Published online Jan 18, 2021. doi: 10.5312/wjo.v12.i1.24
Peer-review started: October 18, 2020
First decision: November 18, 2020
Revised: December 2, 2020
Accepted: December 16, 2020
Article in press: December 16, 2020
Published online: January 18, 2021
The coronavirus disease 2019 (COVID-19) pandemic has resulted in seismic changes in healthcare delivery. As a result of this, hospital footfall required to be reduced due to increased risk of transmission of infection. To ensure patients can safely access healthcare, we introduced orthopaedic clinic telephone consultations in our busy district general hospital.
To investigate patients’ and clinicians’ perspective of telephone consultations during COVID-19, and whether this method of consultation could be a viable option in the post- pandemic future.
This is a single centre, prospective study conducted in a busy National Health Service district general hospital. In May 2020, 100 non- consecutive adult patients were contacted by independent investigators within 48 h of their orthopaedic clinic telephone consultation to complete a telephone satisfaction questionnaire. The questions assessed satisfaction regarding various aspects of the consultation including overall satisfaction and willingness to use this approach long term. Satisfaction and perspective of 25 clinicians conducting these telephone consultations was also assessed via an online survey tool.
93% of patients were overall satisfied with telephone consultations and 79% were willing to continue this method of consultation post- pandemic. Patients found telephone consultations to reduce personal cost and inconvenience associated with attending a hospital appointment. 72% of clinicians reported overall satisfaction with this service and 80% agreed that telephone consultations should be used in the future. The majority found it less laborious in time and administration in comparison to face to face consultations. Patients and clinicians expressed their desire for video consultations as a method of further improving their experience with remote consultations.
Our study has shown that telephone consultations are a safe and rapid method of adaptation to the COVID-19 pandemic, achieving the aim of reducing hospital footfall. This method of consultation has resulted in immense clinician and patient satisfaction. Our findings suggest that this tool has benefits in post pandemic healthcare delivery. It has also highlighted that telephone consultations can act as a steppingstone to the introduction of the more complex platform of video consulting.
Core Tip: Telephone consultations are a safe and rapid method of adaptation to the coronavirus disease 2019 pandemic, achieving the aim of reducing hospital footfall. This method of consultation has resulted in immense patient and clinician satisfaction, suggesting that this tool has benefits in the post pandemic healthcare delivery. Telephone consultations can also act as a steppingstone to the safe introduction of the more complex platform of video consulting.
- Citation: Vusirikala A, Ensor D, Asokan AK, Lee AJX, Ray R, Tsekes D, Edwin J. Hello, can you hear me? Orthopaedic clinic telephone consultations in the COVID-19 era- a patient and clinician perspective. World J Orthop 2021; 12(1): 24-34
- URL: https://www.wjgnet.com/2218-5836/full/v12/i1/24.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i1.24
Severe acute respiratory syndrome coronavirus disease 2019 (COVID-19) was declared as a pandemic on 11th March 2020 by the World Health Organization and has had a profound effect on trauma and orthopaedic services in the National Health Service (NHS). Public Health England reported the burden of coronavirus in England as 157074 Lab- confirmed cases with 37266 confirmed deaths as of June 15, 2020[1]. In response to the rapidly spreading infection, the UK public were placed in lockdown on March 23, 2020.
The NHS England and NHS Improvement released clinical guidelines in delivering remote consultations in secondary care during the coronavirus pandemic to reduce the transmission of disease[2]. The British Orthopaedic Association also supported a pragmatic approach in dealing with trauma and orthopaedic patients in these extraordinary circumstances advocating conservative management for a wide range of injuries that may have been considered for operative management weeks’ before[3].
Trauma and Orthopaedic clinics are one of the busiest clinical environments with each clinician seeing 15-20 patients on average per clinic session. With the high volume and rapid turnover of patient attendance, running these clinics with appropriate social distancing to reduce spread of infection was deemed challenging. Therefore, our trauma and orthopaedic department set up telephone consultations as a way of rapidly adapting to the new guidance provided to reduce hospital footfall and ensuring to deliver high quality patient care.
In the United Kingdom, telephone consultations are not a new concept and are used for primary care triage and have shown to reduce face to face (F2F) consultations[4,5]. In the last decade, digital health technologies have developed that allow virtual medical consultations such as GP at Hand by Babylon Health that is currently trialled as a virtual GP practise in NHS Hammersmith and Fulham Clinical Commissioning Group[6]. There is a long-term plan for digital services within the NHS in the future[7].
