Published online Apr 18, 2019. doi: 10.5312/wjo.v10.i4.206
Peer-review started: January 4, 2019
First decision: January 26, 2019
Revised: February 18, 2019
Accepted: March 16, 2019
Article in press: March 16, 2019
Published online: April 18, 2019
Allograft interbody spacers are utilized during transforaminal lumbar interbody fusion (TLIF) to reestablish anterior column support and disc height. While the TLIF technique offers many improvements over previous surgical methods, instrumentation and bone graft-related complications such as spacer misplacement or migration, screw fracture or misplacement, or rod breakage continue to be reported. The objective of this manuscript is to report on a fractured allograft interbody spacer that displaced into the neural foramen and resulted in impingement on the exiting nerve root that required revision.
A 50-year-old male had two-level TLIF with immediate post-operative right L5 radiculopathy. Computed tomography scan demonstrated a fractured allograft interbody spacer that displaced into the right neural foramen and impinged on the exiting L5 nerve root. Revision surgery was performed to remove the broken allograft fragments from the right L5 foramen and the intact portion of the spacer was left in place. The right leg L5 radicular pain resolved. At the last follow up 12 mo after the index procedure, computed tomography scan confirmed sound interbody and posterolateral fusion.
Displacement of broken allograft interbody spacer following TLIF procedures can result in neurological sequelae that require revision. To avoid such an occurrence, the authors recommend allowing sufficient time for the reconstitution of the graft in saline prior to use to decrease brittleness, to use an impactor size that is as close as possible to the spacer size and meticulous inspection of the cortical allograft spacer for any visible imperfection prior to insertion.
Core tip: Allograft interbody spacers are commonly used in lumbar transforaminal lumbar interbody fusion procedures. A complication previously undocumented in the literature, we report on a fractured allograft interbody spacer that displaced into the neural foramen and resulted in impingement on the exiting nerve root that required revision. At 12 mo post-op, the patient was doing well with computed tomography scan confirming fusion and subsequent removal of the impinging fractured graft fragment. While presumably a rare occurrence, the authors review several technical points to avoid this complication.
- Citation: Kyle A, Rowland A, Stirton J, Elgafy H. Fracture of allograft interbody spacer resulting in post-operative radiculopathy: A case report. World J Orthop 2019; 10(4): 206-211
- URL: https://www.wjgnet.com/2218-5836/full/v10/i4/206.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i4.206
Transforaminal lumbar interbody fusion (TLIF) is a surgical technique that is utilized for lumbar pathologies for which segmental fusion is indicated[1-5]. This method was developed to improve upon previous surgical methods such as anterior or posterior lumbar interbody fusion. Its unilateral approach can reduce the risk of durotomy, nerve damage, or epidural fibrosis relative to posterior lumbar interbody fusion while decreasing incidence of vascular injury and procedure time relative to anterior lumbar interbody fusion[2,5,7].
Prosthetic allograft interbody spacers are utilized during TLIF procedures to restore anterior column support and disc height in patients with degenerative disc disease and spondylolisthesis[4,8-11]. The demineralized surface of the implant’s allogenic bone provides osteoconductivity to aid in osteogenesis and scaffolding for new bone formation along its surface and successful interbody arthrodesis[12,13].
Instrumentation or bone graft-related complications of the TLIF procedure typically involve graft misplacement or migration, screw fracture or misplacement, or rod breakage[14-21]. The authors report on a complication involving a fractured allograft spacer that displaced into the neural foramen impinging on the exiting nerve root during a two-level TLIF. Revision surgery was carried out to remove the broken allograft fragment from the right L5 foramen. To the best of the authors’ knowledge, a complication such as this has not been described in the literature.
A 50-year-old male who had previously undergone L5/S1 laminectomy, ins-trumentation and attempted posterolateral fusion presented to the clinic 2 years after this procedure with chronic low back pain and numbness/pain radiating down his right lower extremity, and to a lesser degree the left lower extremity.
