Published online Aug 18, 2019. doi: 10.5312/wjo.v10.i8.304
Peer-review started: February 15, 2019
First decision: June 12, 2019
Revised: June 24, 2019
Accepted: July 8, 2019
Article in press: July 8, 2019
Published online: August 18, 2019
Basal joint arthritis is a common disease which is especially present in post-menopausal women. A variety of procedures have been described once conservative treatment has failed. The purpose of our study is to present a novel surgical technique based on a clinical case with three-year follow-up which is highly effective, even after failure of previous procedures.
We present a case of a 39 year-old-woman who suffered from recurring, persistent, sharp left thumb pain for several years. After two operative procedures, she presented again with intolerable, sharp pain over the trapeziometacarpal joint, and wished to proceed with a pain relieving procedure or arthroplasty. Intraoperatively, the articular surfaces appeared well, without any bare areas of bone or eburnation, resulting in the decision to perform a “subtraction hemiarthroplasty”. A shortening osteotomy of the os trapezium was performed by removing a slice of 8-9 mm bone, without damaging the joint cartilages. The osteotomy was stabilized using two screws, the ligament and capsular tissue was suture imbricated, and a cut down on the translation and a dorsal radial ligament reconstruction were performed. Three years after the final procedure, a long-term follow-up demonstrates excellent results, pain free with full range-of-motion.
Subtraction hemiarthroplasty with ligament tightening imbrication and reconstruction of the radial ligament led to excellent results in motion and pain.
Core tip: Even after failure of two index procedures, the subtraction hemiarthroplasty technique with ligament tightening imbrication and reconstruction of the radial ligament can lead to excellent results in both motion and pain. This can be a good alternative to a more aggressive treatment approach, such as arthroplasty, arthrodesis, or hemitrapeziectormy, and should be considered in select patients.
- Citation: Bäcker HC, Freibott CE, Rosenwasser MP. Subtraction hemiarthroplasty in basal joint arthritis: A case report. World J Orthop 2019; 10(8): 304-309
- URL: https://www.wjgnet.com/2218-5836/full/v10/i8/304.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i8.304
Basal joint arthritis is a common problem especially in post-menopausal women, however symptoms are present in a few of these cases[1,2]. The trapeziometacarpal joint is a biconcave saddle joint which enables a variety of movements – flexion, extension, abduction, adduction, pronation, supination and opposition, which is why degenerative diseases may be predisposed. It is stabilized by multiple ligaments, of which the beak and dorsoradial ligament seems to be the most important[3,4]. A weakening of the ligaments may lead to a movement of the point of maximal contact from volar-ulnar to dorsoradial[5]. Because of the complexity of the joint, many different treatments exist, ranging from conservative to operative. In mild symptomatic patients, an analgesic therapy, such as custom-made splinting, physiotherapy or even local intra-artciular steroid injection, may be the treatment of choice. In the event that these techniques fail and the patient still suffers from intolerable pain, an operative treatment may be considered. A standard literature search (PubMed) results in 426 relevant articles. The procedures range from osteotomy, arthrodesis, partial or complete trapeziectomy with or without reconstruction of the ligaments and tendon interposition, to implant arthroplasty, spacers, interposition arthroplasty with resurfacing or joint replacement. Even within the different groups, the types vary tremendously, similar to choosing a prosthesis[3]. According to the review on surgery for thumb osteoarthritis published by Wajon et al[6], no gold standard for treatment currently exists. Within the 11 included and reviewed studies, no procedure demonstrated any superiority in terms of clinical outcome. Additionally, Wajon et al[6] found that no comparable study exists evaluating surgery versus non-surgical interventions.
We present a novel surgical technique based on a clinical case with three-year follow-up which is very effective, even after failed previous procedures.
A 39-year old female and former softball coach presented with persistent thumb pain of her left side since 2008.
An arthroscopy of the left basal joint with debridement of fibrillated cartilage and partial synovectomy was indicated and performed at our institution in May 2012. Intraoperatively, a cartilage damage of up to 25% of the articular surfaces (metacarpal as well as trapezial) was identified. The joint was stable under direct examination and stress testing. In December 2014, she presented again with a complete preservation of the scaphoidtrapezial joint and intolerable sharp, persistent pain at the trapeziometacarpal joint. The maximum peak of pain was localized over the palmar aspect of the joint with progression when pinching and grasping.
The patient underwent a volar plate capsulodesis and stabilization, utilizing a free tendon graft at a different institution in 2008, which brought her approximately 2.5 years of pain relief and a return to previous sport activities. Her typical pain level progressed from a VAS 2 out of 10, to 6 out of 10, with a maximal peak at the basal joint of her thumb. As a result an intra-articular steroid injection was performed leading to a pain relief for few months in 2012.
Clinically, a tenderness could be identified, localized over the trapeziometacarpal joint, with a slight hyperflexibility (5 to 10 degrees of hyperflexion).
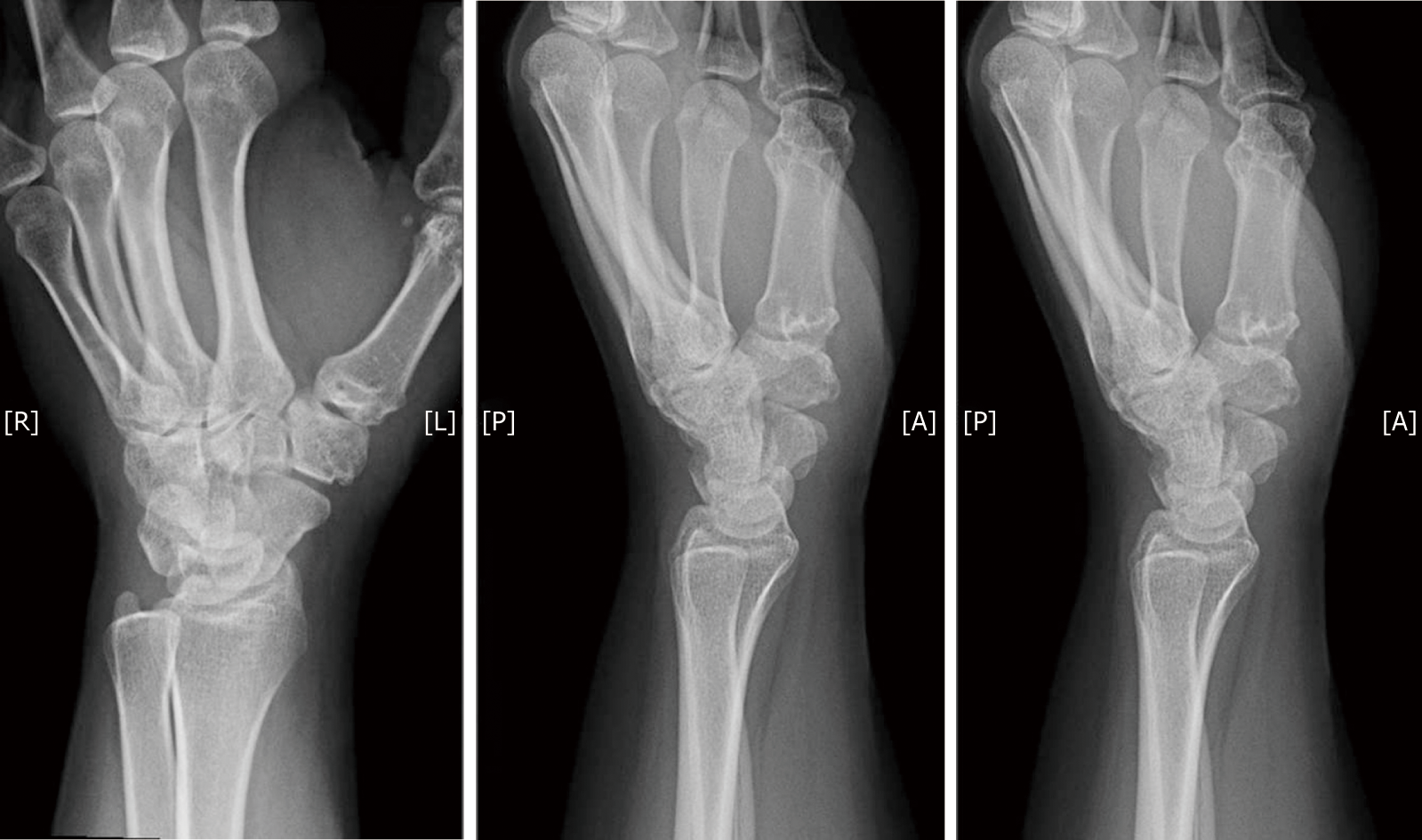
Her radiographs revealed signs of arthrosis, like subchondral sclerosis, and slight joint space narrowing as illustrated in Figure 1.
Because of severe limitations in daily life and in activities, she wished to proceed with a pain relieving procedure. A variety of options were discussed, from arthroplasty, hemiarthroplasty of the trapezium, deletion or shortening of the trapezium to tendon interposition graft and/or soft tissue ligament imbrication with reconstruction, all depending on the intraoperative findings.
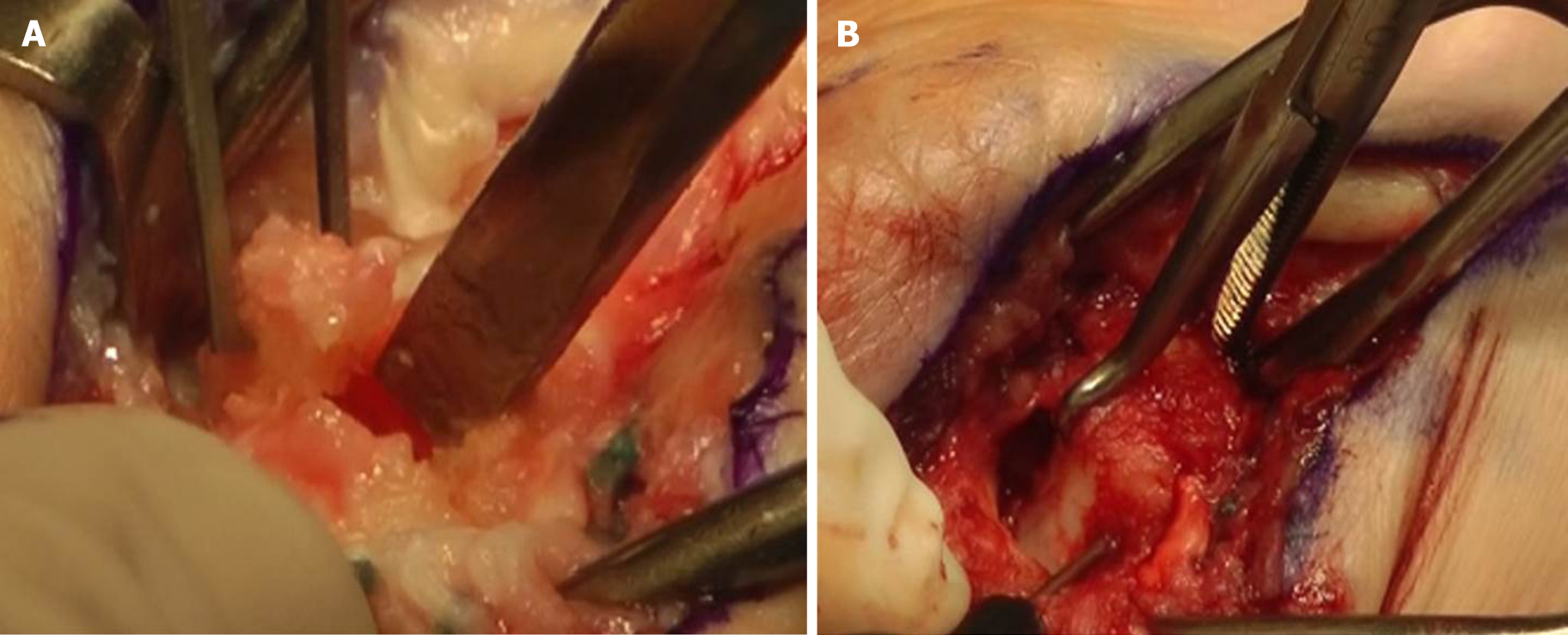
This was an outpatient procedure performed under regional anesthesia – supraclavicular block. The patient was placed in a supine position and the arm placed on a hand table. The left arm was sterilely prepped and draped followed by inflation of the pneumatic tourniquet to 250 mmHg pressure. The previous incision from the Wagner approach[7] was utilized again and extended along the flexor carpi radialis tendon for a few centimeters proximally. The skin flaps, which were still at place without detachment of the metacarpal nor the trapezial attachment, were elevated. The tendon graft of the previously performed reconstruction, as well as numerous non-absorbable sutures, were removed. In the following step, an arthrotomy of the trapeziometacarpal joint was performed and the cartilage was visualized. Even though subchondral sclerosis could be identified in radiographs, the articular surfaces were well-appearing, without any bare areas of bone or eburnation. Therefore, we decided to maintain the articular surfaces by shortening of the central third of the trapezium and then re-transplant and fix the articular surfaces in a contour position against the first metacarpal. To ensure the correct level of osteotomy, image intensifier was utilized. A sagittal saw was used to perform the osteotomy of the os trapezium and remove a slice of approximately 8-9 mm of the bone, without damaging the cartilage. Afterwards, the articular surfaces were readjusted and stabilized using a bone reduction clamp. Two drill holes were created by utilizing a 1.1 mm drill bit, followed by a countersink to allow the 1.5 mm titanium screw heads to be countersunk below the articular surface. The length of the screws was measured to be 9 mm and the titanium screws were placed and tightened. Control under the image intensifier was performed demonstrating a good reduction and excellent fixation without protrusion of the hardware in any plane (Figure 2).
Because of the resection of the tendon autograft reconstruction and shortening of the os trapezium, an instability of the joint was identified and the capsule was suture imbricated using an absorbable 3-0 Biosyn (Biosyn TM) for figure-of-eight sutures. To stabilize the joint, a cut down on the translation and a dorsal radial ligament reconstruction to prevent over-translation was made, leading to a stable joint when simulating the pinch. Furthermore, sutures between the reconstruction and the adjacent thenar muscles were performed using absorbable 3-0 Biosyn (Biosyn TM). The tourniquet was released, circulation was tested and hemostasis was assured with a bipolar cautery. Finally, the incision was closed using a 5-0 Nylon suture and sterile dressings were applied as well as a well-padded fiberglass splint protecting the reconstruction.
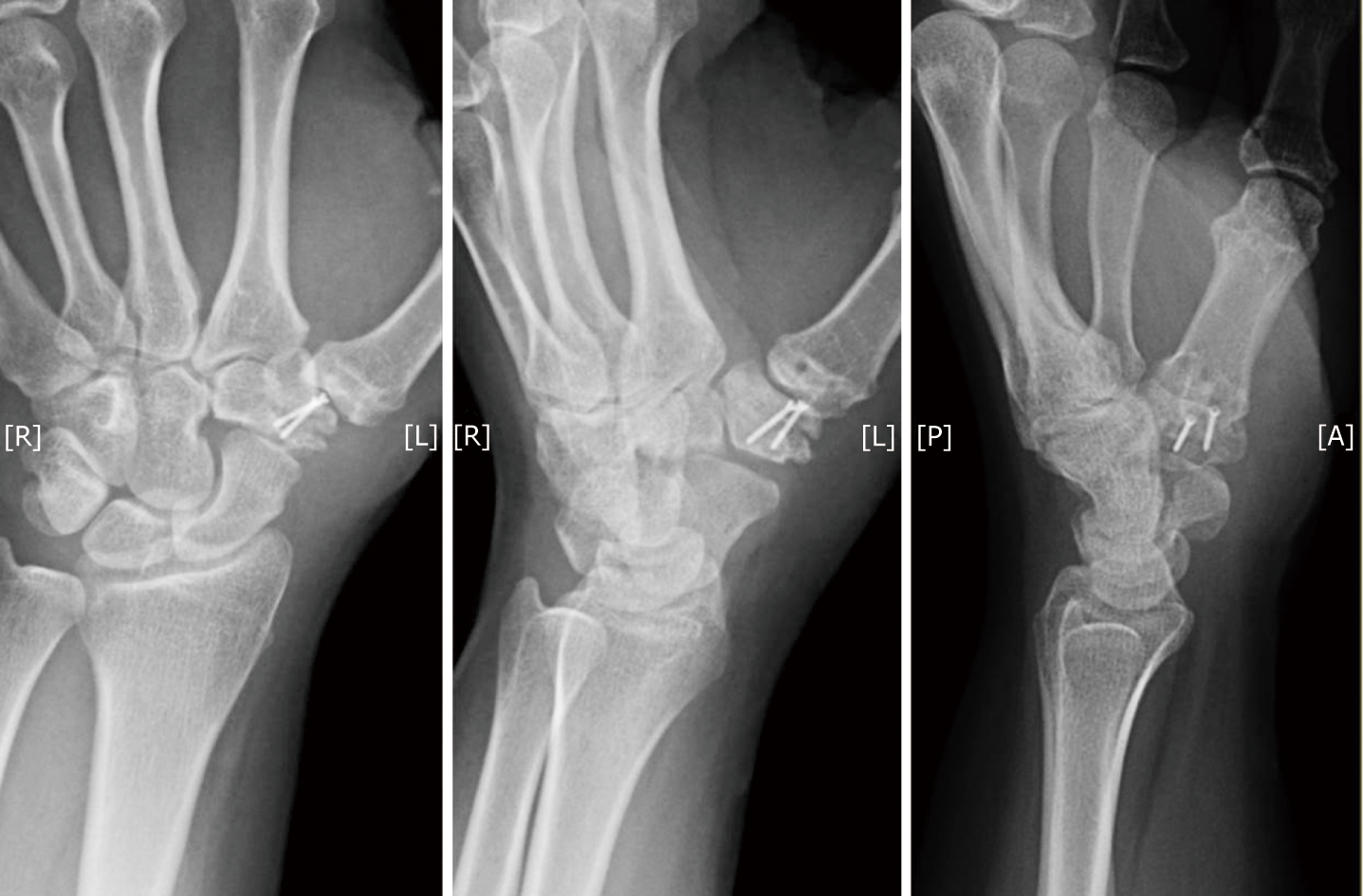
Some degree of basal joint arthritis with a stable trapeziometacarpal joint after subtraction hemiarthroplasty. Radiographs reveal healing of the osteochondral segment. The screws are in position and have not caused adjacent wear or symptoms. The patient has zero pain as well as excellent motion and function.
OUTCOME AND FOLLOW-UP
Clinical follow-up controls were performed after 1.5, 3, 6 and 10 wk. In the first follow-up, the patient reported very little pain. Half of the sutures were removed and the thumb was placed in a fiberglass thumb gauntlet splint. Another 10 days later (3 weeks post-op) the splint was removed and she began mobilizing it. The remaining sutures were removed and the wound was healed. The motion was already satisfactory with only minimal pain. The radiographs performed on that day showed that the screws were still in place and some bony healing of the osteotomy site. At 6 wk post-op, the motion was excellent and the thumb was entirely stable (Figure 3). Therefore, we decided to start occupational therapy and performed a final follow-up 10 wk after.
Three years after performing the subtraction hemiarthroplasty, the patient returned for a long-term follow-up visit. The patient reported no pain and had excellent range of motion of the thumb. The DASH score was a 5.8, with a VAS rating of 1 at rest, and 3 with activity. The range of motion and grip strength was similar to the unaffected side.
The carpometacarpal joint of the thumb is a saddle joint which allows movements in palmar abduction, adduction, flexion, extension, opposition and reposition. Each articular surface is concave in one direction and convex in the other[8]. The most common affected surface in osteoarthritis is the distal surface, which articulates with the volar “beak” of the thumb metacarpal, where the anterior oblique ligament of the trapezium inserts[9,10]. The trapezium consists of a deep groove for the flexor carpi radialis tendon on the palmar side. According to the literature, between 3 and 16 ligaments have been described to participate in the stabilization of the carpometacarpal joint[11]. The dorsoradial ligament seems to be very important, especially to prevent dorsal subluxation of the trapeziometacrapal joint, once the anterior oblique ligament is stripped off the volar cortex[12].
When loading the carpometacarpal joint in a healthy population a volar translation of the first carpometacarpal joint, internal rotation and flexion on the distal trapezial surface could be illustrated. In grasping objects, the metacarpal bone translates ulnar, combined with flexion and abduction relative to the distal trapezial surface; Likewise, extension couples with adduction[11,13].
The technique which we describe seems to alter the force acting on the distal surface of the os trapezium. However, due to insufficient reports in the literature, the exact mechanism cannot be outlined in detail. To our knowledge, no study or case report exists investigating the angle of the carpal bone, specifically the angle after performing the subtraction hemiarthroplasty. Intraoperatively, the articular surfaces of the first metacarpal and os trapezium were well-appearing, without any bare areas of bone or eburnation, which is prerequisite to perform a procedure like this. On the radiographs, a derogation of the radial side of the os trapezium can be identified after the subtraction hemiarthroplasty, which may reduce pain and improves functional outcome. To rebalance the joint, ligament tightening imbrication and dorsal radial ligament reconstruction are required. Meanwhile, preserving the articular cartilage allows one to maintain the complete range of motion with only a few limitations. This idea is similarly used in other techniques such as partial trapeziectomy, with or without interposition.
The subtraction hemiarthroplasty with ligament tightening imbrication and reconstruction of the radial ligament leads to excellent results in this case, even after failure of two prior surgeries. It enables full range of motion, free of pain, in the carpometacarpal joint. Based on this case report with long term follow up, further research should be performed, such as a case series in selected patients with good articular surfaces of the first metacarpal and os trapezium.
Our case presents a new technique to treat early stages of basal joint arthritis. Patients can present in severe, late stages of the disease in outpatient clinic where joint persevering surgeries are unlikely to succeed. These include partial or complete trapeziectomy, with or without reconstruction of the ligaments and tendon interposition, implant arthroplasty, spacers, interposition arthroplasty with resurfacing, or joint replacement. To our knowledge, this case is unique and describes the excellent long term functional outcome including full range of motion after joint preserving surgery – subtraction hemiarthroplasty – even after failure of two prior surgeries.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Musumeci G S-Editor: Gong ZM L-Editor: A E-Editor: Liu JH
| 1. | Wright TW, Thompson J, Conrad BP. Loading of the index metacarpal after trapezial and partial versus complete trapezoid resection. J Hand Surg Am. 2006;31:58-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19:340-341. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 339] [Cited by in F6Publishing: 327] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 3. | Baker RH, Al-Shukri J, Davis TR. Evidence-Based Medicine: Thumb Basal Joint Arthritis. Plast Reconstr Surg. 2017;139:256e-266e. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Lin JD, Karl JW, Strauch RJ. Trapeziometacarpal joint stability: the evolving importance of the dorsal ligaments. Clin Orthop Relat Res. 2014;472:1138-1145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Van Nortwick S, Berger A, Cheng R, Lee J, Ladd AL. Trapezial topography in thumb carpometacarpal arthritis. J Wrist Surg. 2013;2:263-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Wajon A, Vinycomb T, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2015;CD004631. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 7. | Arenas-Prat JM. Wagner approach for first carpometacarpal joint denervation. Tech Hand Up Extrem Surg. 2012;16:107-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Neumann DA, Bielefeld T. The carpometacarpal joint of the thumb: stability, deformity, and therapeutic intervention. J Orthop Sports Phys Ther. 2003;33:386-399. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 98] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Edmunds JO. Current concepts of the anatomy of the thumb trapeziometacarpal joint. J Hand Surg Am. 2011;36:170-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Komatsu I, Lubahn JD. Anatomy and Biomechanics of the Thumb Carpometacarpal Joint. Oper Tech Orthop. 2018;28:1-5. [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Ladd AL, Weiss AP, Crisco JJ, Hagert E, Wolf JM, Glickel SZ, Yao J. The thumb carpometacarpal joint: anatomy, hormones, and biomechanics. Instr Course Lect. 2013;62:165-179. [PubMed] [Cited in This Article: ] |
| 12. | Strauch RJ, Rosenwasser MP, Behrman MJ. A biomechanical assessment of ligaments preventing dorsoradial subluxation of the trapeziometacarpal joint. J Hand Surg Am. 1999;24:198-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Crisco JJ, Coburn JC, Moore DC, Akelman E, Weiss AP, Wolfe SW. In vivo radiocarpal kinematics and the dart thrower's motion. J Bone Joint Surg Am. 2005;87:2729-2740. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 130] [Article Influence: 6.8] [Reference Citation Analysis (0)] |