Telemedicine is well established within orthopaedics worldwide, especially useful for clinical management in remote locations. An American hospital followed up their trauma patients remotely when discharged from a level 1 trauma centre with high levels of satisfaction[8]. In elective orthopaedics, telemedicine has been used for elective paediatrics in Australia for their rural population[9] and also in American paediatric fracture management[10]. Post-operative carpal tunnel care has been conducted using telemedicine with good satisfaction and financial savings[11]. One prospective study found no difference in satisfaction between F2F consultations and telemedicine[12]. In the United Kingdom, the virtual fracture clinic is a common form of telemedicine used in orthopaedics, but the pandemic meant that there needed to be a rapid shift to telephone consultations without a pre-existing United Kingdom model to follow.
There are proven positive models of telemedicine consultations, however particularly in orthopaedics, limitations include the inability to carry out a thorough clinical assessment by physically examining a patient. This can be frustrating for both patients and clinicians. The purpose of this study was to assess patients’ and clinicians’ perspective of telephone consultations during COVID-19, and whether this could be a viable option in the post pandemic future.
This is a single centre, prospective study at a busy NHS district general hospital in the United Kingdom. Telephone clinics were rapidly implemented at the start of the pandemic. In May 2020, 100 non- consecutive adult patients were contacted after their orthopaedic clinic telephone consultation by independent investigators (orthopaedic clinic healthcare professionals) and completed a telephone satisfaction questionnaire (Supplementary material 1) within 48 h of the consultation. We contacted new and follow-up patients from fracture and elective clinics across all trauma and orthopaedic subspecialties to avoid selection bias. Inclusion and exclusion criteria are summarised in Table 1.
| Inclusion criteria | Exclusion criteria |
| Adult patients aged ≥ 18 years of age | Patients aged < 18 yr of age |
| Received orthopaedic clinic telephone consultation | If other members of the family responded on patient’s behalf |
| Satisfaction questionnaire completed within 48 h from telephone consultation | Unable to consent to complete satisfaction questionnaire |
| Communication difficulties (verbal or auditory) as stated in patient clinical notes | |
| Cognitive impairment as stated in patient clinical notes | |
| If patients did not answer their telephone on two occasions to complete the satisfaction questionnaire |
These clinics were consultant-led clinics, with additional specialty registrar and core surgical trainee support. To assess suitability for telephone consultations, each patient was screened by a clinician, by reviewing their emergency department notes, or previous clinic letters and imaging. Any patients that required a wound check, plaster cast care or physical examination were deemed unsuitable for a telephone consultation and a F2F appointment was made.
We assessed the satisfaction and perspective of clinicians conducting the telephone consultations via an online questionnaire tool (Supplementary material 1). All clinicians who conducted the telephone consultation were included and were consultant or specialty registrar level.
The questionnaires for both clinicians and patients were designed by the authors and used a Likert scale. The questions aimed to assess satisfaction regarding various aspects of the consultation including overall satisfaction and willingness to use this approach long term. We broke down the telephone consultation into 3 sections and analysed satisfaction with each: (1) Satisfaction with the explanation of patient condition/ injury; (2) Satisfaction with the outcome received from the consultation; and (3) Satisfaction with the answers received to patient questions during the consultation.
Cronbach’s Alpha coefficient of internal consistency was used as a measure of reliability for the results from the Likert scale used for questions 2 to 6 of the patient satisfaction questionnaire. Analysis was performed on SPSS Statistics version 27.
Fisher’s exact test was used to assess differences in the level of patient satisfaction for age, gender and diagnosis of upper/lower limb injuries. A statistically significant level of P < 0.05 was set. Statistical analysis was performed on GraphPad Prism version 8.3.
Telephone satisfaction questionnaires were carried out from May 5, 2020 to May 20, 2020, equating to 12 working days. 23 clinics were held during this time with a total of 262 patients reviewed. Of these, 125 patients (47.7%) had a telephone consultation, and 100 patients were surveyed giving us a capture rate of 80%.
This was compared with the same time period 1 year prior (May 5, 2019 to May 20, 2019) which equated to a total of 10 working days. 36 clinics were held during this time with a total of 617 patients reviewed F2F. There were no telephone consultations taking place within the department prior to the pandemic.
There were 49 males and 51 females, capturing a wide age demographic from 18 to 85+, with the largest cohort (29%) 45-54 years of age. There was a total of 100 injuries in 100 patients. 50% of these were upper limb injuries, 44% lower limb injuries, 1% spine and 5% did not have a diagnosis recorded on the questionnaire.
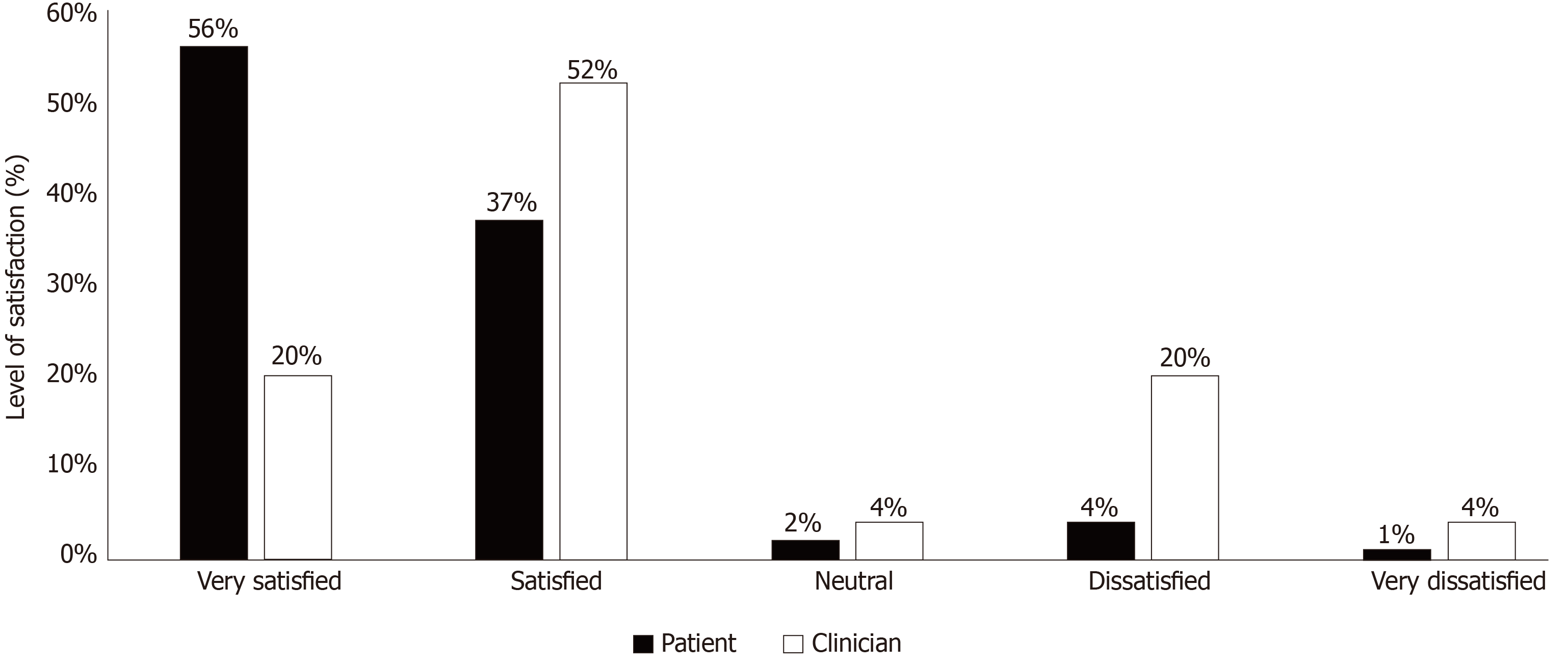
90 out of the 100 patients were happy to be reviewed via telephone consultation. 93% of patients were overall satisfied with telephone consultations with 91% of patients satisfied with the explanation of their condition and answers received to all their questions during the consultation. 79% of the patients were willing to continue this method of consultation in the future. Table 2 is a detailed summary of the level of patient satisfaction with each question. The results of the Likert scale used (very satisfied, satisfied, neutral, dissatisfied and very dissatisfied) for questions 2 to 6 in the patient satisfaction questionnaire revealed satisfactory reliability as shown by Cronbach’s alpha coefficient of internal consistency 0.763.
| Scale | Explanation of condition | Outcome of consultation | Answers received to all questions | Overall satisfaction | Willingness for future telephone consultations |
| Very satisfied | 51 | 47 | 46 | 56 | 44 |
| Satisfied | 40 | 45 | 45 | 37 | 35 |
| Neutral | 6 | 6 | 4 | 2 | 10 |
| Dissatisfied | 3 | 2 | 3 | 4 | 3 |
| Very dissatisfied | 0 | 0 | 2 | 1 | 8 |
Patients had the opportunity to provide free text comments at the end of their questionnaires. Table 3 is a summary of quotations which highlight both positive and negative feedback on telephone consultations. Positive comments were broadly categorized into convenience and efficiency, avoidance of hospital attendance during COVID-19 and mannerisms of the doctors. Negative comments included lack of visual feedback, inability to review images and non-adherence to appointment times.
| Positives | Negatives | ||
| Logistical advantages | A better way to avoid coming to hospital during COVID-19 | Lack of visual feedback | More explanation of X-ray required as I could not see it |
| Good and efficient way to receive results | Video conferencing would be an improvement e.g., Skype/Zoom | ||
| Great service to be seen at home | Prefer F2F to show doctor the deformity | ||
| Telephone consultations made the process quicker than attending the hospital for an appointment | Consultation timings | Was not expecting telephone consultation, a pre-warning text message may have helped | |
| Overall Satisfaction | Very satisfied - doctor really listened and able to ask questions | No specific time given, better to have one hour slots or “window” | |
| Very clear and precise | Patient confidence | Would prefer F2F for first appointment | |
| Doctor was very helpful | Prefer F2F for more support with condition | ||
| Doctor very friendly | Needed to guess whether exercises were being done correctly | ||
| Pleasant doctor | With elderly patients important to advise to have someone accompany them on the telephone call on loudspeaker | ||
We found no statistically significant difference (P < 0.05) in the level of satisfaction between age groups, gender and diagnosis of upper or lower limb injuries (Table 4). There was also no statistically significant difference between willingness for telephone consultations during the current pandemic and willingness for telephone consultations in the future.
| P value (≤ 0.05) | ||||
| Age | Gender | Diagnosis of upper or lower limb injuries | ||
| Question 1 | Willingness for telephone consultation in the current pandemic | 0.31 | 0.32 | > 0.99 |
| Question 2 | Explanation of condition | > 0.99 | 0.09 | 0.25 |
| Question 3 | Outcome of consultation | 0.71 | 0.48 | 0.25 |
| Question 4 | Answers received to all questions | > 0.99 | 0.31 | 0.14 |
| Question 5 | Overall satisfaction | > 0.99 | 0.11 | 0.41 |
| Question 6 | Willingness for future telephone consultations | 0.81 | 0.33 | 0.43 |
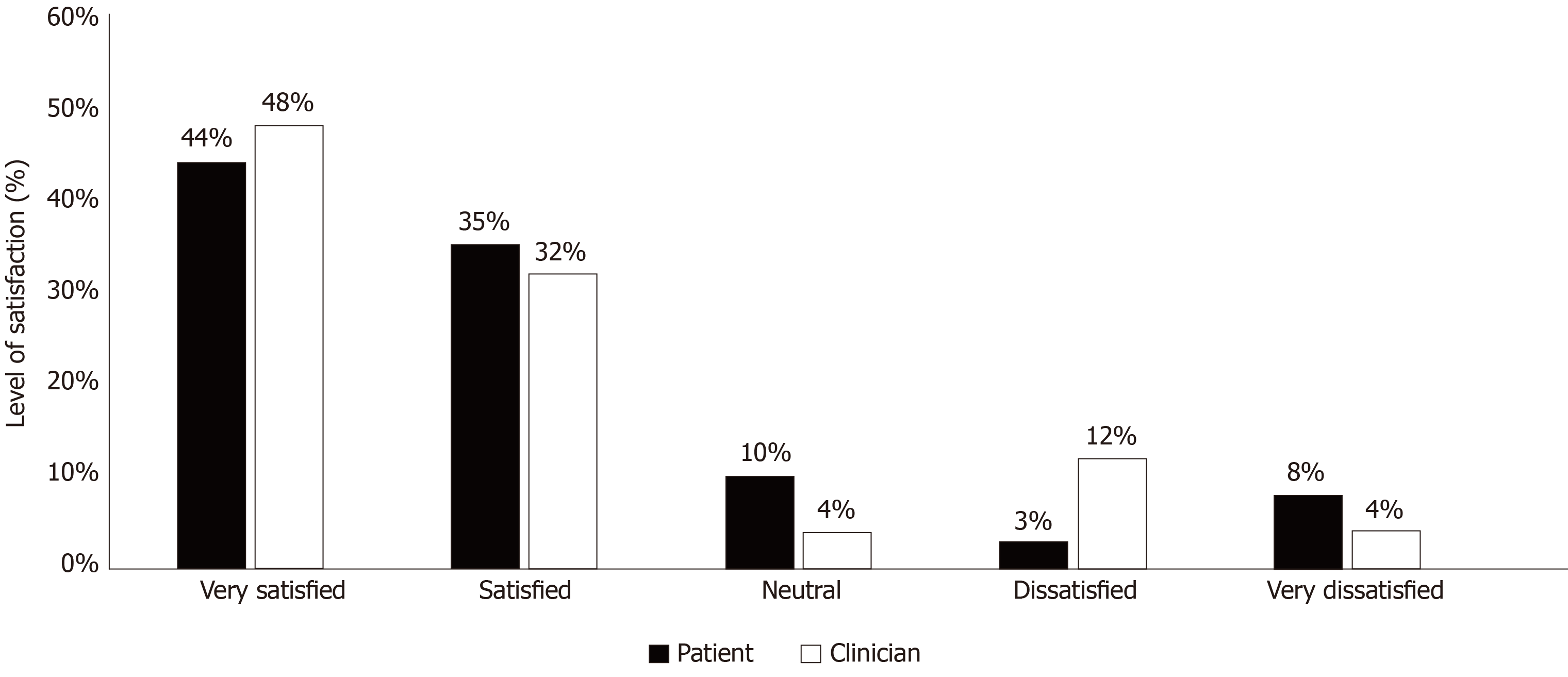
The level of satisfaction of all orthopaedic surgeons carrying out telephone consultations within the department (17 consultants and 8 specialty registrars) was assessed. 72% of clinicians reported overall satisfaction with the use of telephone consultations during the pandemic, with 80% agreeing to continue this method in the future. Figures 1 and 2 compare patient and clinician satisfaction with telephone consultations and their willingness to continue this method of consultation in the future.
Clinicians did not find telephone consultations overly laborious. 80% stated that it took the same amount of time or shorter than traditional face to face consultations and 84% felt telephone consultations required the same or less amount of preparation compared to F2F.
In regard to the effectiveness of telephone consultations, 68% reported them as less comprehensive a medium to F2F consultations. However, the process of explaining the diagnosis and management plan, with subsequent patient questioning fared better. 60% found it the same or easy to explain the diagnosis and management over the telephone and 76% were satisfied with opportunities for patient questions.
Clinicians were also given an opportunity to provide free text suggestions at the end of their questionnaires (Table 5). The overarching suggestions included the need for video consultations which would help with the process of virtual examination, show patients their imaging so as to improve the overall understanding of their condition and subsequent management plan. Additionally, a notable point from a spinal consultant which can be extrapolated across specialties. (“It has to be noted that the public are currently accepting phone consultation as the best available option. This view may change if it carries on for too long. In spine clinics many patients may find it difficult to be convinced that their cases are not suitable for surgical intervention without “hands on” clinic assessment”).
| Suggestions |
| Lack of visual feedback |
| Visual consultations would be a great improvement and improve quality of consultation |
| Video software that will also allow sharing of clinicians’ screen would be more informative as imaging can be shown |
| Workload |
| Dedicated administrator for telephone consultation preparation would be useful |
| Lack of examination |
| Difficult to examine patients. Often reliant on family or patient’s own interpretation of examination |
| Could be limited to follow ups only |
| Difficult to build rapport or trust |
This study investigated patient and clinician satisfaction with orthopaedic clinic telephone consultations. 93% of patients were overall satisfied with telephone consultations. Gilbert et al[13], recently published a quality improvement study which focused on the process involved in the implementation of virtual clinics in response to the COVID-19 pandemic. A secondary outcome from their study assessed patient satisfaction with telephone consultations using a single summative question, which resulted in a mean satisfaction score of 90 out of 100, which was similar to our study findings[13]. From our literature review, no previous United Kingdom based study assessed level of patient satisfaction with the various aspects involved in a telephone consultation. We divided the telephone consultation into 3 sections and analysed satisfaction with each: (1) satisfaction with the explanation of patient condition/ injury; (2) satisfaction with the outcome received from the consultation; and (3) satisfaction with the answers received to patient questions during the consultation. Greater than 90% of patients were satisfied with each of the three areas within the consultation.
79% of patients agreed to future follow ups using this form of telemedicine. Patients felt they were able to obtain the required information from the comfort of their own home, avoiding exposure/spread of COVID-19 and reducing personal cost and inconvenience associated with attending a hospital appointment. In 2014, a study comparing web- based follow up to face to face consultations following joint arthroplasty found that patients in the web-based group incurred lower associated costs[14].
Remote consultations theoretically may be more cost-effective for the NHS. In our department, the average cost per appointment for all trauma and orthopaedic clinics (fracture and elective) are £206 for first time appointment and £165 for follow up appointments[15]. 80% of clinicians in our study found that telephone consultations took the same amount of time or less compared to F2F consultations. Unfortunately, at present, we are unable to comment on the cost-effectiveness of this new telephone consultation service because costing returns are carried out every 3 months. The main cost for an outpatient department is staff payroll. During the pandemic, staff base has not changed because many clinicians were deployed to carry out COVID related duties. Therefore, the base staff cost remained static. Marsh et al[16] in 2014, carried out an economic evaluation of web-based ($98 per patient) compared with in- person follow up ($162 per patient) and showed that service costs were significantly lower in the web-based group[16]. In the near future, if clinicians are back to their normal duties and telephone consultations continue then the average cost per appointment may reduce because more appointments will be carried out per clinician via the telephone and fewer staff may be required to review the same number of patients. This aspect of remote consultations is worthwhile to investigate to ascertain its costing benefits as the NHS is constantly under pressure to provide a cost- effective service but at the same time respond to the rising needs and demands of the population.
72% of clinicians were overall satisfied with telephone consultations. 80% agreed with continuing this method of consultation after the pandemic. Our findings were in contrast with a recent study published in Madrid where only 37.5% of clinicians agreed with continuing telephone consultations in the future because they felt this method of consultation may have limitations for first clinical appointments[17]. Even though our study did not differentiate between first and follow up appointments we had high satisfaction rates to continue this form of telemedicine consultation in the post pandemic era. We recognise that there is a need for further research in identifying the challenges related to first and follow up telephone consultation appointments.
Patients in our study highlighted the importance of clinician punctuality with appointment times. As a new method of consultation, there were wide variations in adherence to appointment times with some clinics being carried out earlier or later than scheduled. In most cases, patients were called by the administrative team in regard to their new date and time of appointment. To ensure future adherence to appointment times and better communication with patients in regard to changes to their appointments a patient text messaging service could be implemented[18].
We are aware that telephone consultations have limitations from both patient and clinician perspectives. They may not be suitable for all conditions but can be a useful tool to stratify risk for each patient. It will help identify those who can be provided advice over the telephone and signposted to resources online. But it will also help identify a clinical situation that necessitates a face to face consultation.
Both patients and clinicians report a lack of visual feedback with telephone consultations. Patients were frustrated that they were unable to visually demonstrate areas of pain or deformity and they could not confirm whether the rehabilitation exercises given to them were being carried out correctly. They also expressed wishes to be able to view their imaging to have a better understanding of their condition. These concerns were also echoed by the clinicians in our study. 68% felt that telephone consultations were not as comprehensive as face to face consultations and this may be due to the inability to examine the patient, review images with patients to explain their conditions and subsequent management in more detail.
Telephone consultations require a very different skill set in comparison to F2F consultations. Clinicians carrying out telephone consultations may adequately assess patients but inadequately reassure them due to the lack of visual cues. This may mean that clinicians may need to quickly adapt specific skills for effective telephone consultations.
In our study, due to the rapid implementation of telephone consultations, clinicians did not receive any formal training, yet, 91% of patients were satisfied with the explanation of their condition and 91% found that all their questions were appropriately answered during the consultation. A number of articles have been published providing guidance on effective telephone consultations, which have also stressed the importance of accurate documentation and stated that clinic letters that are normally sent to GPs should also be sent to patients to reinforce what was discussed and avoid misunderstandings[19,20]. It would be beneficial to review these articles by those carrying out this form of consultation.
Both patients and clinicians in our study suggested the need for video consultations to further improve their experience with remote consultations. A systematic review by Gilbert et al[21] in 2018, showed that patients preferred video consultations to telephone because they had visual feedback from their clinician. This increased their confidence with the information received during the consultation thus increasing their adherence to the medical advice given. They also found video consultations useful for those who have difficulty with verbal descriptions, and it was a good medium to receive rehabilitation as their exercises can be shown to them[21].
Video consultations can help overcome many challenges associated with telephone consultations. But it is important to recognise that implementation of a video consulting platform is a complex process which is resource heavy and requires the involvement of both national and local strategic leads[22]. The execution of a video consultation service requires a team of experts to install new software, adequately train clinicians and administration staff, set up videoconferencing programmes and equipment in patient’s homes and be available for any technical issues that may occur. This process is difficult, requiring a lot of planning and if implemented at speed, service failure may occur.
During our study period in the midst of the pandemic, the number of trauma and orthopaedic clinics held was 1.5 times less (23 clinics vs 36 clinics) and the volume of patients reviewed in these clinics was approximately twice as less compared to the same time period in 2019 (262 patients vs 617 patients). The reduction in the volume of patients in our clinics is likely a reflection of a change in people’s behaviour in response to COVID-19 and the nationwide lockdown. It would be important to assess whether satisfaction levels of telephone consultations amongst our patients remain high when we revert back to running clinics at the pre- pandemic capacity as there would be increased time pressure amongst the clinicians.
Due to the unforeseen circumstances of the COVID-19 pandemic, we had to introduce a safe alternative to F2F consultations quickly. Telephone consultations were easy to implement rapidly in a department with no pre-existing remote consultation model. They were found to be an acceptable method of communication irrespective of age, gender and diagnosis. A similar finding was found in a study carried out at 5 GP practises in South Yorkshire in the United Kingdom[23].
Telephone consultations act as a steppingstone to the introduction of the more complex platform of video consulting. Our department is currently in the process of introducing a video consultation service in a planned and safe manner to ensure a more effective and interactive healthcare service delivery to our patients in the post pandemic future.
This study has several strengths. Firstly, it has shown that telephone consultations have been well received by both clinicians and patients across all ages. Patients had high satisfaction with the opportunity to discuss their condition and have had all their questions answered to an acceptable standard. Telephone consultations have shown to be a safe and quick adaptation to the pandemic, achieving the aim of reducing hospital footfall. This study has also identified the need to further improve remote consultations by introducing video consultation services.
The rapid implementation of this method of remote consultation service within our department has resulted in this study having limitations. We were unable to put our patient and clinician questionnaires through the validation process, but we used a validated Likert scale[24] to assess satisfaction to reduce measurement error and we demonstrated satisfactory reliability of the results obtained as shown by Cronbach’s alpha coefficient. Due to the time critical nature of this study, we were unable to compare satisfaction levels of telephone consultations with F2F consultations and we did not differentiate between first time and follow up clinic appointments, even though overall satisfaction amongst our patients was high. Our clinicians did not receive any specific training prior to carrying out telephone consultations but patients were satisfied with the information provided and subsequent management as a result of these consultations.
We are aware that telemedicine is not a novel approach in trauma and orthopaedics, but our study is a snapshot of patient and clinician satisfaction with the rapid implementation of telephone consultations in the midst of a pandemic. We understand that more detailed work needs to be completed to analyse the effectiveness and acceptability of telephone consultations as a form of safe healthcare delivery in the long term. But for now, it has proved an effective alternative in providing high quality healthcare during these unprecedented times.
The coronavirus disease 2019 (COVID-19) pandemic resulted in seismic changes in healthcare delivery. Due to the high transmission risk of this infection, hospital footfall required to be reduced rapidly. Trauma and Orthopaedic clinics are one of the busiest clinical environments with high volume and rapid turnover of patient attendance. Running these clinics with appropriate social distancing to reduce the spread of infection was deemed challenging. To ensure patients can continue to safely access healthcare, we introduced orthopaedic clinic telephone consultations within our department in a busy district general hospital in England.
Telephone consultations were rapidly implemented within a department with no pre-existing remote consultation model in order to adapt to the COVID-19 pandemic. But in order to ensure patients received high quality care it was vital to obtain patient and clinician satisfaction with this method of remote consultation.
This study aimed to investigate patient and clinician perspective of telephone consultations during the COVID-19 pandemic, and whether this method of remote consultation could be a viable option in the post- pandemic future.
This is a single centre, prospective study conducted in a busy National Health Service district general hospital. 100 non- consecutive adult patients were contacted within 48 h of their telephone consultation to complete a patient satisfaction questionnaire which assessed satisfaction with various aspects of the consultation including willingness to continue this method of consultation in the long term. Clinician perspective and satisfaction with conducting these telephone consultations was also sought.
93% of patients were overall satisfied with telephone consultations and 79% were willing to continue this method of consultation post- pandemic. Patients found telephone consultations to reduce personal cost and inconvenience associated with attending a hospital appointment. 72% of clinicians reported overall satisfaction with this service and 80% agreed that telephone consultations should be used in the future. The majority found it less laborious in time and administration in comparison to face to face consultations. There was no statistically significant difference (P < 0.05) in the level of satisfaction between age groups, gender and diagnosis of upper or lower limb injuries. There was also no statistically significant difference between willingness for telephone consultations during the current pandemic and willingness for telephone consultations in the future.
This study has proved that telephone consultations are an effective alternative that can be implemented rapidly to provide high quality healthcare during these unprecedented times. This method of consultation has resulted in immense clinician and patient satisfaction. Our findings suggest that this tool has benefits in the post-pandemic healthcare delivery.
Although the number of patients and clinicians included was relatively small, this study provided a snapshot of patient and clinician satisfaction with the rapid implementation of telephone consultations, achieving the aim of reducing hospital footfall in response to the COVID-19 pandemic. It also highlighted the need to further improve patient experience of remote consultations with the safe and planned introduction of the more complex platform of video consultation services.
The authors would like to thank the Trauma and Orthopaedic clinical staff who helped with data collection.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Camacho S S-Editor: Zhang L L-Editor: A P-Editor: Xing YX
| 1. | UK Government. Coronavirus (COVID-19) in the UK. Available from: https://coronavirus.data.gov.uk/#category=nations&map=case. [Cited in This Article: ] |
| 2. | NHS England and NHS Improvement. Clinical guide for the management of remote consultations and remote working in secondary care during the coronavirus pandemic. Available from: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0044-Specialty-Guide-Virtual-Working-and-Coronavirus-27-March-20.pdf. [Cited in This Article: ] |
| 3. | British Orthopaedic Association. BOAST- Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available from: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html. [Cited in This Article: ] |
| 4. | Newbould J, Abel G, Ball S, Corbett J, Elliott M, Exley J, Martin A, Saunders C, Wilson E, Winpenny E, Yang M, Roland M. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ. 2017;358:j4197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Miller D, Loftus AM, O'Boyle PJ, McCloskey M, O'Kelly J, Mace D, McKeon N, Ewan SL, Moore L, Abbott A, Cunning S, McCarron MO, Paget AM. Impact of a telephone-first consultation system in general practice. Postgrad Med J. 2019;95:590-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | NHS England and NHS Improvement London. GP at Hand- Fact Sheet. Available from: https://www.england.nhs.uk/London/our-work/gp-at-hand-fact-sheet/. [Cited in This Article: ] |
| 7. | NHS Long Term Plan. Chapter 5: Digitally- enabled care will go mainstream across the NHS. Available from: https://www.longtermplan.nhs.uk/online-version/chapter-5-digitally-enabled-care-will-go-mainstream-across-the-nhs/. [Cited in This Article: ] |
| 8. | Boulanger B, Kearney P, Ochoa J, Tsuei B, Sands F. Telemedicine: a solution to the followup of rural trauma patients? J Am Coll Surg. 2001;192:447-452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Rowell PD, Pincus P, White M, Smith AC. Telehealth in paediatric orthopaedic surgery in Queensland: a 10-year review. ANZ J Surg. 2014;84:955-959. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Sinha N, Cornell M, Wheatley B, Munley N, Seeley M. Looking Through a Different Lens: Patient Satisfaction With Telemedicine in Delivering Pediatric Fracture Care. J Am Acad Orthop Surg Glob Res Rev. 2019;3:e100. [PubMed] [Cited in This Article: ] |
| 11. | Williams M, Amin A, Getgood A, Hallam P, Chojnowski AJ, Chapman PG. Telephone clinic follow-up following carpal tunnel decompression. J Hand Surg Eur Vol. 2008;33:641-644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29:e139-e145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 139] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 13. | Gilbert AW, Billany JCT, Adam R, Martin L, Tobin R, Bagdai S, Galvin N, Farr I, Allain A, Davies L, Bateson J. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 143] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 14. | Marsh JD, Bryant DM, MacDonald SJ, Naudie DD, McCalden RW, Howard JL, Bourne RB, McAuley JP. Feasibility, effectiveness and costs associated with a web-based follow-up assessment following total joint arthroplasty. J Arthroplasty. 2014;29:1723-1728. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | National Collection Cost Index (NCCI). National Cost Collection for the NHS. Available from: https://improvement.nhs.uk/resources/national-cost-collection/#ncc1819. [Cited in This Article: ] |
| 16. | Marsh J, Hoch JS, Bryant D, MacDonald SJ, Naudie D, McCalden R, Howard J, Bourne R, McAuley J. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2014;96:1910-1916. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Luengo-Alonso G, Pérez-Tabernero FG, Tovar-Bazaga M, Arguello-Cuenca JM, Calvo E. Critical adjustments in a department of orthopaedics through the COVID-19 pandemic. Int Orthop. 2020;44:1557-1564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 18. | Rohman L, Maruswezki D, Boyce Cam N. The impact of a text messaging service on orthopaedic clinic Did Not Attend rates. J Telemed Telecare. 2015;21:408-413. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | van Galen LS, Car J. Telephone consultations. BMJ. 2018;360:k1047. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Iyengar K, El-Nahas W. A brief guide to telephone medical consultation. Br J Health Care Manag. 2020;26:1-3. [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Gilbert AW, Jaggi A, May CR. What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? Physiotherapy. 2018;104:178-186. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ. 2020;368:m998. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 496] [Cited by in F6Publishing: 453] [Article Influence: 113.3] [Reference Citation Analysis (0)] |
| 23. | Jiwa M, Freeman J, Coleman M, Joesbury H. Do older patients feel able to cope with illness following telephone consultations? Curr Med Res Opin. 2005;21:339-344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Likert R. A technique for the measurement of attitudes. New York: The Science Press; 1932. [Cited in This Article: ] |