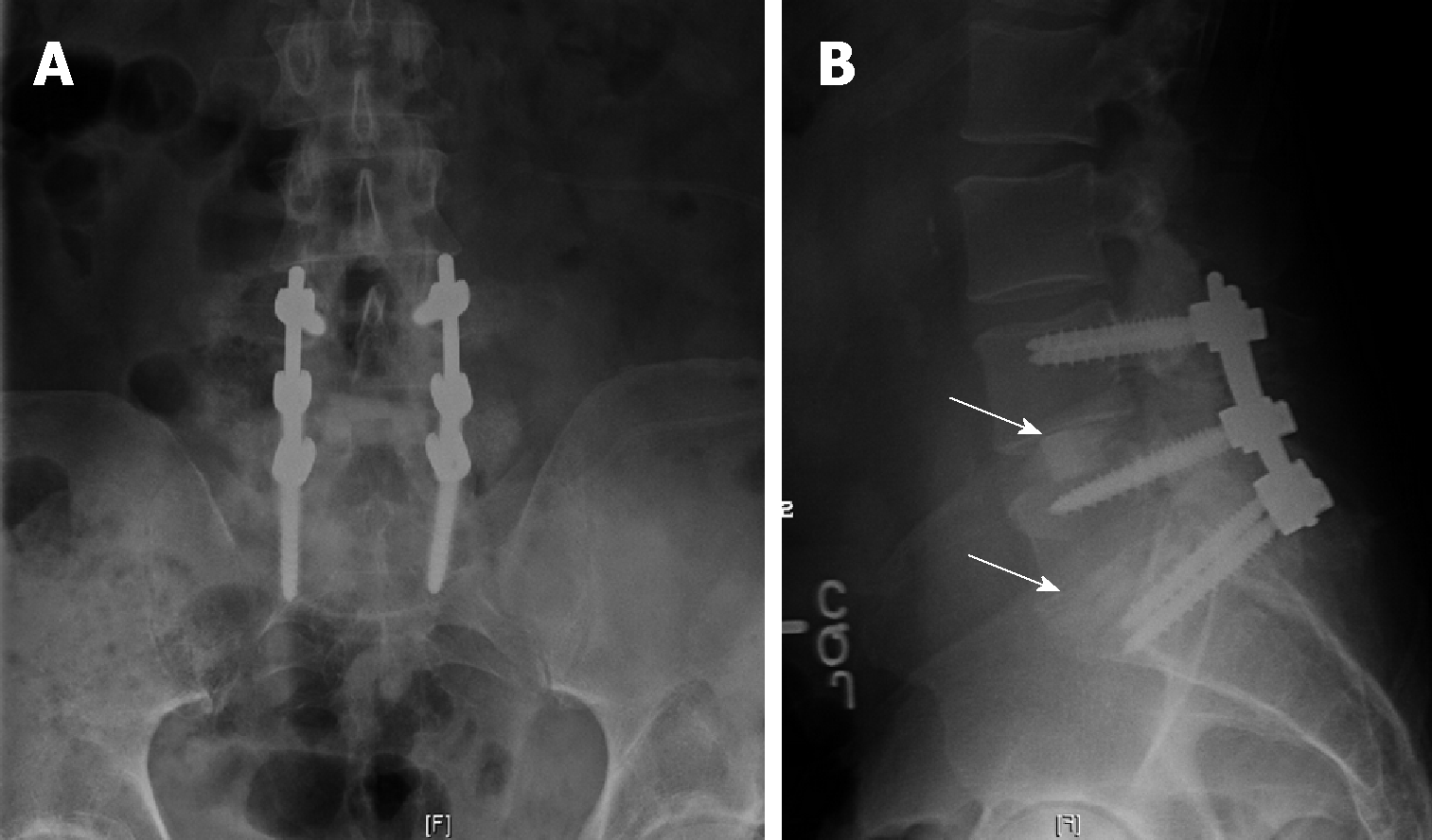
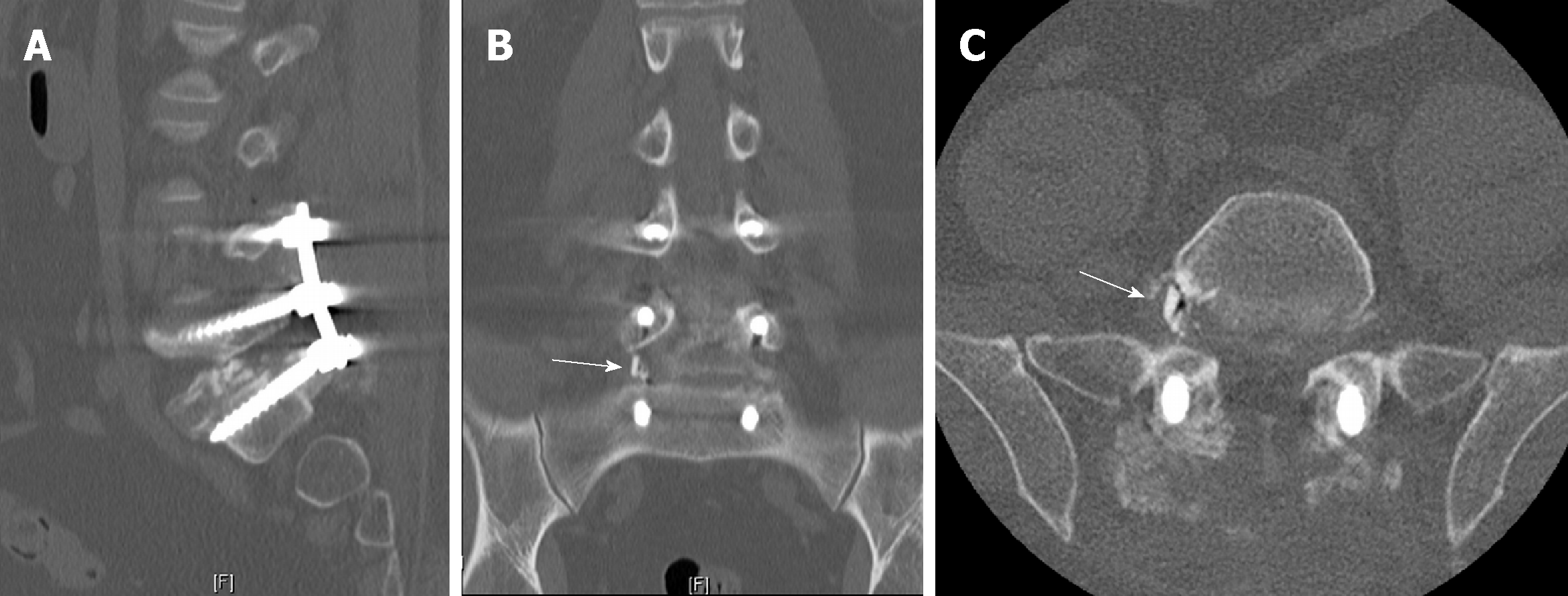
Computed tomography scan and magnetic resonance imaging confirmed L5/S1 nonunion with hardware loosening and adjacent segment disc degeneration and spinal stenosis. Risks, benefits, and alternative management were discussed and the patient elected to proceed with hardware removal, L4/5 decompression using a right-sided approach, and L4-S1 TLIF and posterior spinal fusion with iliac crest autograft. The procedure was carried out as planned with an allograft interbody spacer impacted into the anterior half of the disk space at both the L4/5 and L5/S1 levels without any obvious intraoperative complication. Soon after awaking from anesthesia, the patient began complaining of right leg radiculopathy along the L5 dermatome. Plain films (Figure 1A and B) showed no obvious complication. Computed tomography scan was then obtained which revealed allograft spacer fracture with fragment displacement into the right L5 neural foramen (Figure 2A-C).
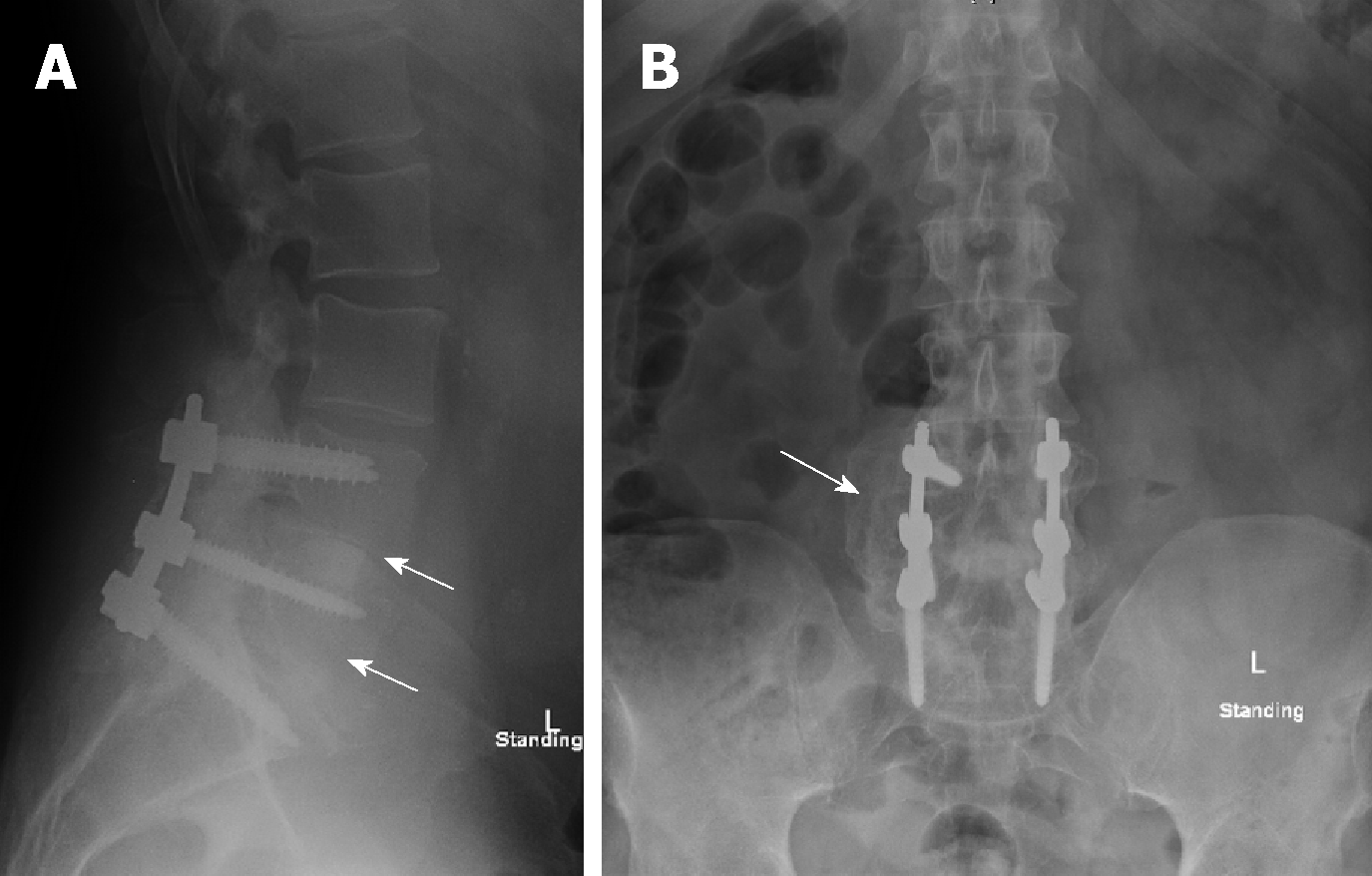
The patient was subsequently taken back to the operating room for revision. The broken allograft pieces were identified and extracted (Figure 3). The intact portion of the allograft interbody spacer was left in place. Immediately following the procedure the patient’s pain improved, and he was discharged home on post-operative day 2.
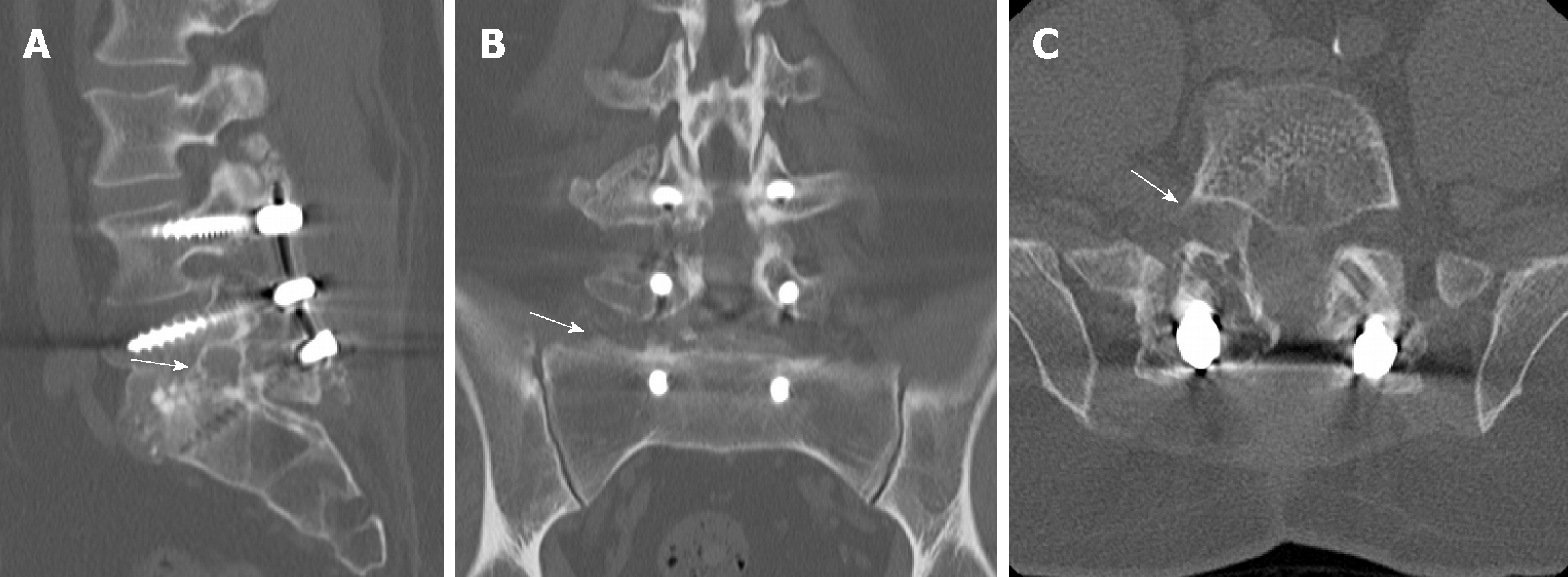
Over subsequent clinic visits, right leg L5 radicular pain resolved, and in the last follow-up 12 mo after the index procedure computed tomography scan confirmed sound interbody and posterolateral fusion with no foraminal bone fragment or stenosis (Figure 4A and B, and Figure 5A-C).
Complications resulting from the interbody fusion procedures have been well reported since the technique was first described by Harms et al[22] in 1982. These complications, however, have typically involved infection, durotomy, bleeding, malpositioned hardware, or pseudoarthrosis[5,11,17,19,21]. Hardware failure reports have been limited to interbody device migration/subsidence, screw fracture, or rod breakage[18,20,23-25]. Saville et al[26] showed that when a posterior lumbar interbody fusion spacer is compressed, failure is observed by subsidence of the graft into the upper or lower vertebral bodies and never internally within the graft itself. There have been case studies reporting vertebral fracture following TLIF procedures that may have resulted from the implantation process itself[26].
The interbody fusion technique involves using vertebral endplate shavers to prepare the disc for the fusion. The graft size is determined using trial spacers. Starting with a smaller size trial spacer and under lateral view fluoroscopic guidance, the trial spacer is gradually increased until the most secure fit is achieved, and then selected for the corresponding graft size. The current case reported is unique as part of the graft was sheared off, which resulted in fractured pieces migrating to the right L5-S1 neural foramen, compressing the exiting nerve root, and resulting in right L5 radiculopathy. The remaining bulk of the interbody spacer remained intact and well positioned. No damage to the vertebral bodies was noted.
According to Janssen et al[27], allograft spacers have been tested to withstand 25000 N of force compared to the compressive strength of a vertebral body itself as 8000 N. This assumes that the compressive strength of the spacer was equally distributed across the surface of the spacer, as opposed to a localized force applied to a portion of the spacer. As the patient experienced a limited axial load on his vertebrae following surgery, it is unlikely the fracture of the spacer occurred post-operatively. No reports were found of the surgeons experiencing significant difficulty or resistance during the insertion of allograft interbody spacers. Typically, a trial spacer is used to determine appropriate spacer size to achieve good vertebral body distraction and press-fit placement prior to inserting the interbody device. This makes it less likely that a poor interbody spacer size choice can explain the resulting fractured spacer. A system-specific insertion tool was used to implant the spacer decreasing the chance of damage occurring during graft insertion.
There are reports of bone allograft fracture in orthopedic surgery, such as after bone tumor resection. Aponte-Tinao et al[28] reported fractured allografts in 19 out of 135 (14%) patients with segmental intercalary bone allograft reconstruction of the lower extremity. The kidney shaped allograft spacer used in the current report is freeze-dried. It is recommended by the manufacturer to reconstitute the graft in saline prior to use to decrease brittleness. After preparation of the disc space, the allograft spacer is inserted into the space with an implant holder, and then an impactor is used to fully seat the spacer into the intervertebral disc space. Possible causes for graft breakage could be one or a combination of the following: insufficient reconstitution of the graft prior to insertion, the impactor used to seat the graft is smaller than the spacer that may lead to shearing of part of the spacer, or the spacer was microscopically cracked prior to its insertion resulting in the graft weakening and breaking.
Displacement of broken allograft interbody spacer following TLIF procedures can result in neurological sequelae that require revision. Though this complication was found during a TLIF procedure, any lumbar interbody fusion technique is subject to this complication in the event a prosthetic allograft spacer is used. To avoid such an occurrence, the authors recommend allowing sufficient time for the reconstitution of the graft in saline prior to use to decrease brittleness, to use an impactor size that is as close as possible to the spacer size and meticulous inspection of the cortical allograft spacer for any visible imperfection prior to insertion.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Emara KM, Malik H S-Editor: Wang JL L-Editor: Filipodia E-Editor: Wu YXJ
| 1. | Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1:2-18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 352] [Reference Citation Analysis (0)] |
| 2. | Derman PB, Albert TJ. Interbody Fusion Techniques in the Surgical Management of Degenerative Lumbar Spondylolisthesis. Curr Rev Musculoskelet Med. 2017;10:530-538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Hee HT, Castro FP, Majd ME, Holt RT, Myers L. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord. 2001;14:533-540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002;33:359-366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 108] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion--systematic review and meta-analysis. Br J Neurosurg. 2015;29:705-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 137] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 6. | Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW, Kuklo TR. Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech. 2005;18:337-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 191] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 7. | Cutler AR, Siddiqui S, Mohan AL, Hillard VH, Cerabona F, Das K. Comparison of polyetheretherketone cages with femoral cortical bone allograft as a single-piece interbody spacer in transforaminal lumbar interbody fusion. J Neurosurg Spine. 2006;5:534-539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Syed H, Voyadzis JM. True Percutaneous Transforaminal Lumbar Interbody Fusion: Case Illustrations, Surgical Technique, and Limitations. J Neurol Surg A Cent Eur Neurosurg. 2016;77:344-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Xiao YX, Chen QX, Li FC. Unilateral transforaminal lumbar interbody fusion: a review of the technique, indications and graft materials. J Int Med Res. 2009;37:908-917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Tallarico RA, Lavelle WF, J Bianco A, Taormina JL, Ordway NR. Positional effects of transforaminal interbody spacer placement at the L5-S1 intervertebral disc space: a biomechanical study. Spine J. 2014;14:3018-3024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Heim SE, Abitbol JJ. Complications and strategies for salvage of intervertebral fixation devices. Orthop Clin North Am. 2002;33:393-402, vii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Gupta A, Kukkar N, Sharif K, Main BJ, Albers CE, El-Amin Iii SF. Bone graft substitutes for spine fusion: A brief review. World J Orthop. 2015;6:449-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 72] [Cited by in F6Publishing: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 13. | Beaman FD, Bancroft LW, Peterson JJ, Kransdorf MJ, Menke DM, DeOrio JK. Imaging characteristics of bone graft materials. Radiographics. 2006;26:373-388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Liang Y, Shi W, Jiang C, Chen Z, Liu F, Feng Z, Jiang X. Clinical outcomes and sagittal alignment of single-level unilateral instrumented transforaminal lumbar interbody fusion with a 4 to 5-year follow-up. Eur Spine J. 2015;24:2560-2566. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Leute PJ, Hammad A, Hoffmann I, Hoppe S, Klinger HM, Lakemeier S. Set screw fracture with cage dislocation after two-level transforaminal lumbar interbody fusion (TLIF): a case report. J Med Case Rep. 2015;9:22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Pan FM, Wang SJ, Yong ZY, Liu XM, Huang YF, Wu DS. Risk factors for cage retropulsion after lumbar interbody fusion surgery: Series of cases and literature review. Int J Surg. 2016;30:56-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Hu W, Tang J, Wu X, Zhang L, Ke B. Minimally invasive versus open transforaminal lumbar fusion: a systematic review of complications. Int Orthop. 2016;40:1883-1890. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Tormenti MJ, Maserati MB, Bonfield CM, Gerszten PC, Moossy JJ, Kanter AS, Spiro RM, Okonkwo DO. Perioperative surgical complications of transforaminal lumbar interbody fusion: a single-center experience. J Neurosurg Spine. 2012;16:44-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Joseph JR, Smith BW, La Marca F, Park P. Comparison of complication rates of minimally invasive transforaminal lumbar interbody fusion and lateral lumbar interbody fusion: a systematic review of the literature. Neurosurg Focus. 2015;39:E4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 20. | Smith AJ, Arginteanu M, Moore F, Steinberger A, Camins M. Increased incidence of cage migration and nonunion in instrumented transforaminal lumbar interbody fusion with bioabsorbable cages. J Neurosurg Spine. 2010;13:388-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Wong AP, Smith ZA, Stadler JA, Hu XY, Yan JZ, Li XF, Lee JH, Khoo LT. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am. 2014;25:279-304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 22. | Harms J, Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl)]. Z Orthop Ihre Grenzgeb. 1982;120:343-347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 303] [Cited by in F6Publishing: 297] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 23. | Villavicencio AT, Nelson EL, Rajpal S, Otalora F, Burneikiene S. Case Series of Anterior Intervertebral Graft Extrusions in Transforaminal Lumbar Interbody Fusion Surgeries. World Neurosurg. 2016;85:130-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Stein IC, Than KD, Chen KS, Wang AC, Park P. Failure of a polyether-ether-ketone expandable interbody cage following transforaminal lumbar interbody fusion. Eur Spine J. 2015;24 Suppl 4:S555-S559. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Kim PD, Baron EM, Levesque M. Extrusion of expandable stacked interbody device for lumbar fusion: case report of a complication. Spine (Phila Pa 1976). 2012;37:E1155-E1158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Saville PA, Anari JB, Smith HE, Arlet V. Vertebral body fracture after TLIF: a new complication. Eur Spine J. 2016;25 Suppl 1:230-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Janssen ME, Lam C, Beckham R. Outcomes of allogenic cages in anterior and posterior lumbar interbody fusion. Eur Spine J. 2001;10 Suppl 2:S158-S168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Aponte-Tinao LA, Ayerza MA, Muscolo DL, Farfalli GL. Should fractures in massive intercalary bone allografts of the lower limb be treated with ORIF or with a new allograft? Clin Orthop Relat Res. 2015;473:805-811. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |