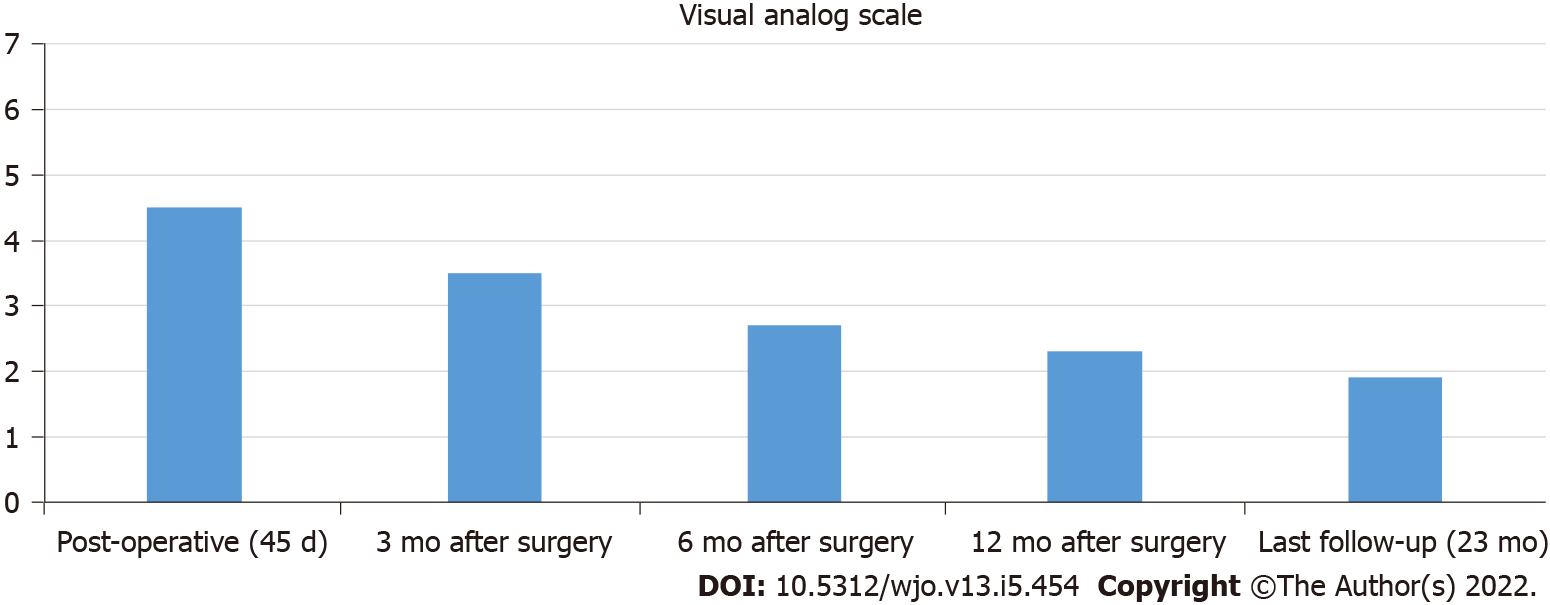
A mild improvement was recorded in the patient's clinical course, pain and quality of life. Using the values of OKS and VAS obtained immediately after surgery and at the last follow-up visit, we observed an improvement in the values of both scales (post-op OKS score 29.5, range 30-43; OKS at 3 mo 32.3 (+9.5%); OKS at 6 mo 34 (+15.2%); OKS at 12 mo 35.8 (+23.3%); OKS at last follow-up 36.8, range 30-43 (+24.8%); post-op VAS 4.5, range 1.5-7.5; VAS at 3 mo 3.5 (-22.2%); VAS at 6 mo 2.7 (-40%); VAS at 12 mo 2.3 (-48.9%); VAS at last follow-up 1.9, range 1.5-7.5 (-57.8%) (Figures 1 and 2). We also used the Barthel Index Score to evaluate the mean functional activity and daily living autonomy score at the time of the last follow-up: 77.3 (range 70-85). At the time of the last follow-up 4 patients could walk without any walking aid (36.4%), 6 patients required a wheeled walker for mobilization (54.5%), and 1 patient used a wheelchair (9.1%). Due to the lack of pre-operative clinical scores, no formal statistical analysis was performed. At the mean follow-up of 23.2 mo, all implants appeared well positioned and osteointegrated with a mean knee score of 34.81 (range 30-41). Mean knee postoperative flexion was 96.2° (range 80-105) and 102° (range 90-106) at the time of last follow-up. No patient showed signs of fixed deformity, extension lag or hyper-extension of the involved leg. In 7 patients, prophylactic cerclage of the femur was needed due to fractures extending to the metadiaphyseal region, with important comminution (C2.1-C2.2; C3.2-C3.3) and a severe grade of osteoporosis requiring a more proximal resection of the distal femur with the use of a longer stem to permit a greater stability of the implant.
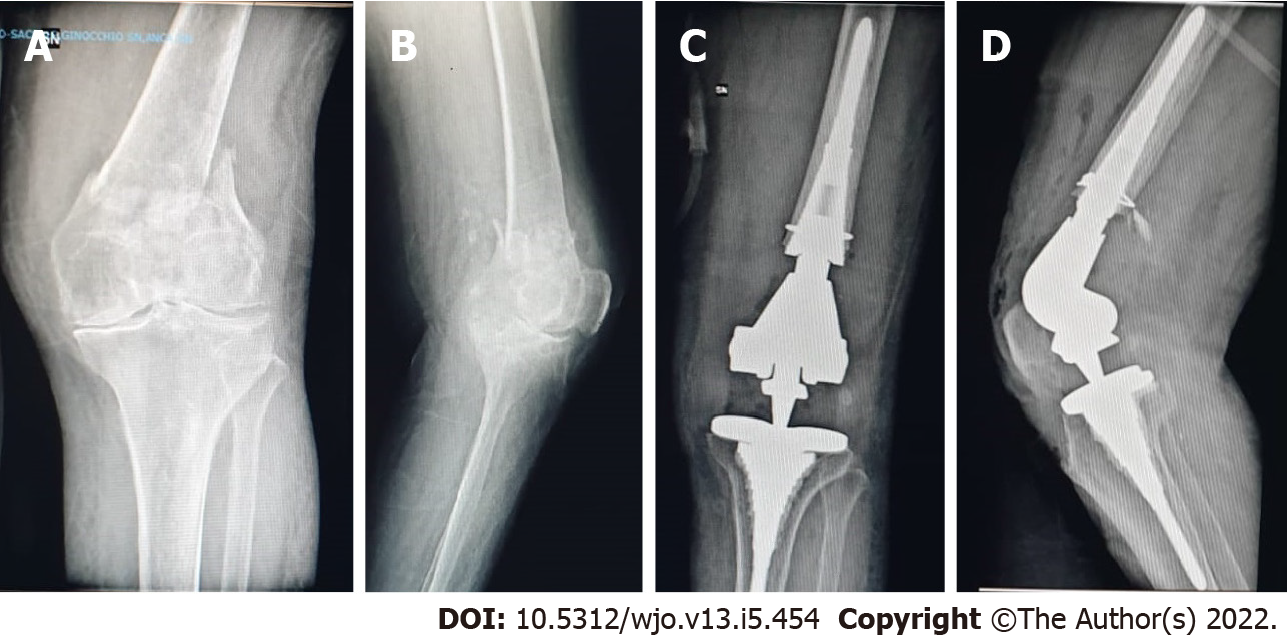
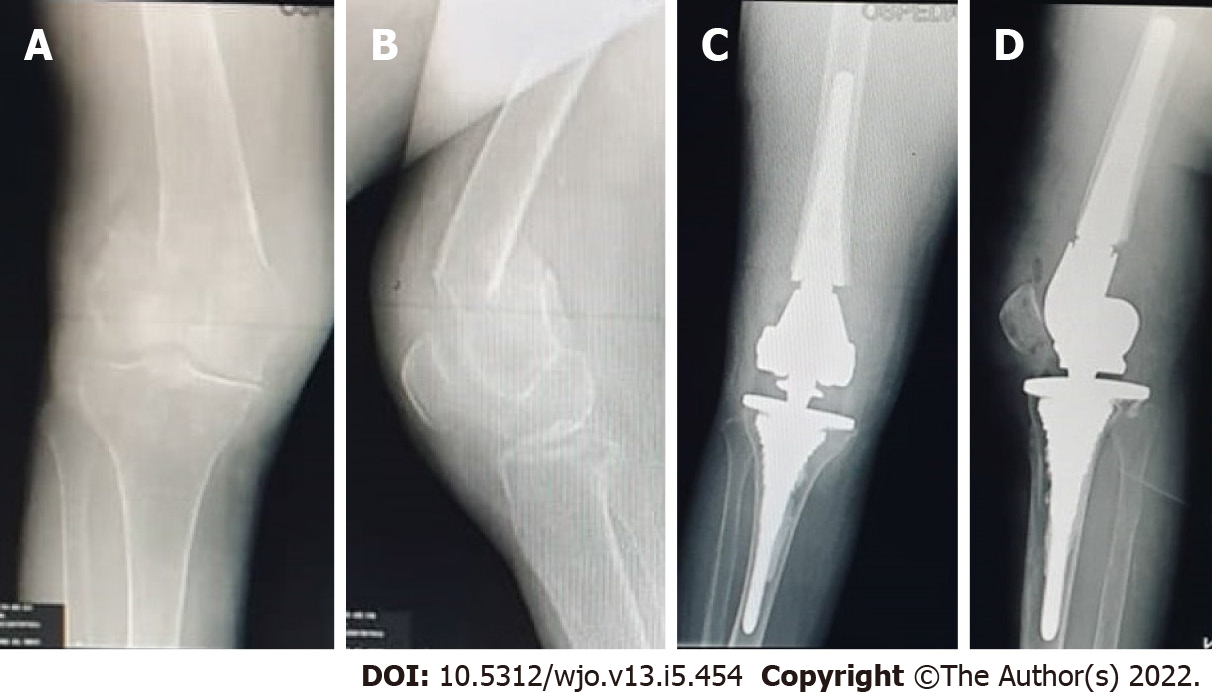
The radiological study showed excellent osteointegration of the cemented femoral stems, according to the criteria of the Knee Society Rating System[11] (Figures 3 and 4). No radiolucent line or osteolysis around the surface of the femoral and tibial stems were observed. There were no signs of angular deformity or malunion. Stress-shielding in zone 6 of the tibial stems was physiologically represented in 60% of the analyzed stems. No progressive axial subsidence > 5 mm was observed. No leg length discrepancy > 1 cm was observed. There was, however, a suspected radiolucent line under the tibial (zone 3) in 4 patients but < 1 mm and 1 patient < 2 mm, but both were not progressive. The measurements performed on the radiographs showed a good restoration of the joint geometry of the knee. There were no major or minor peri-operative complications. No revisions were needed during the follow-up period (Table 3).
| Operative data and observed complications | |
| OR time in min | 112.9 (96.6-130.7) |
| Blood loss in mL | 280 (200-420) |
| Blood transfusion, n (%) | 1 (9) |
| 1-yr mortality rate (for every cause), n (%) | 0 (0) |
| Length of stay in d | 8.3 (6-10) |
| Postoperative ROM in degrees | 96 (80-105) at 3 mo |
| 102 (90-106) at 2 yr | |
| Functional autonomy at 1 yr (Barthel Index) | 77.3 (70-85) |
| 6 patients using a walker | |
| 1 patients using a wheelchair | |
| 4 patients walking without any walking aid | |
| Early (< 1 mo) post-operative complications, n | 0 |
| Late (> 1 mo) post-operative complications, n | 4 patients with radiolucent lines < 1 mm |
| 1 patient with radiolucent lines < 2 mm | |
Prosthetic surgery is one of the greatest achievements of orthopaedics of the last century. Clinical results are excellent in the medium and long term. In addition, the research for better materials has improved the safety and reliability of the implants. In the late decades, an important topic has been debated in international literature: synthesis vs arthroplasty as a treatment of choice to be used in the lateral fractures of the proximal femur. Multi-fragmentary fractures burdened by intrinsic instability, poor bone quality and associated comorbidities that require early recovery, are the elements that tip the scale in favor of arthroplasty. The same thought process was used regarding fractures of the distal femur. Fracture patterns that are difficult to classify (fracture pattern AO/OTA 33C), osteoporosis and important associated degenerative changes (osteoarthritis) and advanced age, are the elements that led the choice towards the use of prosthetics. Metaphyseal comminution complicates the reconstruction of the native alignment and a solid fixation is extremely difficult to achieve and consequently often leads to malunion and/or non-union. Similarly, severe osteoporosis and profound condylar destruction can cause inadequate reduction, secondary loss of reduction and osteosynthesis failure with implant cut-out due to the poor bone stock[12-15]. For these reasons, in elderly, arthroplasty might be the first choice of treatment in case of complete destruction of the distal femur and/or the proximal tibia.
In our study, all patients were over the age of 85 and suffered from supracondylar or intercondylar displaced femoral fractures. All patients had a diagnosis of osteoporosis and a certain grade of pre-existing knee osteoarthritis. A cemented femoral stem with porous coated Metaphyseal Sleeve was used in every patient because of the complex and unstable fracture patterns, the fragile osteoporotic bone, the lack of pre-existent implant (except 1 patient with proximal ipsilateral femoral osteosynthesis) and the low BMI of our population. This allowed reaching the main objective of DFR: The early restoration of a stable limb which guaranteed early mobilization or transfers, depending on the previous level of mobility. The use of a megaprosthesis satisfies both of these requirements.
Mega-implants were originally designed to meet the needs of cancer surgery after extensive resections of bone segments[16]. Over the years, large resection prostheses have been used both in trauma surgery for complex fractures and periarticular pseudarthrosis and in revision surgery[17-19]. The modern modular mega-implants have replaced monoliths, while making the surgical technique simpler and more versatile. Recently, several authors documented that in selected patients, this procedure is better than arthroplasty secondary to failure of open reduction and internal fixation, and shows excellent results and great patient-satisfaction. However, there have been limited reports regarding the use of arthroplasty with mega-prostheses in the acute setting for distal femoral fractures in the elderly and all of them are small retrospective case studies.
The most pivotal paper was published by Appleton et al[20] in 2006. The authors analyzed a population of 52 patients, aged between 55 and 98, who underwent a primary cemented hinged total knee replacement for distal femoral fracture with a metaphyseal extension and reported a 1-year mortality rate of 41%[21,22], a revision rate of 13.6% and an implant survival rate of 4.6% at 1 year. Similar results were obtained by Rosen et al[9] with a 1-year implant survival rate of 100% and a 71% rate of return to the pre-operative ambulation capacities in a cohort of 24 patients with non-union fractures of the distal femur.
Our study showed better results in terms of mortality as compared to what it is found in the literature, with a low 1-year mortality rate (0%). This can be explained by our study population which had few comorbidities, only 3 out of 11 patients with an American Society of Anesthesiologists (ASA) level 3, and the fact that all the patients had a favorable family history and a good level of mobility prior to the intervention. Streubel et al[23] observed a 23% mortality rate following distal (native) and proximal femoral fractures. Similarly, Boureau et al[24] found a 1-year mortality rate of 14% because the studied population included 62% of patients with an ASA score of 3.
In our study, all surgeries were performed by the same surgeon, leading to a standardization of the technique. Our results are comparable with those found in the literature. The most important parameters we have taken into consideration are: blood loss and related transfusions, surgical time, functional and radiographical results, hospitalization time and complications. Regarding blood loss, we had an average Hbg loss of 2.8 g/dL (280 mL). Wang et al[7] reported a mean Hgb loss of 3.8 g/dL (380 mL). In our series we observed lower blood transfusion rates of 9.9% (1 unit of blood transfused postoperatively) than those observed by Pearse et al[25] (24%) (2.5 units of blood transfused postoperatively). On the other hand, Wang et al[7] did not mention blood transfusions in their study.
In terms of functional results, we evaluated our population using validated questionnaires during the follow-up period at 45 d, 3, 6, 12, and 18 mo after surgery (VAS, OKS) and assessed the ROM. Our results were slightly inferior in terms of short-term ROM and 1-year post-operative mobility (Barthel Index) than those reported by Parratte et al[26]. The functional results reported by Sarzaeem et al[14] and Boureau et al[24] were not comparable because of the use of different clinical scores (Knee society score, Parker score, Tegner activity scale).
These studies conclusions have some limitations: data was retrospectively collected from a registry, so there could be coding errors; procedures were performed by different surgeons with different levels of experience, directly influencing the results. A total of 30 patients with proximal tibial fractures who underwent knee replacements using different implants were analyzed. Our operative times were higher than those reported by Pearse et al[25] (112.9 min for our study against 97 min) but lower than those reported by Rosen et al[9] (170 min).
In terms of average hospital stay, our average stay was of 8.3 d (not including orthogeriatric and rehabilitation unit), against 11 d in the study by Bettin et al[4] and 15 d for Appleton et al[20] No major or minor complications were recorded in our study. The French Hip and Knee Society multicenter series of TKA reported 1 death from cardiovascular etiology (major complications) and 3 patients with deep vein thrombosis, including 1 complicated by a pulmonary embolism[26].
The results further confirm that major complications are predominant in patients over the age of 75, which underlines the need for a geriatric oriented-management[12,26]. In addition, Parratte et al[26] found a revision rate of 11.5%, similar to the one found by Boureau et al[24] at 9.5%. However, both of these results seemed inferior than patients treated by osteosynthesis for this type of fracture. Radiolucent lines, based on the radiographic and Hospital for Special Surgery Knee Score, on the femoral side were not seen while they were found on the tibial side in 4 patients with < 1 radiolucent line and 1 patient with less than 2. Our imaging results analyses revealed favorable outcomes and all knee implants were stable.
Our study shows that this surgical procedure is equally safe and effective. In fact, hospitalization times and intra-operative blood losses were not higher than expected and the surgical procedure was well tolerated by patients. This last data is relevant because it shows that if performed by an experienced surgeon, distal femoral replacement can be done rapidly without increasing the risk of malrotation, implant instability, infections and blood loss. The excellent osteointegration of the implants and the absence of revisions, albeit limited by our short follow-up, demonstrate that DFR surgery is safe and effective. Our case series is certainly more recent because it goes from 2015 to 2020 and it is clear that surgical techniques and perioperative management of patients have changed during the years. For example, the use of tranexamic acid and blood loss recovery protocol has limited the intraoperative need for transfusions. The implementation of an outpatient physiotherapy protocol has encouraged early discharge: two patients did not undergo inpatient rehabilitation and were directly discharged.
The authors believe that the most important factors determining the success of DFR is the possibility of immediate unrestricted weight-bearing, intensive physical rehabilitation and early discharge[27]. A stable and quickly cemented fixation with megaprosthesis is indeed an undemanding technique in elderly, osteoporotic, low-demand or sedentary patients which allows a rapid mobilization and prevents prolonged bed rest[28].
This study has several limitations: the small size of the study group, the type of retrospective series and the biases created by it, the inhomogeneous etiology and multiple missing data (anthropometrics data, surgery related factor, no pre-operative functional scores). Furthermore, we noticed other clear limitations: the extreme age of our patients, disfavoring long-term follow-up, the absence of a control group and the short follow-up period. Nevertheless, our data are still one of the most recent and largest cohorts available in the literature.
In the osteoporotic elderly patient with severe arthritis, DFR using a fully porous coated Metaphyseal Sleeve for acute fractures of the distal femur can be a valid option. However, this type of surgery should only be performed in centers specializing in prosthetic hip and knee revision and failure surgery[29]. It is important to note that in order to achieve the best functional outcomes it is necessary to operate on only carefully selected patients and as quickly as possible. Carefully selected patients have a higher chance of prolonged implant survival because of a diminished risk of non-union, implant failure, mal-union and infection, especially in the absence of an ipsilateral total hip arthroplasty.
In conclusion, complex fractures of the distal femur in elderly osteoporotic patients treated with megaprosthesis have shown good functional outcomes and low complication rates similar to other studies with a short-term follow-up. We recommend this procedure in selected patients without relevant comorbidities. Patient selection is of paramount importance and parameters to consider include: age (with age > 90 being a contraindication), comorbidities, ASA score, good previous functional status, physical-mental compliance and the absence of an ipsilateral implant. Acute distal femoral replacement surgery of the knee can reduce the length of hospital stays, hospitalization-related complications and costs. However, in order to achieve statistically relevant evidence, more randomized controlled studies are needed.
Treatment of complex distal femur fractures in the elderly is debated. Currently available techniques (i.e. retrograde nailing, plate and screws fixation, delayed knee replacement surgery) are plagued by poor outcomes. More recently, megaprosthesis have been used for treatment of major trauma and their use has been investigated in treatment of distal femur fractures as well.
There is a lack of short to long term outcomes studies on the use of megaprosthesis for treatment of complex distal femur fractures in the elderly.
The aim of this study is to critically review our clinical experience with usage of megaprosthesis for treatment of complex distal femur fractures in a series of 11 elderly patients.
We conducted a retrospective review of 11 consecutive patients older than 85-years-old for treatment with knee megaprosthesis at our institution. Patients were followed-up on an average for 23 mo after surgery. Clinical and radiographical outcome measures were assessed. Mortality was also recorded.
No deaths were recorded in our case series. At the time of the last follow-up all patients were walking either independently or with walking aids. The average Oxford Knee Score at the time of the last follow-up was 36.8 points. The average Visual Analogical Scale score at the time of the last follow-up was 1.9 points.
Knee megaprosthesis in the setting of complex distal femur fractures in elderly patients is a valid solution which is able to offer short operative times and hospital stays.
Longer follow-up studies will be needed to further validate our results. Furthermore, case-controlled studies (i.e. magaprosthesis vs standard plate fixation) would be useful to compare clinical outcomes between these two techniques.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Velázquez-Saornil J, Spain; Widmer KH, Switzerland S-Editor: Zhang H L-Editor: Filipodia CL P-Editor: Zhang H
| 1. | Loosen A, Fritz Y, Dietrich M. Surgical Treatment of Distal Femur Fractures in Geriatric Patients. Geriatr Orthop Surg Rehabil. 2019;10:2151459319860723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Larsen P, Ceccotti AA, Elsoe R. High mortality following distal femur fractures: a cohort study including three hundred and two distal femur fractures. Int Orthop. 2020;44:173-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Myers P, Laboe P, Johnson KJ, Fredericks PD, Crichlow RJ, Maar DC, Weber TG. Patient Mortality in Geriatric Distal Femur Fractures. J Orthop Trauma. 2018;32:111-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 4. | Bettin CC, Weinlein JC, Toy PC, Heck RK. Distal Femoral Replacement for Acute Distal Femoral Fractures in Elderly Patients. J Orthop Trauma. 2016;30:503-509. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Hake ME, Davis ME, Perdue AM, Goulet JA. Modern Implant Options for the Treatment of Distal Femur Fractures. J Am Acad Orthop Surg. 2019;27:e867-e875. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Tampere T, Ollivier M, Jacquet C, Fabre-Aubrespy M, Parratte S. Knee arthroplasty for acute fractures around the knee. EFORT Open Rev. 2020;5:713-723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Wang W, Yang K, Yang P, Song D, Wang C, Song J, Li X, Wang K. Primary total knee arthroplasty for complex supracondylar femoral fractures in patients with knee arthritis: A retrospective study of a patient cohort. Medicine (Baltimore). 2018;97:e12700. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474:1886-1893. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 680] [Cited by in F6Publishing: 599] [Article Influence: 74.9] [Reference Citation Analysis (0)] |
| 9. | Rosen AL, Strauss E. Primary total knee arthroplasty for complex distal femur fractures in elderly patients. Clin Orthop Relat Res. 2004;101-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Huddleston JI, Wiley JW, Scott RD. Zone 4 femoral radiolucent lines in hybrid vs cemented total knee arthroplasties: are they clinically significant? Clin Orthop Relat Res. 2005;441:334-339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;9-12. [PubMed] [Cited in This Article: ] |
| 12. | Bohm ER, Tufescu TV, Marsh JP. The operative management of osteoporotic fractures of the knee: to fix or replace? J Bone Joint Surg Br. 2012;94:1160-1169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Campana V, Ciolli G, Cazzato G, Giovannetti De Sanctis E, Vitiello C, Leone A, Liuzza F, Maccauro G. Treatment of distal femur fractures with VA-LCP condylar plate: A single trauma centre experience. Injury. 2020;51 Suppl 3:S39-S44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Sarzaeem MM, Omidian MM, Kazemian G, Manafi A. Acute Primary Total Knee Arthroplasty for Proximal Tibial Fractures in Elderly. Arch Bone Jt Surg. 2017;5:302-307. [PubMed] [Cited in This Article: ] |
| 15. | Caliogna L, Medetti M, Bina V, Brancato AM, Castelli A, Jannelli E, Ivone A, Gastaldi G, Annunziata S, Mosconi M, Pasta G. Pulsed Electromagnetic Fields in Bone Healing: Molecular Pathways and Clinical Applications. Int J Mol Sci. 2021;22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Donati F, Di Giacomo G, D'Adamio S, Ziranu A, Careri S, Rosa M, Maccauro G. Silver-Coated Hip Megaprosthesis in Oncological Limb Savage Surgery. Biomed Res Int. 2016;2016:9079041. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Parvizi J, Tarity TD, Slenker N, Wade F, Trappler R, Hozack WJ, Sim FH. Proximal femoral replacement in patients with non-neoplastic conditions. J Bone Joint Surg Am. 2007;89:1036-1043. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Perticarini L, Rossi SMP, Fioruzzi A, Jannelli E, Mosconi M, Benazzo F. Modular tapered conical revision stem in hip revision surgery: mid- term results. BMC Musculoskelet Disord. 2021;22:29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Rossi SMP, Ivone A, Ghiara M, Jannelli E, Sangaletti R, Perticarini L, Benazzo F. A ligament tensor-guided extramedullary alignment technique for distal femoral cut in total knee replacement: results at a minimum 3 years follow-up. Arch Orthop Trauma Surg. 2021;141:2295-2302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Appleton P, Moran M, Houshian S, Robinson CM. Distal femoral fractures treated by hinged total knee replacement in elderly patients. J Bone Joint Surg Br. 2006;88:1065-1070. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87:483-489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 310] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 22. | Shortt NL, Robinson CM. Mortality after low-energy fractures in patients aged at least 45 years old. J Orthop Trauma. 2005;19:396-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Streubel PN, Ricci WM, Wong A, Gardner MJ. Mortality after distal femur fractures in elderly patients. Clin Orthop Relat Res. 2011;469:1188-1196. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 178] [Cited by in F6Publishing: 171] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 24. | Boureau F, Benad K, Putman S, Dereudre G, Kern G, Chantelot C. Does primary total knee arthroplasty for acute knee joint fracture maintain autonomy in the elderly? Orthop Traumatol Surg Res. 2015;101:947-951. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Pearse EO, Klass B, Bendall SP, Railton GT. Stanmore total knee replacement vs internal fixation for supracondylar fractures of the distal femur in elderly patients. Injury. 2005;36:163-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Parratte S, Ollivier M, Argenson JN. Primary total knee arthroplasty for acute fracture around the knee. Orthop Traumatol Surg Res. 2018;104:S71-S80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Bell KM, Johnstone AJ, Court-Brown CM, Hughes SP. Primary knee arthroplasty for distal femoral fractures in elderly patients. J Bone Joint Surg Br. 1992;74:400-402. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 64] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Oliva MS, Vitiello R, Cauteruccio M, Pesare E, Rovere G, Meschini C, Liuzza F, Maccauro G, Ziranu A. Cemented versus cementless megaprosthesis in proximal femur metastatic disease: A systematic review. Orthop Rev (Pavia). 2020;12:8689. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Ebied A, Zayda A, Marei S, Elsayed H. Medium term results of total knee arthroplasty as a primary treatment for knee fractures. SICOT J. 2018;4:6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |