Published online Feb 18, 2020. doi: 10.5312/wjo.v11.i2.116
Peer-review started: May 23, 2019
First decision: July 31, 2019
Revised: September 19, 2019
Accepted: November 28, 2019
Article in press: November 28, 2019
Published online: February 18, 2020
Processing time: 274 Days and 15.4 Hours
This unique presentation of hip swelling is only the seventh reported case of pseudotumor recurrence in a non-metal-on-metal total hip arthroplasty (THA) construct. The constellation of patient symptoms and laboratory findings contradict the expected elevated serum metal ion levels associated with the formation of pseudotumor. The presentation, lab trends, and imaging findings contribute to the growing base of knowledge surrounding the effects of corrosion in arthroplasty constructs with stem-neck modularity.
A 74-year-old man status post primary THA presented with left hip swelling and elevated serum metal ions five years after implantation of a modular stem-neck prosthesis. The swelling was diagnosed as pseudotumor based on laboratory trends and imaging findings and was treated with revision arthroplasty that completely resolved the initial hip swelling. The patient presented with recurrent hip swelling and recurrent pseudotumor findings on imaging in the same hip four months later. Non-operative management with ultrasound-guided hip aspiration resulted in symptom relief and resolution of the recurrent swelling. After one year of follow-up, the patient had no further recurrences of hip swelling.
This case of post-revision pseudotumor recurrence elucidates attributable patient, surgical, and implant factors with a discussion of diagnostics, management, and prognosis for patients with pseudotumor in non-metal-on-metal arthroplasty constructs.
Core tip: This unique presentation of hip swelling is only the seventh reported case of pseudotumor recurrence in a non-metal-on-metal total hip arthroplasty construct. These patients require a low threshold for clinical evaluation, using multiple modalities such as history, physical exam, magnetic resonance imaging, and serum metal ion level testing. The presentation, lab trends, and imaging findings of this case contribute to the growing base of knowledge surrounding the effects of corrosion in arthroplasty constructs with stem-neck modularity.
- Citation: Desai BR, Sumarriva GE, Chimento GF. Pseudotumor recurrence in a post-revision total hip arthroplasty with stem neck modularity: A case report. World J Orthop 2020; 11(2): 116-122
- URL: https://www.wjgnet.com/2218-5836/full/v11/i2/116.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i2.116
Total hip arthroplasty (THA) yields excellent patient satisfaction and offers improvement in mobility and quality of life[1]. Advancements in technology have shaped prosthesis design to accommodate patient factors, level of activity, and surgical approaches. THA constructs can be composed of three components-the femoral component, acetabular component, and bearing surface. One variation of prosthesis design is modular neck systems, which allow a wide range of intraoperative adjustments of the femoral head, adjustment of leg length, and horizontal femoral offset [2]. Modularity aims to reproduce the natural biomechanics of the hip through the adjustment of individual prosthetic components. Proximal stem-neck modularity includes a junction that can have a double taper subjective to both axial and bending stresses. This stress leads to an uncommon complication known as fretting corrosion[2]. Destruction at contact sites from relative micromotion between two components of the prosthesis can lead to mid-stem failure in modular stem prostheses[2].
Metal-on-metal (MoM) THA is an alternative prosthetic design that was commonly used before unexpected complications led to its disuse. The concept was originally designed with the advantage of increased joint stability and fewer dislocations given a larger surface area for contact. An unforeseen complication of MoM arthroplasty was pseudotumor formation–at rates as high as 59% in studied cohorts[3]. This association has been seen consistently in metal-on metal THA[4]. A study by Ming showed the elapsed time between MoM THA and revision arthroplasty for pseudotumor formation to be 61 mo[5]. In the same study cohort of 97 patients, 3% had post-revision pseudotumor recurrence[5]. Recently, pseudotumor formation has been linked to non-metal-on-metal THA, especially in patients with modular constructs. Based on the literature review conducted by the authors of this report, only seven cases of pseudotumor recurrence have been associated in THA with non-MoM modular constructs[5,6].
The authors of this paper present a case of post-revision pseudotumor recurrence in a THA with a modular femoral component. The patient was informed that data concerning the case would be submitted for publication, and patient consent was obtained. Table 1 outlines a timeline of the patient presentation.
| Timeline | Patient situation |
| February 2012 | Past medical history: Degenerative osteoarthritis; Underwent left total hip arthroplasty |
| November 2017 | Initial presentation for left hip swelling; Fluid collection seen on magnetic resonance imaging |
| December 2017 | Treated with revision total hip arthroplasty; Immediate resolution of pseudotumor post-revision |
| March 2018 | Recurrent left hip swelling; Resolution after repeat magnetic resonance imaging and joint aspiration |
| March 2019 | After 1-yr of follow-up no further hip swelling recurrences or pain symptoms |
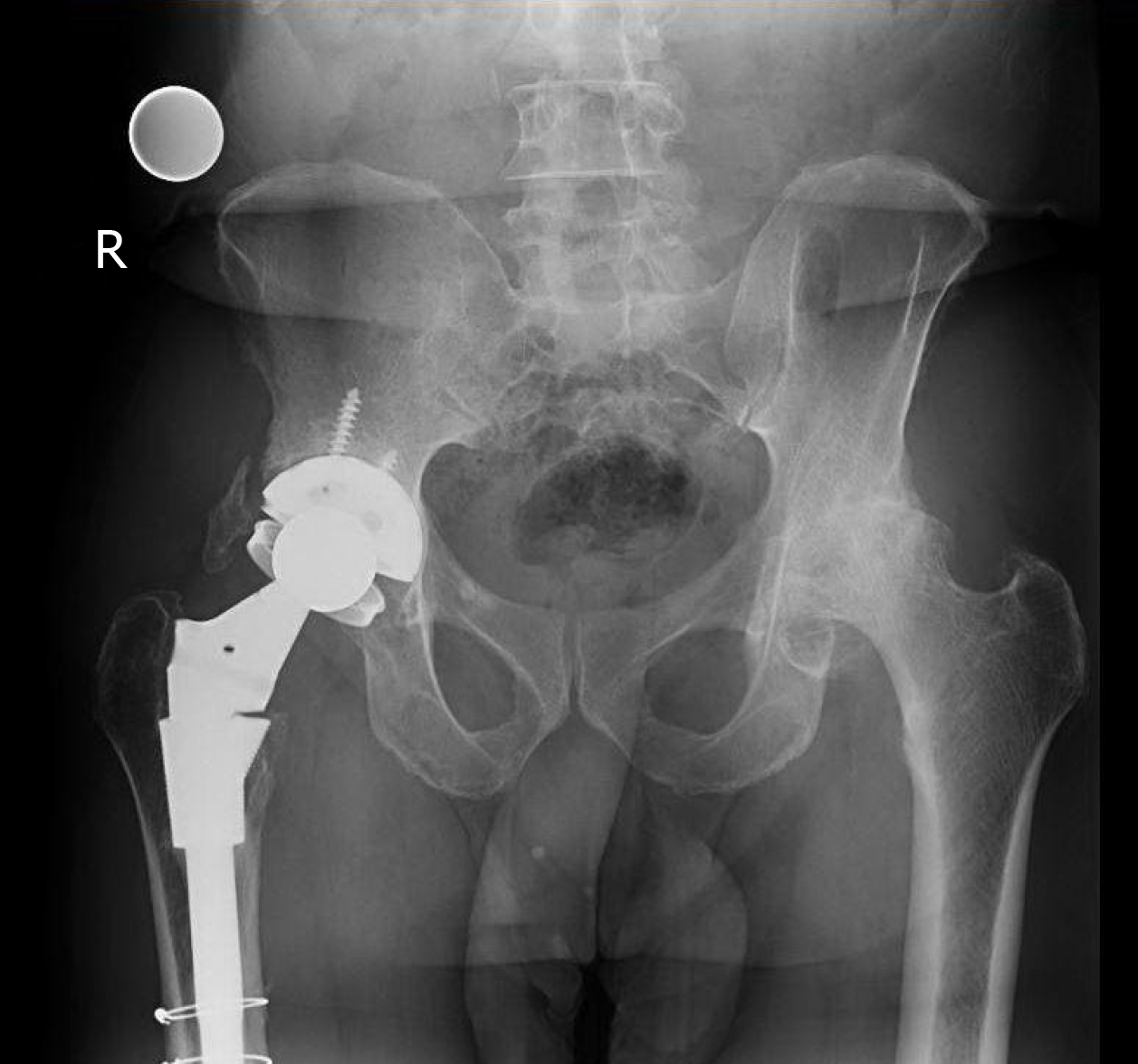
A 74-year-old African-American male was referred to the senior author on the orthopedic joint service with left hip swelling and pain more than five years after THA (Figures 1 and 2). The patient presented with a one-month history of left hip swelling. Associated symptoms included discomfort with movement, decreased range of motion, and left lower extremity swelling. There was no recent history of trauma and the left limb was neurovascular-intact.
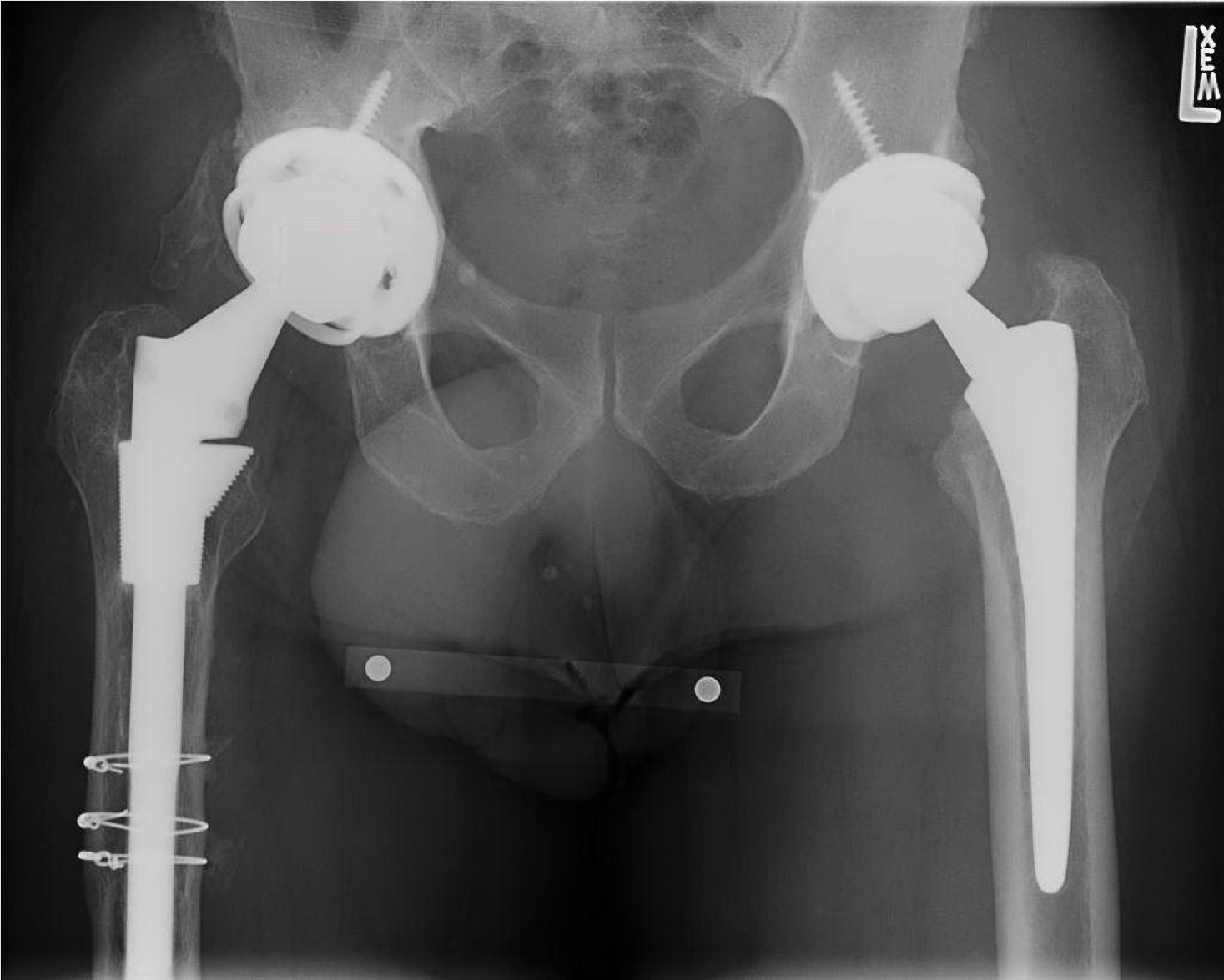
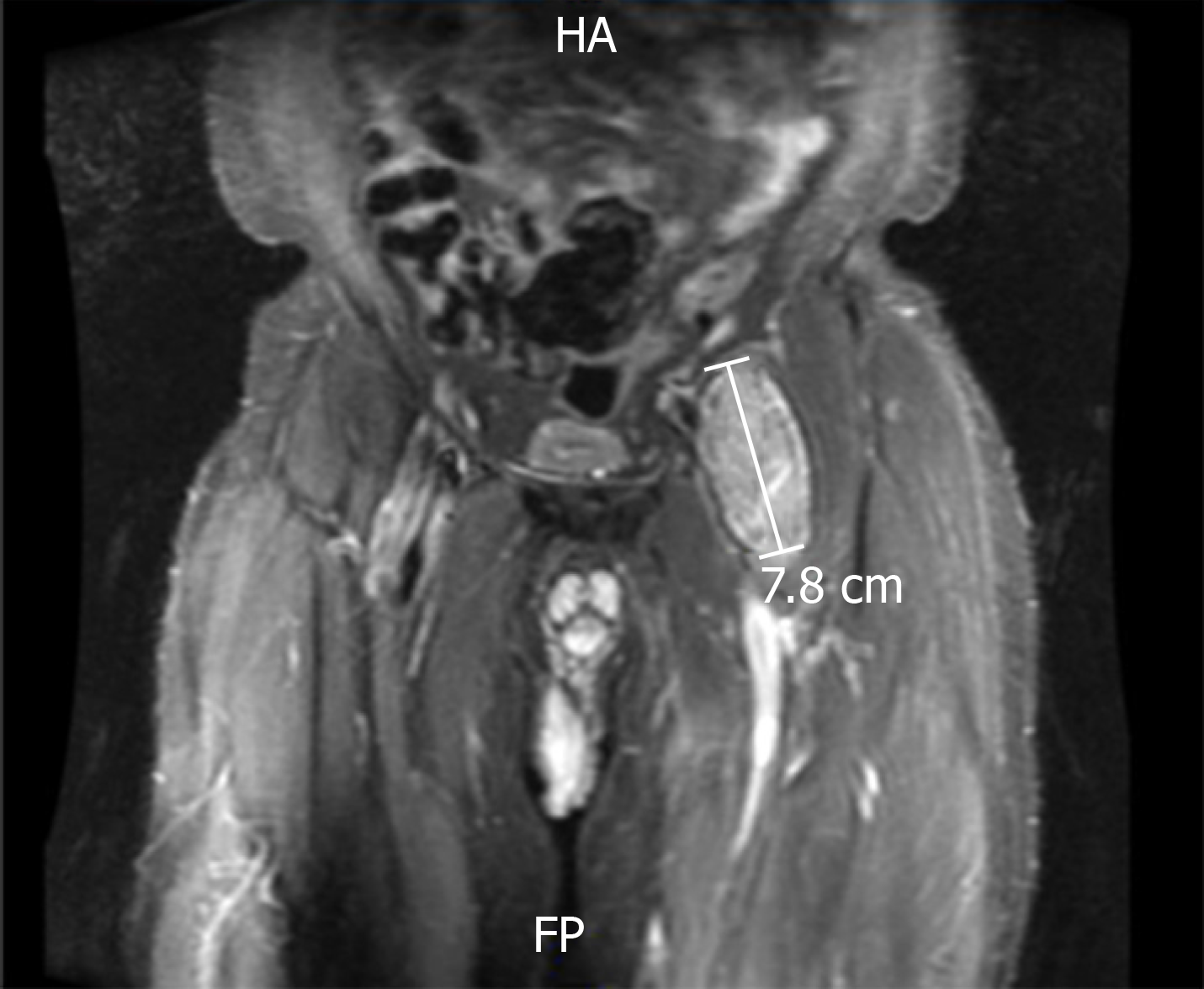
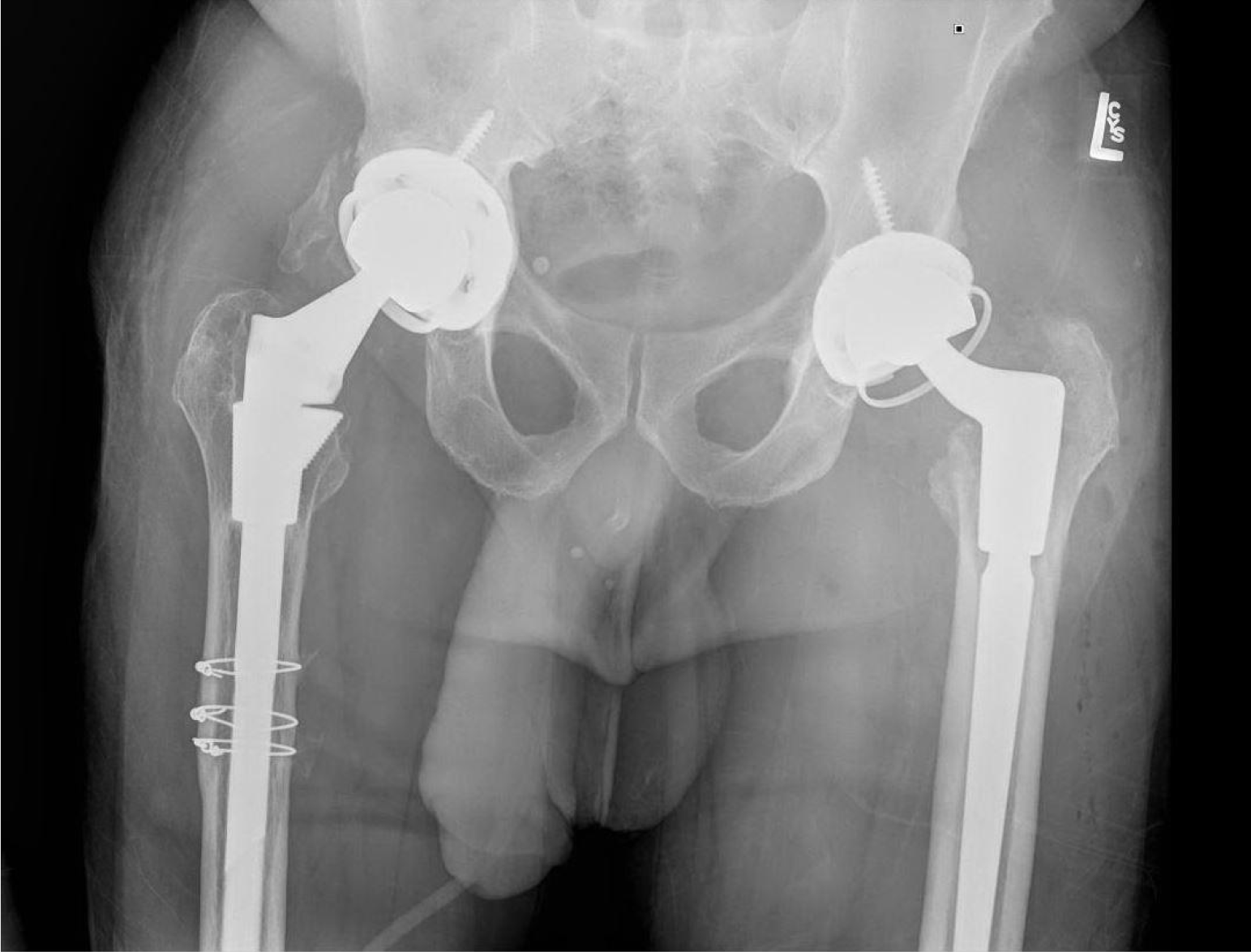
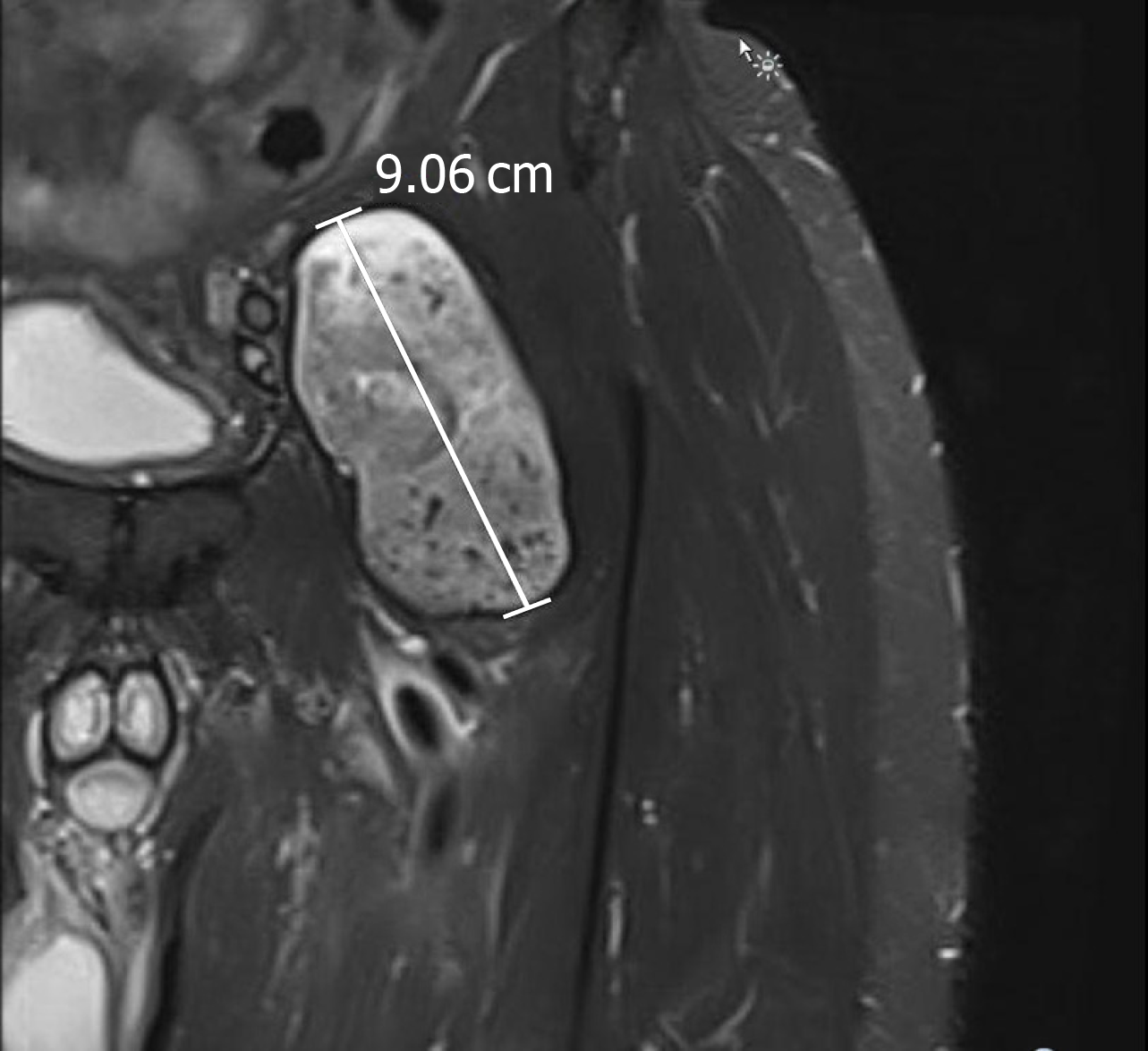
The patient presented with left hip swelling and was evaluated with physical exam and imaging. Magnetic resonance imaging (MRI) showed a well-defined complex lesion anterior to the left hip prosthesis (Figure 3) and a septated simple fluid collection posterior to the left hip prosthesis; further evaluation revealed elevated serum metal ion levels-serum cobalt 12 ng/mL (ref. range 0.0-0.9 ng/mL) and serum chromium 2.8 ng/mL (ref. range < 0.3 ng/mL) The lesion was first unsuccessfully managed with aspiration by interventional radiology. After continued discomfort and signs of component loosening on imaging, the patient opted for with revision arthroplasty. During revision, the initial incision was used to resect necrotic soft tissue and drain a large blood-tinged fluid collection in the articular space. The collected tissue was sent for culture and pathology, which showed fibrin and fibrous tissue without the presence of neutrophils. On extraction of the head and neck, there was a significant degree of corrosion along the mid-portion and body of the neck. The acetabular component was well-fixed and in good condition to accommodate a new constrained liner. The revision was completed by extracting the proximal segment of the femoral stem and replacing it with an 18 mm × 155 mm modular stem, a 25-mm neutral proximal body, and 28 mm neutral femoral head. The new components were firmly seated, demonstrating stability and no impingement on range of motion. At two-week follow-up patient was ambulating well with a cane with no acute post-operative complications (Figure 4).
The patient presented again four months post-revision with a two-week history of recurrent left hip swelling. A new lesion was noted on MRI in a location similar to the initial lesion (Figure 5). Serum metal ion levels at this time had returned to baseline (serum cobalt = 1.5 ng/mL; serum chromium = 1.4 ng/mL). Ultrasound-guided fine needle aspiration of the lesion yielded 15cc of clotted blood, resembling the aspiration findings of the initial lesion suggesting adverse local tissue reaction (ALTR) recurrence.
The patient’s only notable past medical history was hypertension well-controlled on medication.
New pseudotumor formation in a location similar to the initial lesion was noted on MRI. Serum metal ion levels were elevated above the normal range, but significantly lower than on initial presentation for pseudotumor formation (serum cobalt = 1.5 ng/mL; serum chromium = 1.4 ng/mL).
MRI at time of initial presentation showed a well-defined complex lesion anterior to the left hip prosthesis and a septate simple fluid collection posterior to the left hip prosthesis. Repeat MRI at recurrence confirmed a similar lesion larger in size at the same location.
The final diagnosis of the presented case is post-revision ALTR recurrence.
An ultrasound-guided hip aspiration provided symptomatic relief and resolution of hip swelling.
At clinical follow-up 18 mo post-revision there were no radiographic signs of implant loosening and the patient reported no further episodes of hip swelling with satisfactory return to baseline mobility.
The goal of prosthetic modularity is to offer intraoperative adjustments to manage leg length, anteversion, and offset to better replicate natural hip biomechanics[7]. Dual modularity refers to arthroplasty construct components (head, neck, and stem) that may be interchanged, specifically at the proximal portion where the head-neck and neck-stem junctions are located. Modularity at the head-neck junction was originally designed to allow movements in different planes and to reduce friction and wear[2]. However, the additional junctions pose complications such as fracture, corrosion, fretting, dissociation, and cold-welding[8]. The specific concern of fretting and crevice corrosion is a known association established in modular constructs[9]. Micromotion at the neck-stem junction from natural bending movements can predispose components to fretting corrosion and metal debris deposition[9].
Pseudotumor is a term historically associated with metal-on-metal arthroplasty implants. However, with the growing recognition that cystic masses causing pain, pressure effects, bone and soft-tissue destruction can be associated with implants of different bearings and degrees of modularity, the literature has adapted new terms such as asymptomatic lymphocytic vasculitis-associated lesions based on histological findings and the more encompassing term ALTR. A recent systematic review of pseudotumors suggested an incidence ranging from 1% up to 6% of all hip THAs[4]. These pseudotumors are neither infective nor neoplastic and have been proposed to occur secondary to excessive wear debris, foreign body reaction, metal hypersensitivity, and certain patient/surgical-related factors[6].
One commonly suggested etiology of ALTRs is metal ion deposition generated by mechanical wear and surface corrosion at modular junctions[10]. Fretting is a relative oscillatory tangential movement of small amplitude which can occur between contacting surfaces of two immobile and fixed object[11]. In presence of body fluids, fretting can be accompanied by corrosive effects. The presence of water within human tissues initiates a repassivation reaction, where the exposed metal surface forms an oxide and releases hydrogen ions. Negatively charged chloride ions migrate to balance these positively charged hydrogen ions, producing hydrochloric acid, which dissolves metal alloys. The resulting corrosion debris generated from the modular junction appears responsible for ALTR[11].
Looking further at instances of pseudotumor recurrence, a study by Kwon looked at 40 revisions after the presence of symptomatic ALTR diagnosed on metal artifact reduction sequence MRI with elevated metal ion levels[6]. These patients all had metal-on-polyethylene bearings on titanium alloy femoral stems so there was only one site of modularity at the head-neck junction. They used the Goldberg criteria to assess fretting and corrosion and found that three-quarters of the patients had Grade 3 tissue damage and metal debris at the femoral component’s trunnion neck taper[6]. They were revised to a ceramic femoral head with a titanium adaptor sleeve over the femoral stem trunnion. In the patient that experienced recurrence, there was no linear correlation to post-revision serum metal ion levels. Rather they suggested that pre-revision MRI findings of lesions with abductor deficiency and intra-operative tissue damage should be stronger predictive factors for post-revision complications such as pseudotumor recurrence[6].
Thus, it would lead us to believe that with an increase in the number of modular junctions, there exists an increased propensity for fretting corrosion and an increased incidence of ALTRs. Several recent studies looking at revision outcomes in THA with dual modularity suggest exactly this[5,8-11]. The benefits of dual modularity are clear, it provides greater flexibility and facilitates the adjustment of leg length, femoral anteversion, and offset in order to accurately reproduce the center of rotation of the hip. However, both axial and bending stresses at the stem-neck junction strongly influence fretting corrosion eventually leading to mechanical failure of the modular neck and the subsequent need for revision.
Kwon looked at outcomes after revision dual taper THA in about 200 patients with symptomatic ALTR due to taper corrosion[6]. A staggering 20% of the cohort experienced post-revision complications. 3% of those patients experienced pseudotumor recurrence. 5 of the patients were revised to a cemented monoblock femoral stem with a ceramic head, so recurrence may be less likely attributable to stem-neck modularity or head-neck taper corrosion. The authors attributed recurrence to surgical, patient, and implant factors. They hypothesized that incomplete surgical debridement and inadequate removal of pseudotumor can contribute. However, extensive debridement needs to be performed with preservation of nearby neurovascular structures.
The uniqueness of this case report is highlighted by the post-revision ALTR recurrence. Previously reported cases of stem-neck modularity leading to pseudotumor formation exhibited implant damage between two metal components[12]. This lends to the notion that micromotion between adjoining metal-on-metal components are susceptible to the same corrosion and metal ion deposition seen in MoM arthroplasty. In order for this mechanism to be true however, one would expect more cases of pseudotumor formation given the number of THAs performed yearly using stem-neck modularity.
Current recommendations in symptomatic patients with ALTRs suggest avoiding overreliance on any single investigative tool in the clinical decision-making process for revision surgery[13]. There should be a low threshold for clinical evaluation, especially in patients dual modularity THA. A combination approach has been recommended by the consensus statement between the American Association of Hip and Knee Surgeons, American Academy of Orthopaedic Surgeons, and Hip Society in regards to managing symptomatic patients with dual modular THA. The recommendation states “And in patients where revision in indicated, knowledge of the pre-revision risk factors we talked about earlier can mitigate the incidence of complications and need for re-revision.”
This case highlights a post-revision pseudotumor recurrence in a modular femoral stem THA not utilizing metal-on-metal prostheses. This article aims to elucidate patient, surgical, and implant factors that may contribute to pseudotumor recurrence with a discussion of diagnostics, management, and prognosis.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papachristou G S-Editor: Wang J L-Editor: A E-Editor: Liu MY
| 1. | Ritter MA, Albohm MJ. Overview: maintaining outcomes for total hip arthroplasty. The past, present, and future. Clin Orthop Relat Res. 1997;81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Krishnan H, Krishnan SP, Blunn G, Skinner JA, Hart AJ. Modular neck femoral stems. Bone Joint J. 2013;95-B:1011-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Hart AJ, Satchithananda K, Liddle AD, Sabah SA, McRobbie D, Henckel J, Cobb JP, Skinner JA, Mitchell AW. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional computed tomography and magnetic resonance imaging. J Bone Joint Surg Am. 2012;94:317-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 218] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 4. | Daniel J, Holland J, Quigley L, Sprague S, Bhandari M. Pseudotumors associated with total hip arthroplasty. J Bone Joint Surg Am. 2012;94:86-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Dimitriou D, Liow MH, Tsai TY, Leone WA, Li G, Kwon YM. Early Outcomes of Revision Surgery for Taper Corrosion of Dual Taper Total Hip Arthroplasty in 187 Patients. J Arthroplasty. 2016;31:1549-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Kwon YM, Rossi D, MacAuliffe J, Peng Y, Arauz P. Risk Factors Associated With Early Complications of Revision Surgery for Head-Neck Taper Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty. 2018;33:3231-3237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2012;41:422-426. [PubMed] |
| 8. | Kop AM, Swarts E. Corrosion of a hip stem with a modular neck taper junction: a retrieval study of 16 cases. J Arthroplasty. 2009;24:1019-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 157] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 9. | Canham CD, Muradov PI, Simpson JB, Incavo SJ. Corrosion and adverse local tissue reaction after total hip arthroplasty with a modular titanium alloy femoral neck. Arthroplast Today. 2017;3:211-214. [PubMed] [DOI] [Full Text] |
| 10. | De Martino I, Assini JB, Elpers ME, Wright TM, Westrich GH. Corrosion and Fretting of a Modular Hip System: A Retrieval Analysis of 60 Rejuvenate Stems. J Arthroplasty. 2015;30:1470-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Baxmann M, Jauch SY, Schilling C, Blömer W, Grupp TM, Morlock MM. The influence of contact conditions and micromotions on the fretting behavior of modular titanium alloy taper connections. Med Eng Phys. 2013;35:676-83; discussion 676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Leung P, Kudrna JC. Growth of an intrapelvic pseudotumor associated with a metal-on-metal total hip arthroplasty after revision arthroplasty causing a femoral nerve neuropathy. Arthroplast Today. 2016;2:105-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Kwon YM, Lombardi AV, Jacobs JJ, Fehring TK, Lewis CG, Cabanela ME. Risk stratification algorithm for management of patients with metal-on-metal hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, and the Hip Society. J Bone Joint Surg Am. 2014;96:e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 131] [Article Influence: 11.9] [Reference Citation Analysis (0)] |